CASE REVIEW
Case Sharing: Early dapagliflozin stabilizes patients with acute decompensated heart failure regardless of ejection fraction
Heart failure (HF) is a complex condition characterized by pathophysiologic heterogeneity and the presence of congestive symptoms, particularly in cases of acute decompensated heart failure (ADHF).1,2 These factors significantly increase the risk of hospitalization due to HF worsening and cardiovascular (CV) death.2,3 In a recent interview with Omnihealth Practice, Dr. Fong, Yan-Hang Esmond shared two notable cases from the Queen Elizabeth Hospital (QEH) that highlighted the early use of dapagliflozin, a sodium-glucose co-transporter-2 (SGLT2) inhibitor. These cases involved patients with heart failure with preserved ejection fraction (HFpEF) and heart failure with reduced ejection fraction (HFrEF), as confirmed by serum N-terminal prohormone of brain natriuretic peptide (NT-proBNP) levels and echocardiogram (ECHO) assessment results. The early initiation of dapagliflozin in both cases played a crucial role in rapidly stabilizing the patients' conditions and facilitating a smooth transition to the discharge phase.
Background
Unmet needs in the management of HF The treatment landscape for HFpEF and HFrEF are vastly distinct, with HFpEF presenting unique challenges in terms of diagnosis and treatment.1 HFpEF is often masqueraded as other forms of CV diseases such as cardiac amyloidosis, hypertrophic cardiomyopathy, high-output HF or valvular heart disease.1 “In practice, the diagnosis of patients with HFpEF may be delayed due to the lack of timely echocardiogram and complexity in interpreting the results” Dr. Fong explained.
Dr. Fong pointed out that compared to HFrEF, treatment options for HFpEF patients are more limited. Guidelines from the European Society of Cardiology (ESC) and the American College of Cardiology/American Heart Association/Heart Failure Society of America (ACC/AHA/HFSA) widely endorse the use of beta-blockers, angiotensin receptor blockers (ARBs), angiotensin receptor-neprilysin inhibitors (ARNIs), mineralocorticoid receptor antagonists (MRAs), and SGLT2 inhibitors as the ‘4-pillar’ cornerstone for the treatment of HFrEF.4 In contrast, the complexity and heterogeneity of the HFpEF syndrome make it challenging to adopt a “one-size-fits-all” approach, resulting in limited pharmacological options for HFpEF patients.1
Potential threats associated with ADHF
Patients with chronic HF and other medical comorbidities such as renal dysfunction and diabetes are susceptible to decompensation, often presenting with symptoms of congestion and fluid retention.2 Dr. Fong emphasized the importance of promptly addressing congestion symptoms such as peripheral edema, which are particularly prevalent in up to 39.2% of Southeast Asian patients with ADHF.5
“Decongestion should be performed for ADHF patients regardless of their left ventricular ejection fraction (LVEF) status,” Dr. Fong added, “While diuretics are the mainstay option for decongestion, they are unsuitable for patients with impaired renal function due to the potential risk of kidney overload and over-diuresis.” As such, it is crucial to adopt appropriate and comprehensive decongestion approaches to prevent residual congestion and minimize the frequency and severity of rehospitalizations.3
Dapagliflozin facilitated notable clinical benefits in HF patients
Dapagliflozin, an SGLT2 inhibitor, has been shown to improve survival outcomes of HF patients in many randomized controlled trials.6 A meta-analysis of 22 studies revealed that dapagliflozin significantly reduced all-cause mortality (p=0.006), HF hospitalization (p<0.00001), and CV death (p=0.01) compared to placebo.6 Subsequent subgroup analysis confirmed the consistency of dapagliflozin in reducing the incidence of the composite outcome of HF hospitalization or urgent HF visits among both HFpEF (p=0.001) and HFrEF (p<0.0001) patients.6 Moreover, dapagliflozin diminishes the need for diuretics in HFpEF patients.7 A prespecified analysis of the DELIVER trial demonstrated that dapagliflozin reduced new initiations of loop diuretics by 32% (HR=0.68; 95% CI: 0.55-0.84; p<0.001).7 Patients receiving dapagliflozin were less likely to require loop diuretic initiation or dose increase (p<0.001) and more likely to experience loop diuretic discontinuation or dose decrease (p<0.001).7
Assessing the eligibility of HF patients for early initiation of dapagliflozin
LVEF and NT-proBNP are key prognostic parameters in HF management, with both recommended for risk stratification in the 2022 AHA/ACC/HFSA and 2021 ESC guidelines.8,9 A post-hoc analysis of the DELIVER trial revealed that patients with higher baseline NT-proBNP concentrations faced an elevated risk of CV death or HF worsening events (p<0.001).10 Additionally, a retrospective study published in 2020 demonstrated that reductions in LVEF were associated with comparable increases in mortality and hospitalizations for both cardiac and noncardiac admissions (p<0.001).11
Nevertheless, Dr. Fong acknowledged the long waiting times for LVEF assessments using ECHO, which has prompted greater reliance on NT-proBNP assessments in HF screening, with the recommended HF diagnostic algorithms of the AHA/ACC/HFSA and ESC guidelines suggesting a plasma concentration of NT-proBNP ≥125pg/mL as a threshold indicative of HF.8,9 To demonstrate the clinical benefits of early dapagliflozin initiation, Dr. Fong recounted 2 patients who presented with ADHF symptoms and were later diagnosed with HFpEF and HFrEF respectively. In both cases, dapagliflozin was initiated early based on the patients’ serum NT-proBNP levels and LVEF statuses.
Case sharing
Case 1: A 78-year-old female patient with HFpEF
In July 2023, a 78-year-old woman weighing 80kg with comorbid ischemic heart disease and hypertension was admitted to the hospital due to shortness of breath. She had a history of percutaneous coronary intervention and was on three antihypertensive medications (lovastatin, amlodipine, beta-blockers). The patient also had impaired kidney function, with a creatinine level of 150μmol/L and an estimated glomerular filtration rate (eGFR) of 45%.
Initially, she was diagnosed with pneumonia based on mild haziness observed on chest X-ray and was discharged after receiving a course of antibiotics. However, she was rehospitalized in September 2023 with symptoms of shortness of breath, tachycardia (heart rate=120bpm), peripheral edema, and congestive signs on chest X-ray. Her NT-proBNP level was assessed and found to be 6,300pg/mL, leading to a diagnosis of atrial fibrillation and ADHF.
To stabilize the patient's heart rate, intravenous amiodarone was administered. Furosemide was given for decongestion, and anticoagulant agents were initiated for atrial fibrillation. By the third day of hospitalization, the patient's condition had stabilized. Subsequently, ECHO was performed, revealing an LVEF status of 55%-60% with left ventricular hypertrophy and left atrial enlargement. Based on the results of the NT-proBNP assessment and ECHO, dapagliflozin was initiated for the patient. On the 4th day of hospitalization, the patient was discharged when her blood pressure (BP) returned to 128/68mmHg, heart rate normalized to 70bpm, and blood oxygen saturation (SpO2) reached 98%.
The patient was monitored through follow-up visits at specialist outpatient clinics, which revealed that the treatment provided significant relief of most HF symptoms. The patient was classified as Class I according to the New York Heart Association (NYHA) Classification, and her renal function and heart rate remained stable. No adverse events related to dapagliflozin or hospital readmissions occurred. The patient is scheduled to undergo an ablation surgery to treat her atrial fibrillation.
Case 2: A 60-year-old male patient with HFrEF
In May 2023, a 60-year-old male smoker with a 5-year history of hypertension was admitted to the hospital. The patient presented with symptoms of shortness of breath and peripheral edema, along with severely elevated BP (190/100mmHg) and a heart rate of ≥90bpm, indicating a hypertensive emergency. Subsequent blood tests revealed impaired renal function (eGFR 32%) and significantly elevated NT-proBNP levels (12,500pg/mL). ECHO results indicated a LVEF of 15%-20%, as well as findings consistent with HFrEF, including dilated cardiomyopathy and moderate functional mitral regurgitation.
During the patient's 5-day hospital stay, in addition to bisoprolol fumarate, sacubitril/valsartan and spironolactone, dapagliflozin 10mg daily was initiated as part of the treatment regimen. Intravenous diuretics were administered to alleviate congestive symptoms. Overall, the patient tolerated the treatment well, and BP was stabilized at 130/70mmHg.
Upon discharge, the patient was enrolled in the QEH HF program and transferred to an outpatient transition clinic for close monitoring and up-titration of medications. The program provided comprehensive support, including counseling on lifestyle modifications, drug reconciliation by pharmacists, physiotherapy, occupational therapy and cardiac rehabilitation.
After 4 months, follow-up assessments revealed a significant improvement in NT-proBNP levels (reduced to 300pg/mL) and an LVEF of 55%-60%. The patient remained free of HF symptoms and complications up to the present day, indicating a favorable response to the treatment approach.
Discussion
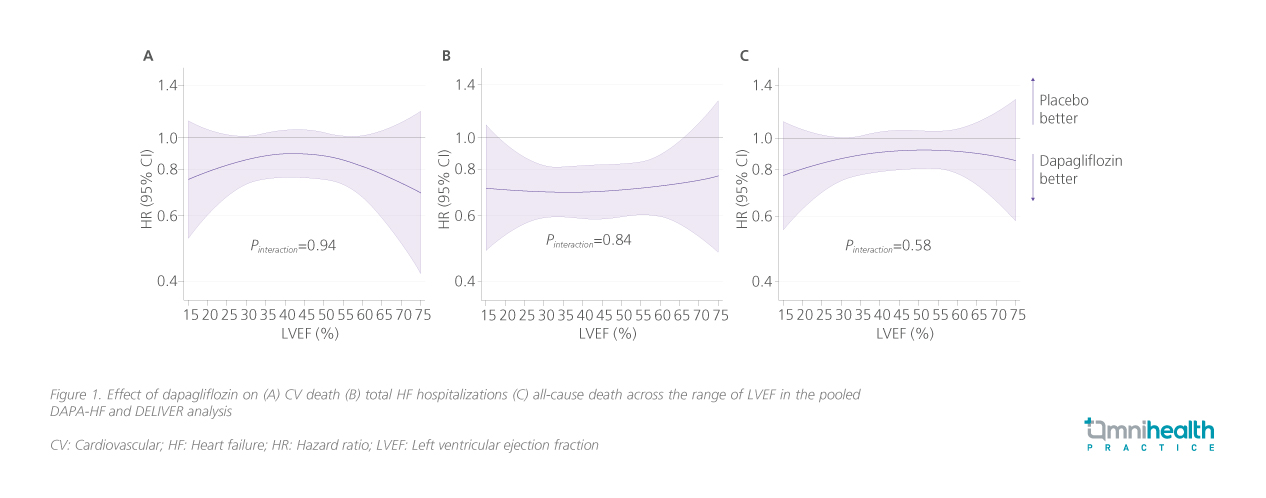
SGLT2 inhibitors have consistently demonstrated clinical benefits in patients with HF regardless of LVEF status.12 They are the only disease-modifying drug class that is recommended as first-line treatment for HF irrespective of LVEF status by the ESC.12 Dr. Fong emphasized that dapagliflozin, in particular, has robust clinical evidence supporting its efficacy and tolerability in HF patients across multiple ranges of LVEF. Such advantages were retained in the real world as seen in his clinical cases. In a pooled analysis of patients with HFrEF and HFpEF from the DAPA-HF and DELIVER studies, dapagliflozin demonstrated significant reductions in the risks of CV death (HR=0.86; 95% CI: 0.76-0.97; p=0.01), all-cause death (HR=0.90; 95% CI: 0.82-0.99; p=0.03) and total HF hospital admissions (RR=0.71; 95% CI: 0.65-0.78; p<0.001) compared to placebo.13 These clinical benefits of dapagliflozin were retained across the range of LVEF (CV death pinteraction= 0.94; total HF hospital admission pinteraction=0.84; all-cause death pinteraction= 0.58) (figure 1).13 Furthermore, dapagliflozin facilitated additional benefits across the cardio-renal-metabolic (CRM) spectrum.14 In a post-hoc analysis of the DELIVER trial, dapagliflozin was associated with a significant reduction in composite CV death or HF worsening events in HFpEF patients regardless of their baseline number of CRM conditions (pinteraction=0.734) or their CRM overlap status (pinteraction=0.773).14
Conclusion
Previous clinical studies have demonstrated the reliable efficacy of dapagliflozin in reducing the risk of CV death, HF hospitalizations and worsening of HF.6,7 The clinical cases shared by Dr. Fong offered insights into the clinical reality and the application of dapagliflozin in both HFpEF and HFrEF patients. Dr. Fong concluded that considering the narrow selection of treatment options available for HFpEF patients, SGLT2 inhibitors such as dapagliflozin offer a reliable and safe approach to managing HF progression and reducing the risk of developing comorbidities.
This is an independent editorial article, published and distributed through unrestricted educational support from AstraZeneca Hong Kong Limited, for the purpose of continuing medical education only. The views expressed in this publication reflect the experience and/or opinion of the author(s) and are not necessarily those of editors, publisher and sponsor(s). Because of rapid advances in medicine, independent verification of clinical diagnoses, medical suitability and dosage should be made before treatment prescription. The appearance of advertisement, if any, has no influence on editorial content or presentation and does not imply the endorsement of products by the publication, or its authors and editors.
- Omote K, et al. Heart Failure with Preserved Ejection Fraction: Mechanisms and Treatment Strategies. Annu Rev Med. 2022;73:321-337.
- Kurmani S, et al. Acute Heart Failure: Definition, Classification and Epidemiology. Curr Heart Fail Rep. 2017;14(5):385-392.
- Boorsma EM, et al. Congestion in heart failure: a contemporary look at physiology, diagnosis and treatment. Nat Rev Cardiol. 2020;17(10):641-655_Suppl.
- Bayés-Genís A, et al. Head-to-head comparison between recommendations by the ESC and ACC/AHA/HFSA heart failure guidelines. Eur J Heart Fail. 2022;24(6):916-926.
- Filippatos G, et al. Global Differences in Characteristics, Precipitants, and Initial Management of Patients Presenting With Acute Heart Failure. JAMA Cardiol. 2020;5(4):401- 410.
- Ali AE, et al. Effect of Dapagliflozin in Patients with Heart Failure: A Systematic Review and Meta-Analysis. Glob Heart. 2023;18(1):45.
- Chatur S, et al. Dapagliflozin and diuretic utilization in heart failure with mildly reduced or preserved ejection fraction: the DELIVER trial. Eur Heart J. 2023;44(31):2930-2943.
- Heidenreich PA, et al. 2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2022;145(18):e895-e1032
- McDonagh TA, et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J. 2021;42(36):3599-3726
- Myhre PL, et al. Influence of NT-proBNP on Efficacy of Dapagliflozin in Heart Failure With Mildly Reduced or Preserved Ejection Fraction. JACC Heart Fail. 2022;10(12):902-913.
- Angaran P, et al. Association of Left Ventricular Ejection Fraction with Mortality and Hospitalizations. J Am Soc Echocardiogr. 2020;33(7):802-811.e6.
- Docherty KF, et al. The four pillars of HFrEF therapy: is it time to treat heart failure regardless of ejection fraction? Eur Heart J Suppl. 2022;24(Suppl L):L10-L19.
- Jhund PS, et al. Dapagliflozin across the range of ejection fraction in patients with heart failure: a patient-level, pooled metaanalysis of DAPA-HF and DELIVER. Nat Med. 2022;28(9):1956-1964.
- Ostrominski JW, et al. Cardio-Renal-Metabolic Overlap, Outcomes, and Dapagliflozin in Heart Failure With Mildly Reduced or Preserved Ejection Fraction. JACC Heart Fail. 2023;11(11):1491-1503.

