Cardio-kidney-metabolic (CKM) diseases often coexist in patients and are intimately linked with one another.1 Chronic kidney disease (CKD), heart failure (HF) and type 2 diabetes mellitus (T2D) form a triad of CKM conditions with major comorbidity, leading to compounded adverse outcomes.1 In a recent webinar, Dr. Janaka Karalliedde from Guy’s and St Thomas’ Hospital, King’s College London, the United Kingdom, highlighted the importance of checking for all three CKM conditions whenever one is presented and that early diagnosis and treatment with sodium-glucose cotransporter 2 inhibitors (SGLT2is) such as empagliflozin are essential in preventing the progression of these CKM conditions. Not only has empagliflozin shown efficacy in the management of T2D, it has also extended its benefits in mitigating cardiovascular (CV) and mortality risks and preserving kidney function.
Interconnectivity of the CKM system
Interactions between the heart, kidneys, and the metabolic system are complex and multifactorial, and CKM diseases contribute to the cycle of organ damage and dysfunction.1 Chronic diseases such as T2D lead to inflammation and increased oxidative stress which feed into organ damage through a complex combination of neurohormonal feedback mechanisms.1 Organ damage is facilitated by compensatory mechanisms and renin-angiotensin-aldosterone system (RAAS) activation which feeds into the cycle of organ damage in both the kidneys and the heart leading to conditions of CKD and HF.1 Dr. Karalliedde emphasized that it is important to recognize that many patients do not experience a singular disease, but rather a combination of multiple conditions.
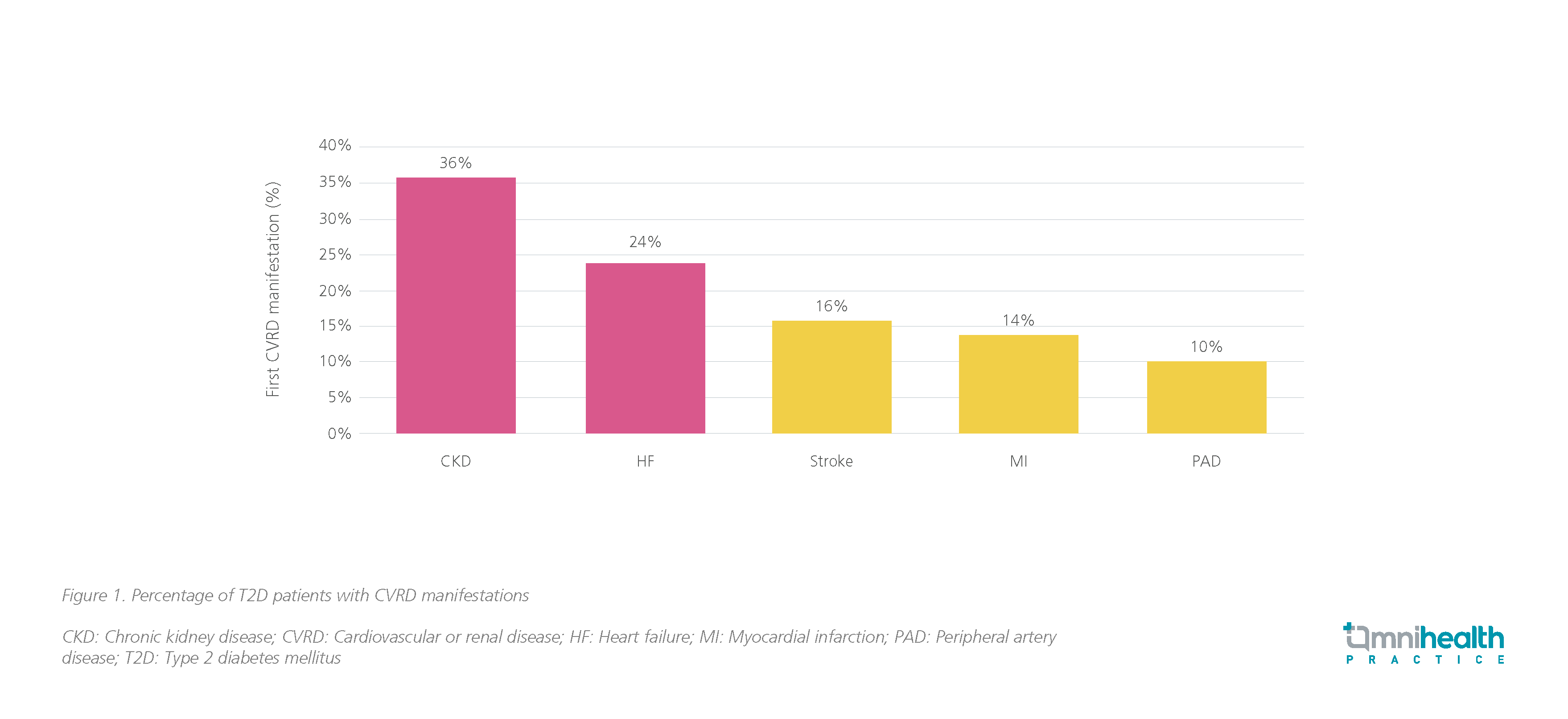
For instance, approximately 60% of individuals with CKD suffer from CV diseases, a stark contrast to the 5.8% observed in patients without CKD.2 Similarly, 50% of patients with T2D also suffer from CKD and 16% of HF patients are comorbid with all 3 conditions.2,3 Even among T2D patients with well-controlled glucose levels, HF and CKD are very common.4 In a large multinational cohort study in patients with T2D (n=772,336), 36% of the first cardiorenal disease manifestations were CKD and 24% were HF (figure 1).4
Recognizing the value of uACR assessment outside of renal function decline
Among the CKM condition triad, Dr. Karalliedde highlighted the burden of CKD which is often described as a silent killer since patients typically do not exhibit noticeable early symptoms. However, despite its prevalence in the T2D population, almost 90% of any stage CKD remains undiagnosed.5 The 2024 Kidney Disease Improving Global Outcomes (KDIGO) Clinical Practice Guidelines for the Evaluation and Management of Chronic Kidney Disease classified CKD based on the cause, GFR category and albuminuria category.6 Treatment is recommended with either elevated eGFR or uACR.6 However, by the time patients are diagnosed with CKD based on a low estimated glomerular filtration rate (eGFR), it is often too late as irreversible damage to the nephrons has already occurred, leaving limited opportunities for damage prevention.5 To improve the effectiveness of screening, it was reminded that the urine albumin-creatinine ratio (uACR) may be a useful indicator for early detection as it often rises before the eGFR drops.7 Dr. Karalliedde stated that for T2D patients who are also at risk of developing diabetic kidney diseases (DKD), uACR measurements are not merely a renal function test, but also serve to assess their CV health and overall mortality risk, adding that “When I talk to my patients, I say we are not doing just another urine test, we are doing a kidney and heart test. By telling your patient why this is important, they are more likely to bring that sample back.”
Elevating kidney health with empagliflozin including patients with DKD
Dr. Karalliedde claimed that in the last 2 decades, there had been no new treatments developed specifically for the management of DKD prior to the SGLT2is. In recent years, SGLT2is such as empagliflozin have emerged, showing benefits across the board not only in T2D and heart diseases but also in improving renal outcomes.
Data from the EMPA-REG OUTCOME highlighted the renal outcomes in T2D populations.8,9 In this trial, empagliflozin was shown to significantly reduce the risk of incident or worsening nephropathy by 39% (HR=0.61; 95% CI: 0.53-0.70).8 When considering a subgroup analysis in the population with DKD, the benefit was even more pronounced.9 Patients with baseline overt DKD, defined by a uACR>300mg/g with any eGFR at baseline, had a 60% risk reduction (HR=0.40; 95% CI: 0.21-0.77) in composite kidney endpoints which consisted of eGFR<15mL/min/1.73m2, sustained doubling of serum creatinine from baseline, initiation of kidney replacement therapy or kidney death.9 Patients with non-overt DKD, defined as eGFR<60mL/min/1.73m2 with UACR≤300mg/g, had a 47% risk reduction (HR=0.53; 95% CI: 0.42-0.67) in incident or worsening neuropathy as well.9
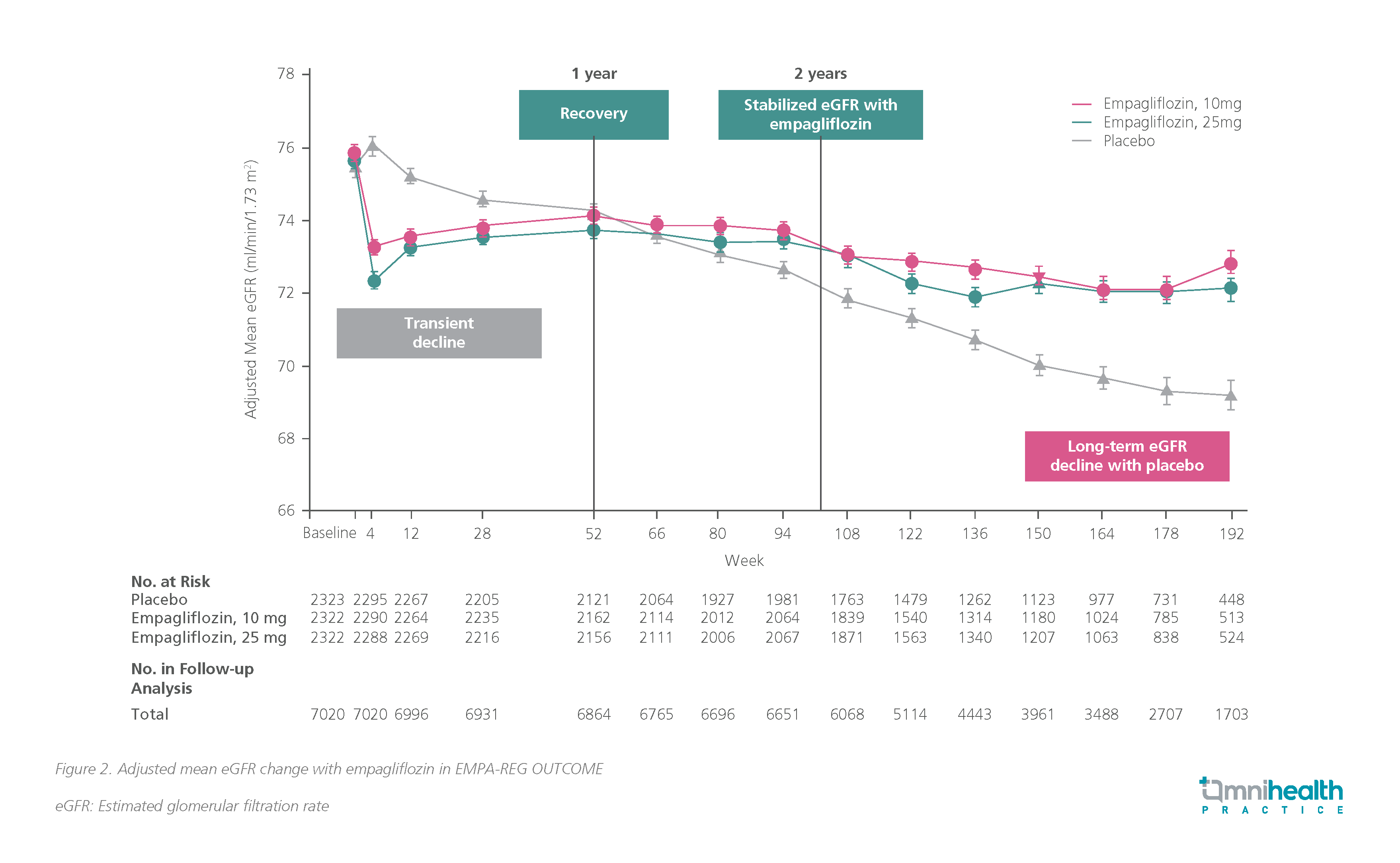
Empagliflozin was also demonstrated to slow the progression of renal function decline.8 Despite a transient decline in eGFR at initiation, it was stabilized at year 2 and showed smaller decline over the long term compared with the placebo (figure 2).8
Similarly, in patients across the HF spectrum in the EMPEROR-Preserved and EMPEROR-Reduced studies, the rate of eGFR decline was 1.73mL/min/1.73m2 lower (p<0.001) with empagliflozin in the HFrEF population and 1.37mL/min/1.73m2 lower (p<0.001) with empagliflozin in the HFpEF population.10,11
CV benefits of empagliflozin in the CKM populations
He further asserted that whilst many SGLT2is have demonstrated improvements in CV and renal outcomes in clinical trials, only empagliflozin has shown beneficial effects on CV mortality and all-cause mortality in patients with T2D. In the EMPA-REG OUTCOME study, significant reductions in all-cause mortality (HR=0.68; 95% CI: 0.57-0.82; p<0.001), hospitalization for heart failure (HR=0.65; 95% CI: 0.50-0.85; p=0.002), and death from CV causes, non-fatal myocardial infarction, or non-fatal stroke (HR=0.86; 5% CI: 0.74-0.99; p<0.001) were reported in populations with comorbid T2D.12 Data from the subgroup analysis of patients with DKD in EMPA-REG OUTCOME also showed that empagliflozin reduced the risk of CV mortality by 29% (HR=0.71; 95% CI: 0.52-0.98).13
Furthermore, both the EMPEROR-Preserved and the EMPEROR-Reduced studies met their key endpoints in preventing cardiovascular death and hospitalization for HF with 25% (HR=0.75; 95% CI: 0.65-0.86; p<0.001) and 21% (HR=0.79; 95% CI: 0.69-0.90; p<0.001) risk reduction respectively.10,11 Hence, Dr. Karalliedde advised that the sooner we treat the patients with empagliflozin, the better and the greater the heart and kidneys are protected.
Practical clinical considerations of SGLT2i therapy
Dr. Karalliedde highlighted that most patients with CKM conditions should be automatically considered for SGLT2is like empagliflozin. When empagliflozin is initiated early in primary care, it can potentially delay a maximum of 27 years according to data on chronic eGFR slopes, but the benefit is somewhat diminished when empagliflozin is initiated later in the disease course.14 Therefore, early intervention is key to getting the greatest benefit from empagliflozin and slowing the decline in kidney function.14 Hence, Dr. Karalliedde maintained that primary care physicians should identify and treat DKD as early as possible and delay the progression and the irreversible loss of nephrons. By improving the patient’s HbA1c, reducing the risk of hypoglycemia and reducing body weight with drugs like empagliflozin, quality-adjusted life years (QALYs) increase which signifies a better quality of life for patients.15
Dr. Karalliedde noted that prescription of SGLT2is may not be appropriate in certain patient populations, such as those with a history of diabetic ketoacidosis, lower BMI (<20kg/m2) and high blood glucose levels or losing weight, patients over >75 years of age who are frail or are unwell in the peri-operative setting. He noted that as genital mycotic infections are common, physicians should explain to patients empagliflozin’s mechanism of action, emphasize the importance of proper genital hygiene and how to treat the infection if it occurs. Patients should also be informed about the potential drop in kidney function when initiating empagliflozin. Dr. Karalliedde reassured that it represents a temporary respite for the kidneys, and it would quickly stabilize, transforming into a better-preserved renal function over the long term.
Conclusion
It is important to understand the interconnectedness of the CKM systems and how dysfunction in one area can affect the others. Extensive evidence from clinical trials affirms that irrespective of the patients’ T2D status, empagliflozin confers benefits across the CKM axis for patients with comorbid HF and DKD.10-13 SGLT2is like empagliflozin should be started as early as possible in these patients to improve their quality of life.15 Thus, primary care physicians should proactively screen and treat patients earlier to prevent delays in accessing therapeutic benefits from potentially life-changing drugs like empagliflozin.
This is an independent editorial article, published and distributed through unrestricted educational support from the pharmaceutical community, for the purpose of continuing medical education only. The views expressed in this publication reflect the experience and/or opinion of the author(s) and are not necessarily those of editors, publisher, and sponsor(s). Because of rapid advances in medicine, independent verification of clinical diagnoses, medical suitability and dosage should be made before treatment prescription. The appearance of advertisement, if any, has no influence on editorial content or presentation and does not imply the endorsement of products by the publication, or its authors and editors.
- Ronco C, et al. Cardiorenal syndrome. J Am Coll Cardiol. 2008;52(19):1527-1539.
- Lovre D, et al. Managing Diabetes and Cardiovascular Risk in Chronic Kidney Disease Patients. Endocrinol Metab Clin North Am. 2018;47(1):237-257.
- Vijay K, et al. Heart Failure in Patients with Diabetes and Chronic Kidney Disease: Challenges and Opportunities. Cardiorenal Med. 2022;12(1):1-10.
- Birkeland KI, et al. Heart failure and chronic kidney disease manifestation and mortality risk associations in type 2 diabetes: A large multinational cohort study. Diabetes Obes Metab. 2020;22(9):1607-1618.
- Szczech LA, et al. Primary care detection of chronic kidney disease in adults with type-2 diabetes: the ADD-CKD Study (awareness, detection and drug therapy in type 2 diabetes and chronic kidney disease). PLoS One. 2014;9(11):e110535.
- Kidney Disease: Improving Global Outcomes (KDIGO) CKD Work Group. KDIGO 2024 Clinical Practice Guideline for the Evaluation and Management of Chronic Kidney Disease. Kidney Int. 2024;105(4S):S117-S314.
- Caramori ML, et al. Diabetic Kidney Disease. [Updated 2022 Aug 3]. In: Feingold KR, Anawalt B, Blackman MR, et al., editors. Endotext [Internet]. South Dartmouth (MA): MDText.com, Inc.; 2000-. https://www.ncbi.nlm.nih.gov/books/NBK279103/ Accessed April 25, 2024.
- Wanner C, et al. Empagliflozin and Progression of Kidney Disease in Type 2 Diabetes. N Engl J Med. 2016;375(4):323-34.
- Wanner C, et al. Consistent effects of empagliflozin on cardiovascular and kidney outcomes irrespective of diabetic kidney disease categories: Insights from the EMPA-REG OUTCOME trial. Diabetes Obes Metab. 2020;22(12):2335-2347.
- Packer M, et al. Cardiovascular and Renal Outcomes with Empagliflozin in Heart Failure. N Engl J Med. 2020;383(15):1413-1424.
- Anker SD, et al. Empagliflozin in Heart Failure with a Preserved Ejection Fraction. N Engl J Med. 2021;385(16):1451-1461.
- Zinman BZ, et al. Empagliflozin, Cardiovascular Outcomes, and Mortality in Type 2 Diabetes. N Engl J Med. 2015;373:2117-2128.
- Wanner C, et al. Empagliflozin and Clinical Outcomes in Patients With Type 2 Diabetes Mellitus, Established Cardiovascular Disease, and Chronic Kidney Disease. Circulation. 2018;137(2):119-129.
- Fernández-Fernandez B, et al. EMPA-KIDNEY: expanding the range of kidney protection by SGLT2 inhibitors. Clin Kidney J. 2023;16(8):1187-1198.
- McEwan P, et al. Understanding the inter-relationship between improved glycaemic control, hypoglycaemia and weight change within a long-term economic model. Diabetes Obes Metab. 2010;12(5):431-436.


