Heart failure with preserved ejection fraction (HFpEF) is becoming the predominant form of heart failure (HF), yet it is often underdiagnosed in clinical practice.1,2 In a recent webinar, Professor Andrew J. Stewart Coats from the Heart Research Institute, Sydney, Australia, underscored the urgent need for earlier detection and intervention. Central to this webinar was the transformative potential of sodium-glucose co-transporter 2 (SGLT2) inhibitors such as empagliflozin, which have shown remarkable benefits in improving outcomes, including the reduced risk of cardiovascular death or hospitalization for HF in patients across the ejection fraction spectrum.3,4 He also highlighted the importance of early diagnosis, adherence to guideline-directed medical therapy (GDMT), and the integration of emerging evidence-based treatments into routine clinical care.5,6
HFpEF: A common yet frequently missed diagnosis
HFpEF is emerging as the more prevalent form of HF compared with HF with reduced ejection fraction (HFrEF), accounting for approximately half of all HF hospitalizations.1 Its mortality rate is comparable to that of HFrEF, with similar outcomes observed over one year (mortality rate ~30%) to five years (mortality rate ~70%) .7 Studies show that 76% of patients with unrecognized HF have HFpEF, and one in six individuals over 65 years of age presenting with breathlessness in primary care may have undetected HF.2 The increasing prevalence of HFpEF has been partly linked to the historically limited treatment options compared to HFrEF.8 However, with the emergence of therapies like SGLT2 inhibitors, it is time this underrecognized condition receives greater attention.9
Prof. Coats noted, “This diagnostic gap contributes to poor outcomes and missed opportunities for timely intervention. It is very important that we get a diagnosis now that we do have proven treatments for HFpEF.” However, diagnosis is frequently delayed in clinical reality, with 55% of patients experiencing symptoms for up to five years before being correctly identified.10 Most diagnoses occur during unscheduled hospitalizations, underscoring the need for proactive screening in outpatient settings.10 Timely recognition enables the initiation of GDMT, which can significantly reduce cardiovascular mortality and hospitalizations.5,6
The challenge of early detection is further complicated by the need for precise differentiation, as HFpEF frequently coexists with or is obscured by common comorbidities such as chronic obstructive pulmonary disease (COPD) and obesity.11,12 These comorbidities can mask or mimic HFpEF symptoms, such as fatigue, exertional breathlessness, and reduced exercise tolerance, complicating clinical assessment.11,12 Prof. Coats explained, “We go from a heart-centered condition to a condition where the heart is damaged by a whole-body series of illnesses.”
Global guidelines for accurate HFpEF identification
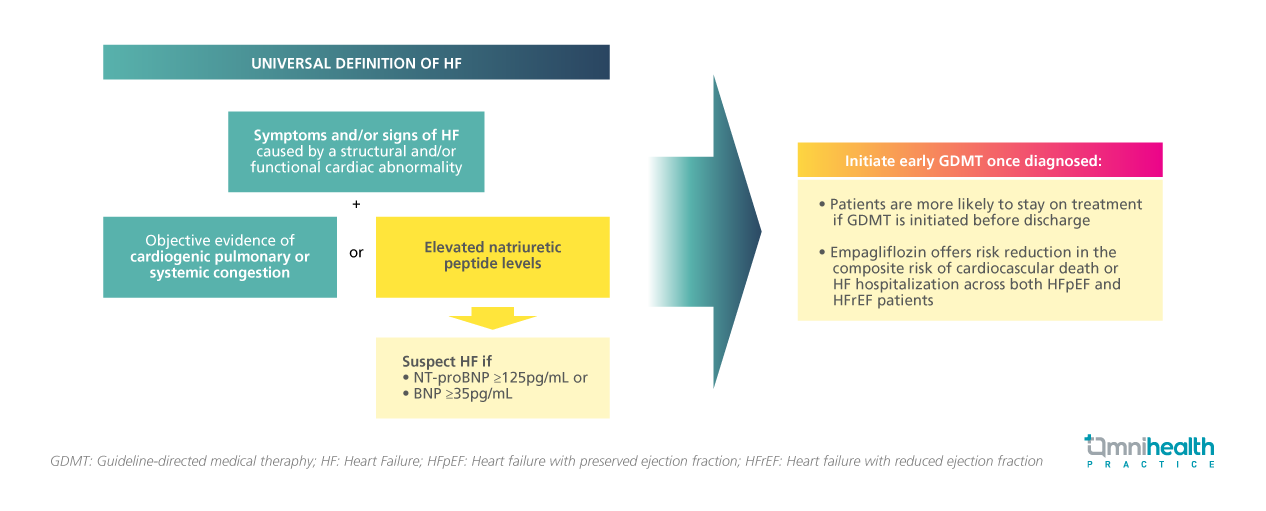
Given the diagnostic complexity of HFpEF, a standardized and evidence-based framework is essential to guide clinicians through the evaluation process and ensure accurate identification of HFpEF. Clinicians should differentiate HFpEF from other conditions through comprehensive evaluation, including echocardiography (ECHO), electrocardiography (ECG), and biomarker analysis, to avoid misdiagnosis and ensure appropriate treatment.10 International guidelines emphasize a structured approach to diagnosing HFpEF with its universal definition requiring symptoms or signs of HF, evidence of structural and/or functional cardiac abnormalities, with elevated natriuretic peptide (e.g. N-terminal pro-B-type natriuretic peptide [NT-proBNP]) levels, and/or objective evidence of cardiogenic pulmonary or systemic congestion by diagnostic modalities such as imaging.12
NT-proBNP levels ≥125pg/mL are considered diagnostic of HF, though values may vary with age, obesity, atrial fibrillation, and renal function.13 ECHO is central to confirming preserved ejection fraction (≥50%) and identifying features like left ventricular hypertrophy and left atrial enlargement.11,14 Additional tests—including chest X-ray, pulmonary function testing, and routine blood work—help rule out alternative diagnoses and assess comorbidities.11 Importantly, Prof. Coats explained that treatment with empagliflozin can be initiated based on NT-proBNP results alone, regardless of ejection fraction. This flexibility allows clinicians to begin treatment early, even before echocardiographic confirmation, ensuring timely intervention.
Empagliflozin delivers comprehensive benefits beyond HFpEF
The emphasis on early diagnosis is especially critical given that SGLT2 inhibitor such as empagliflozin has demonstrated sustained benefits across the full spectrum of HF patients.3,4 Empagliflozin has redefined HF management with its broad clinical benefits, as demonstrated in both the phase 3 randomized EMPEROR-Reduced and EMPEROR-Preserved trials, the latter of which Prof. Coats highlighted to be the first prospective trial in HFpEF to meet its primary endpoints.3,4
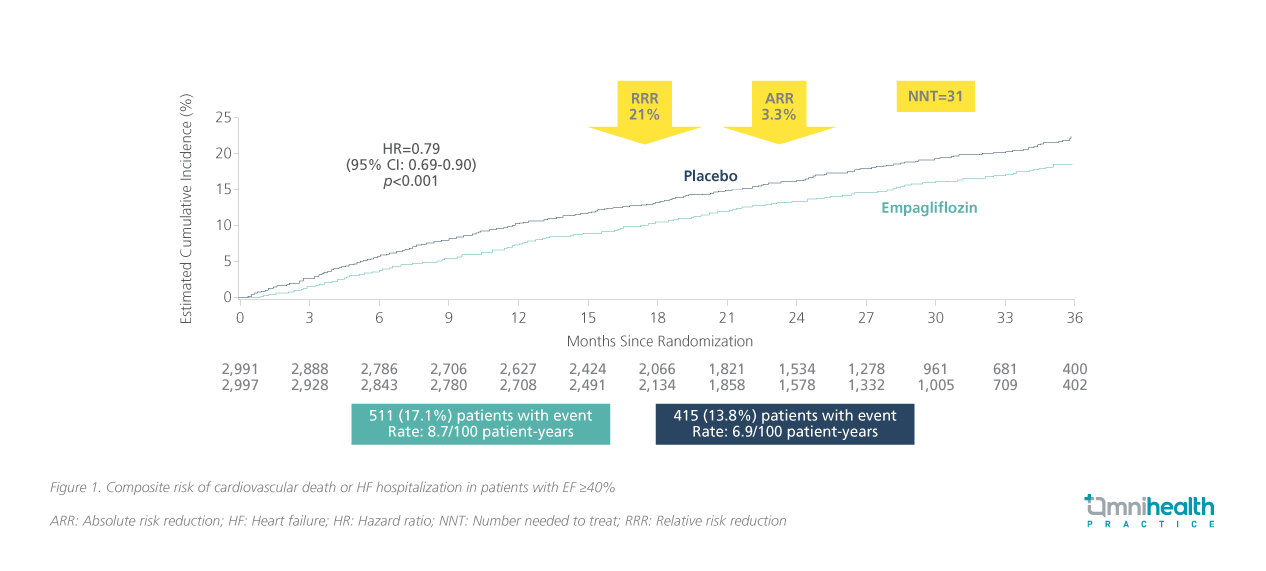
Empagliflozin’s therapeutic benefit was initially established in patients with HFrEF through the EMPEROR-Reduced trial, where it significantly reduced the risk of cardiovascular death or hospitalization for HF in HFrEF patients regardless of diabetes status by 25% compared to those who received placebo (HR=0.75; 95% CI: 0.65-0.86; p<0.001).4 In the EMPEROR-Preserved trial, empagliflozin reduced the composite risk of cardiovascular death or HF hospitalization in patients with ejection fraction ≥40% by 21% compared to placebo (HR=0.79; 95% CI: 0.69-0.90; p<0.001) (figure 1), with benefits emerging as early as 18 days after initiation.3,15 It also significantly slowed renal decline, offering protection beyond cardiac outcomes.3 Prof. Coats reflected on the impact of these findings: “There was an ovation in the audience as the truly first positive HFpEF trial we had ever had.”
The renal safety profile of empagliflozin is particularly notable—in both the EMPEROR-reduced and EMPEROR-preserved trials, empagliflozin was started in patients with an eGFR as low as 20mL/min/1.73m², making it accessible to those with advanced kidney disease.3,4,16 With a manageable safety profile and effectiveness in both HFrEF and HFpEF, empagliflozin has redefined HF management.3,4 As Prof. Coats highlighted, it stands as a foundational therapy in HF care, offering timely and meaningful improvements in outcomes.
Early initiation of GDMT for better adherence
To fully leverage the benefits of SGLT2 inhibitors such as empagliflozin, it is crucial to consider the timing of initiation, particularly following hospitalization.5,6 Evidence shows that patients discharged without GDMT are significantly less likely to receive it later, with post-discharge prescription rates dropping to as low as 7.7% (figure 2).5 Starting therapy before discharge not only enhances uptake but also protects patients during the post-hospitalization period.6 The benefits of implementing GDMT in reducing cardiovascular death, hospital readmission, and urgent HF visits, have been observed as early as 1-2 weeks after initiation.5,6 Since the availability of trials such as the EMPEROR-Preserved, , SGLT2 inhibitors have been established as foundational therapies recommended for not only HFrEF but also HFpEF patients, receiving class I recommendations in the European Society of Cardiology (ESC) guidelines.17
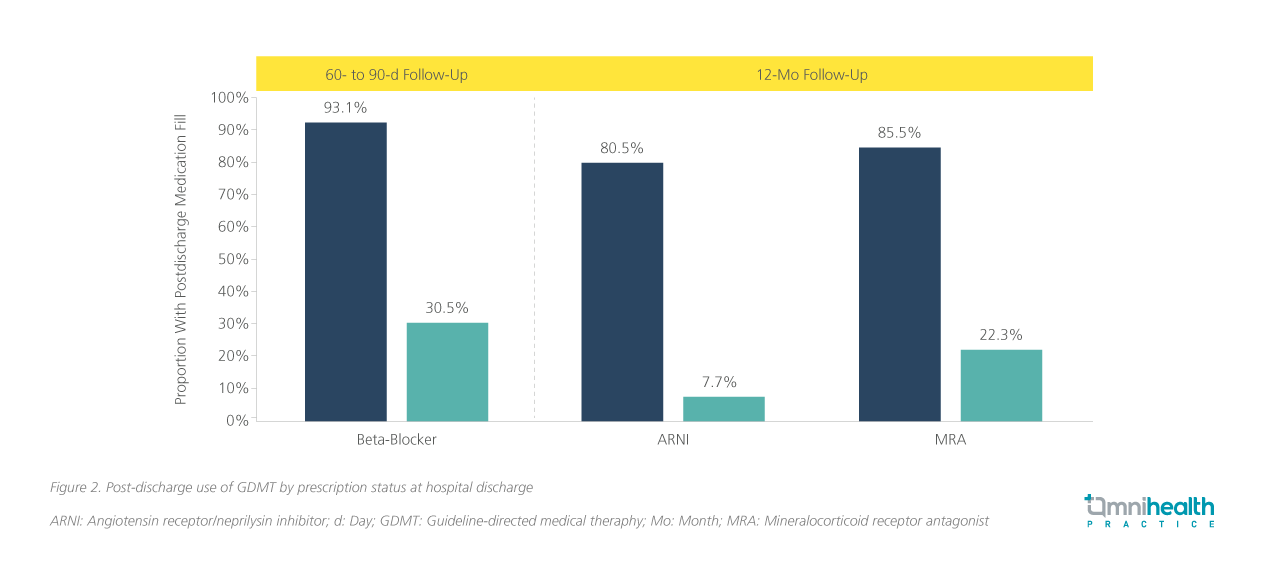
Prof. Coats advised, “It is very important that you initiate the SGLT2 inhibitor treatment because we want to protect the patient in terms of heart and kidney outcomes. If you are not on the drug at hospital discharge, the chance of being on the drug afterwards is much lower.” Starting empagliflozin before hospital discharge ensures early therapeutic benefit and better long-term adherence.5,6 Timely initiation of SGLT2 inhibitors aligns with guideline recommendations for comprehensive HF care.11,17 Prof. Coats encouraged clinicians to prescribe GDMT rather than defer, ensuring optimal adherence.
Conclusion
HFpEF is a serious yet treatable condition that demands greater clinical attention and urgency.1 With effective therapies now available, particularly SGLT2 inhibitors like empagliflozin, early diagnosis has become more critical than ever.3,4,17 Prof. Coats emphasized clinicians must maintain a high index of suspicion, especially in patients with comorbidities, to avoid missed opportunities for intervention. The advent of SGLT2 inhibitors marks a breakthrough in HF management, offering rapid and sustained improvements in outcomes.3,4 By recognizing HFpEF early and initiating guideline-directed therapy promptly, healthcare providers can improve the prognosis of this once elusive condition and deliver impactful, patient-centered care
This is an independent editorial article, published and distributed through unrestricted educational support from the pharmaceutical community, for the purpose of continuing medical education only. The views expressed in this publication reflect the experience and/or opinion of the author(s) and are not necessarily those of editors, publisher, and sponsor(s). Because of rapid advances in medicine, independent verification of clinical diagnoses, medical suitability and dosage should be made before treatment prescription. The appearance of advertisement, if any, has no influence on editorial content or presentation and does not imply the endorsement of products by the publication, or its authors and editors.
- Oktay AA, et al. The emerging epidemic of heart failure with preserved ejection fraction. Curr Heart Fail Rep. 2013;10(4):401-10.
- van Riet EE, et al. Prevalence of unrecognized heart failure in older persons with shortness of breath on exertion. Eur J Heart Fail. 2014;16(7):772-7.
- Anker SD, et al. Empagliflozin in Heart Failure with a Preserved Ejection Fraction. N Engl J Med. 2021;385(16):1451-1461.
- Packer M, et al. Cardiovascular and Renal Outcomes with Empagliflozin in Heart Failure. N Engl J Med. 2020;383(15):1413-1424.
- Rao VN, et al. In-Hospital Initiation of Sodium-Glucose Cotransporter-2 Inhibitors for Heart Failure With Reduced Ejection Fraction. J Am Coll Cardiol. 2021;78(20):2004-2012.
- American College of Cardiology. Inpatient Initiation of HFrEF Therapies. Available at: https://www.acc.org/Latest-in-Cardiology/Articles/2022/06/01/12/11/Inpatient-Initiation-of-HFrEF-Therapies. Accessed: June 20, 2025.
- Owan TE, et al. Trends in prevalence and outcome of heart failure with preserved ejection fraction. N Engl J Med. 2006;355(3):251-9.
- Vasan RS, et al. Epidemiology of Left Ventricular Systolic Dysfunction and Heart Failure in the Framingham Study: An Echocardiographic Study Over 3 Decades. JACC Cardiovasc Imaging. 2018;11(1):1-11.
- Borlaug BA, et al. Heart Failure With Preserved Ejection Fraction: JACC Scientific Statement. J Am Coll Cardiol. 2023;81(18):1810-1834.
- Bottle A, et al. Routes to diagnosis of heart failure: observational study using linked data in England. Heart. 2018;104(7):600-605.
- McDonagh TA, et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J. 2021;42(36):3599-3726.
- Vaduganathan M, et al. Mode of Death in Heart Failure With Preserved Ejection Fraction. J Am Coll Cardiol. 2017;69(5):556-569.
- Bozkurt B, et al. Universal definition and classification of heart failure: a report of the Heart Failure Society of America, Heart Failure Association of the European Society of Cardiology, Japanese Heart Failure Society and Writing Committee of the Universal Definition of Heart Failure: Endorsed by the Canadian Heart Failure Society, Heart Failure Association of India, Cardiac Society of Australia and New Zealand, and Chinese Heart Failure Association. Eur J Heart Fail. 2021;23(3):352-380.
- StatPearls. Left Ventricular Ejection Fraction. Available at: https://www.ncbi.nlm.nih.gov/books/NBK459131/. Accessed: June 20, 2025.
- Butler J, et al. Early benefit with empagliflozin in heart failure with preserved ejection fraction: insights from the EMPEROR-Preserved trial. Eur J Heart Fail. 2022;24(2):245-248.
- Jardiance® (empagliflozin). Hong Kong Prescribing Information. 2024.
- McDonagh TA, et al. 2023 Focused Update of the 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J. 2023;44(37):3627-3639.


