CASE REVIEW
Dapagliflozin reduces ESKD risk in geriatric CKD patients with comorbidities: A local case sharing
The prevalence of chronic kidney disease (CKD) among the elderly population is on the rise.1,2 The incidence of advanced-stageCKD increased sharply with advancing age.3 When compared with the younger counterparts, older patients with advanced CKD are more likely to be intolerable to conventional therapies, such as angiotensin-converting enzyme inhibitors (ACEis)or angiotensin receptor blockers (ARBs).2,3 In 2021, dapagliflozin was approved for the treatment of patients regardless of type 2 diabetes (T2D), providing an additional treatment option to address the medical gap in the local CKD management.4In an interview with Omnihealth Practice, Dr. Shea, Tat-Mingshared 2 clinical cases of patients aged >80 years with stage 3/4 CKD having multiple comorbidities, in whom dapagliflozin stabilized their estimated glomerular filtration rate (eGFR)and halted CKD progression. Dr. Shea also discussed the clinical data of dapagliflozin and provided practical tips to optimize treatment outcomes in the elderly CKD population.
Background
Unmet medical needs in elderly patients with CKD
The prevalence of CKD is rising, especially in the elderly.1 It is estimated that the eGFR progressively declines at an average rate of 8mL/min/1.73m2 every 10 years beyond the age of 30. Comparing to patients with normal renal function, CKD patients have a higher risk of death, cardiovascular (CV) events, hospitalization, as well as impaired quality of life.5 In the absence of timely and effective intervention, the condition will eventually progress to end-stage kidney disease (ESKD), which requires dialysis or renal transplantation in order to sustain the patients’ life.2
In the past, CKD patients were managed with ACEis or ARBs, given the benefits of reducing proteinuria and delaying disease progression.2 However, significant residual renal risk remains. On the other hand, vulnerable elderly patients are more prone to the adverse events (AEs), particularly hyperkalemia and hypotension, arising from the use of these medications.6 In real-life practice, the treatment persistence of ACEi/ARB is limited in patients with advanced CKD in whom dosage adjustment and even treatment discontinuation might be required.5 Thus, the risk and benefit balance of ACEis and ARBs must be carefully evaluated in this population. An additional treatment option is needed for CKD patients to preserve renal function and delay disease progression.
Dapagliflozin advances the treatment landscape of CKD with or without T2D
Dapagliflozin is a sodium-glucose co-transporter 2 inhibitor (SGLT2i) which lowers blood glucose concentration in adults with T2D by increasing urinary glucose excretion.7 Multiple clinical benefits beyond glucose lowering with dapagliflozin have been demonstrated in various clinical trials, including improvement in CV outcomes, and very recently, risk reduction in renal outcomes.8,9 Yet, concerns have been heightened on the use of SGLT2is, including dapagliflozin, that they might increase the risk of hypoglycemia among older patients with CKD.9
DAPA-CKD was a randomized, double-blind, placebo-controlled, multicenter trial dedicated to assess the renal outcomes of dapagliflozinin CKD patients with or without T2D.9 A total of 4,304 patients regardless of T2D and with an eGFR of 25-75mL/min/1.73m2 and urine albumin-creatinine ratio (UACR) of 200mg/g-5,000mg/g were enrolled.9 All patients received a stable dose of ACEis/ARBs as background therapy.9
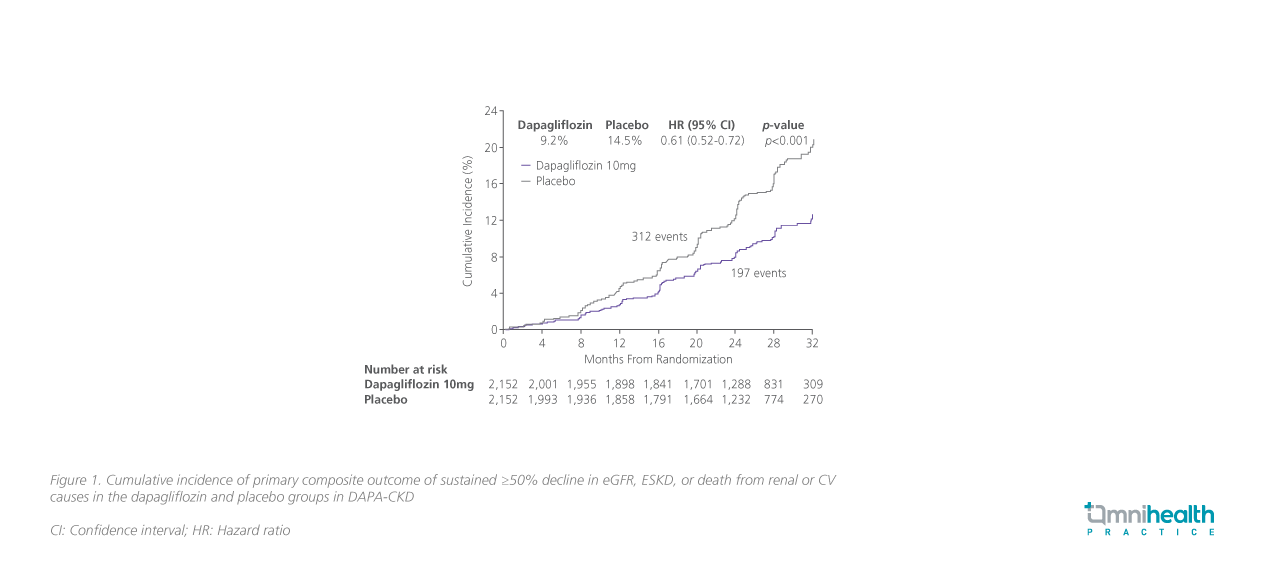
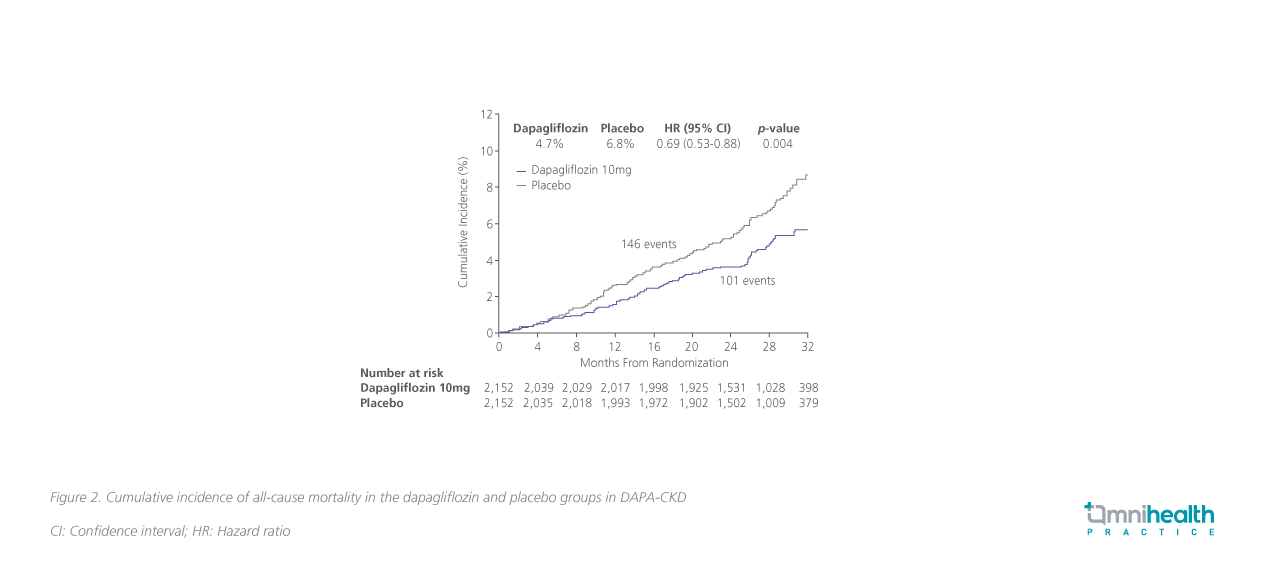
After a median follow-up of 2.4 years, results showed that dapagliflozin significantly reduced the risk of the primary composite outcome of sustained ≥50% decline in eGFR, ESKD, or death from renal or CV causes among CKD patients with a relative risk reduction of 39% (HR=0.61; 95% CI: 0.51-0.72; p<0.001)(figure 1).9 Regarding all-cause mortality, a secondary outcome ofDAPA-CKD, dapagliflozin achieved a 31% relative risk reduction vs. placebo (HR=0.69; 95% CI: 0.53-0.88; p=0.004) (figure 2).9 The incidences of AEs of dapagliflozin were similar to those in the placebo group.9 The rate of major hypoglycemia in the dapagliflozin group was lower than that in placebo group, and there were no hypoglycemic episodes in patients without diabetes.9,10
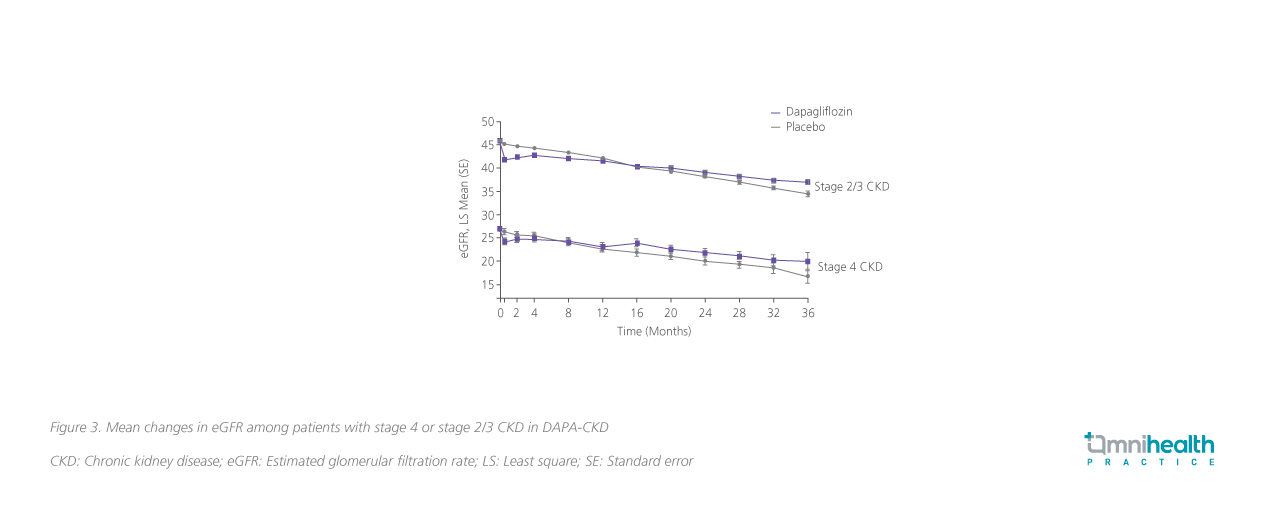
The clinical efficacy of dapagliflozin in stage 4 CKD patients was demonstrated in a post-hoc analysis of DAPA-CKD.5 Regarding the effects on the eGFR slopes, dapagliflozin attenuated progressive decline of eGFR in patients with stage 4 CKD and achieved a between-groups difference of 1.23mL/min/1.73m2 per year(95% CI: 0.36-2.09; p=0.005) vs. placebo, which was consistent with the effect among patients with stage 2/3 CKD (pinteraction=0.48)(figure 3).5 Overall, stage 4 CKD patients tolerated dapagliflozin well.5 The rates of serious AEs or AEs of interest, including renal-relatedAEs, major hypoglycemia or volume depletion, were also similar among patients treated with placebo.5
Based on the positive findings, the 2022 consensus by the American Diabetes Association (ADA) and Kidney Disease: Improving Global Outcomes (KDIGO) recommends the use ofSGLT2is, including dapagliflozin, as a first-line pharmacological treatment for diabetic kidney disease (DKD).11 Considering the therapeutic benefits and high tolerability, dapagliflozin has been proven to be a favorable treatment option for older CKD patients.5,8,9
Case report
Case 1: The effect of dapagliflozin in a stage 4 CKD elderly patient with comorbidities
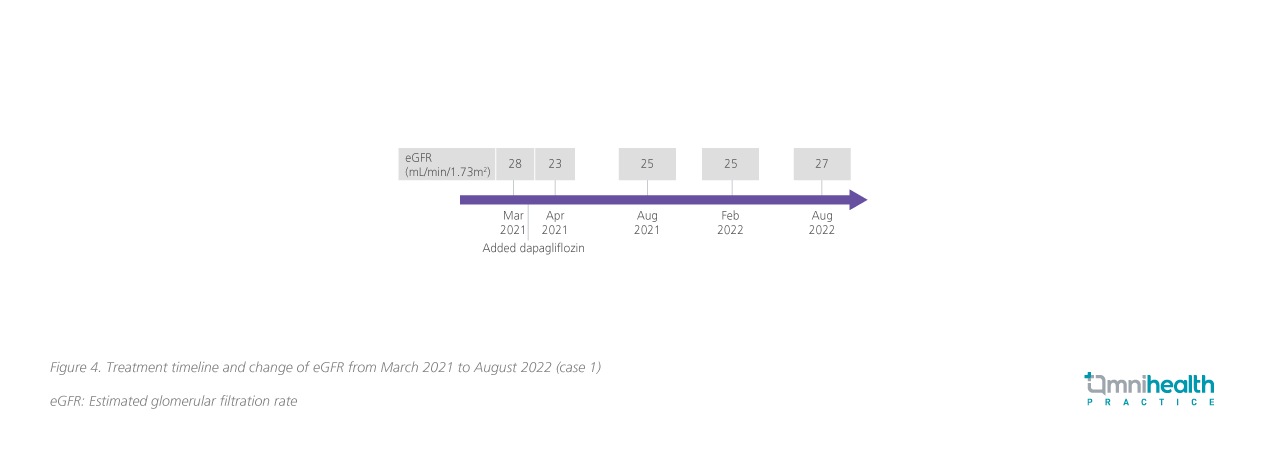
An 83-year-old lady with hypertension, hyperlipidemia and T2D was referred to Dr. Shea in March 2021 due to her persistently reduced eGFR down to 28mL/min/1.73m2, which suggested to be stage 4 CKD. Her family members were concerned about the possible necessity of dialysis in the future and wished to stabilize her renal function as soon as possible to prevent the disease from progressing to ESKD. Over the past few years, the patient has been treated with metformin and sulfonylurea for T2D; and ARB for hypertension and CKD. Although her blood pressure and glucose were well controlled, there was no improvement in renal function despite the use of an ARB.
The patient was started on dapagliflozin on her first visit, while sulfonylurea was stopped; and the dose of metformin was reduced, while losartan was replaced with telmisartan. Dr. Sheareminded that both metformin and dapagliflozin are associated with weight loss, and that it is imperative to monitor the patient’s weight regularly to avoid getting underweight.
During the first 4 weeks of treatment with dapagliflozin, the patient’s eGFR dropped to 23mL/min/1.73m2. Her eGFR started to stabilize after 4 weeks of treatment, with the eGFR increased back to 27mL/min/1.73m2, which has been sustained for more than 1.5 years as of her last visit in September 2022 (figure 4). Throughout the treatment course, the patient's glycated hemoglobin (HbA1c)level remained stable at around 6.1%-6.3%. Overall, dapagliflozin was well tolerated by this patient, and no AE was reported.
Case 2: Dapagliflozin in an elderly CKD patient with multi-morbidities
An 87-year-old, functionally independent, overweight lady had a past medical history of hypertension, hypercholesterolemia, hyperuricemia, multiple minor strokes, congestive heart failure, gout, T2D, depression, osteoporosis, insomnia, dementia, and rapid eye movement (REM) sleep disorder. With these multiple comorbidities, she had been treating with 14 medications. In 2015, her eGFR was 53mL/min/1.73m2 (i.e., stage 3 CKD), and was treated with irbesartan for her hypertension. In 2018, the issue of getting overweight with this patient became worse, with her body mass index (BMI) reaching 30.8kg/m2. Dapagliflozin was started for further control on T2D in early 2018, before it was approved as CKD treatment. The patient's overweight issue improved during the first 4 months of treatment, with eGFR of 51mL/min/1.73m2. Over 3 years of treatment, Dr. Shea was surprised that the patient’s eGFR started to rebound and increase gradually to 61mL/min/1.73m2 in 2021, which has been sustained as of today (figure 5). The patient tolerated the drug well with no reports of AEs.

Discussion
Undoubtedly, the management of CKD in geriatric patients poses a tremendous challenge to clinicians. Geriatric issues such as frailty and comorbidities, especially diabetes and hypertension, must be considered when planning the management of CKD in this population. In DAPA-CKD, dapagliflozin demonstrated remarkable efficacy in stabilizing eGFR and delaying ESKD among CKD patients, including those who were older and with advanced-stage of CKD. As demonstrated in the first case, the renal function of the elderly patient was deteriorating and progressed to stage 4CKD. The use of ARB was unable to slow down the decline in kidney function. Dapagliflozin was added on top of an ARB to further preserve renal function. Over 1.5 years of treatment, the patient’s eGFR was stabilized without AEs. The approval of dapagliflozin provides a new treatment option for the CKD management, which helps further reduce renal risks and preserve kidney function.
The second case demonstrated that dapagliflozin provided extrarenal benefits beyond glucose lowering with eGFR rebounded from 51mL/min/1.73m2 to 61mL/min/1.73m2, which exceeded Dr. Shea’sexpectation. Moreover, Dr. Shea mentioned that elderly patients often have multiple comorbidities and are more prone to AEs arising from the medications, posing challenges to physicians in the CKD management in geriatric patients. “Even though the elderly patients are with poor renal function, multiple comorbidities and on numerous medications, dapagliflozin still demonstrates safety and efficacy, ”Dr. Shea said.
In Dr. Shea’s point of view, weight control is crucial for maintaining geriatric patients’ functional independence. Clinicians should ensure that sufficient nutrients are provided to strengthen patients’ muscles so that they would not become too frail. For T2D patients, he reminded that when adding dapagliflozin, the dose of antidiabetic drugs associated with weight loss such as metformin should be adjusted accordingly. In addition, it is necessary to monitor theweight of patients on a regular basis to prevent them from getting underweight.
Furthermore, Dr. Shea reckoned that there is a need to remind older CKD patients treated with SGLT2is of the possible occurrence ofurogenital infections. They should be encouraged to maintain basic hygiene and seek medical attention when symptoms of candidiasis develop. However, these infections are generally mild-to-moderate and can be managed effectively with standard treatment. Dose interruption or treatment discontinuation is not generally required, unless there is persistent infection.
Conclusion
In summary, dapagliflozin attenuated CKD progression and reduced the risk of ESKD, as demonstrated in the clinical trials. Local experiences showed that dapagliflozin is safe to use in geriatric patients with stage 4 CKD or with multiple comorbidities despite being frailer. The availability of dapagliflozin addresses the medical gap in the local CKD management among the elderly population, especially when the use of ACEis or ARBs still poses a significant residual renal risk of disease progression and may be inappropriate in patients with low blood pressure or those experiencing hyperkalemia.

