EXPERT INSIGHT
Balancing sensitivity with specificity in cervical cancer screening by co-testing with HPV and cytology
The Hong Kong College of Obstetricians and Gynaecologists (HKCOG) has recently updated its guidelines on the prevention and screening of cervical cancer.1 The latest recommendations incorporated recent evidence on the role of co-testing with human papillomavirus (HPV)-based screening and cytology-based screening.1 In an interview with Omnihealth Practice, Dr. Wong, Ching-Yin Grace shared the rationale behind co-testing as the preferred testing modality in The Family Planning Association of Hong Kong as it offers concurrent triaging. The combination of sensitivity with HPV tests and the specificity with cytology tests allows for a more lenient screening schedule for women in Hong Kong without compromising the benefit of cervical cancer detection.
Strategies against cervical cancer on a local level
Oncoviruses like HPV are known to cause cancers like cervical cancer.2 Just the 2 strains of HPV16 and HPV18 account for around 50% and 20% of cervical cancers respectively.2 Vaccination and screening of these pathogens on a global scale are active prevention strategies essential to cervical cancer prevention as outlined by the World Health Organization.2,3 However, Dr. Wong cautioned that local strategies that consider regional needs and infrastructure are needed for effective implementation. As such, the local guidance published by the HKCOG on cervical cancer prevention and screening has been updated to reflect the latest data and recommendations.1
The merits of adding HPV tests in cervical cancer screening
In Hong Kong, the nonvalent HPV vaccine has been incorporated into the Hong Kong Childhood Immunisation Programme (HKCIP) since 2019, offering a 2-dose schedule for girls administered in Primary 5 and Primary 6 respectively.1 The efforts have resulted in a wide coverage of >80% among these girls.1 Additionally, catchup HPV vaccinations have been suggested to be offered to older girls up to the age of 18 who have previously missed the vaccination program.1
The HPV vaccine does not protect against all types of HPV infections, and by extension not all cases of cervical cancer.1 As such, continuous screening after vaccination is still essential according to the HKCOG guidelines.1 Dr. Wong discerned that effective screening methods need to be both highly sensitive and specific due to the high rates of vaccination and the availability of 9-valent vaccines in Hong Kong. In systematic reviews conducted over 2 decades ago, it was already known that HPV-based tests for cervical intraepithelial neoplasia grade ≥2 (CIN2+) lesions have higher sensitivity (90.0%vs. 72.7%) than cytology-only tests for atypical squamous cells of undetermined significance (ASCUS), at the cost of lower specificity (86.5% vs. 91.9%).4
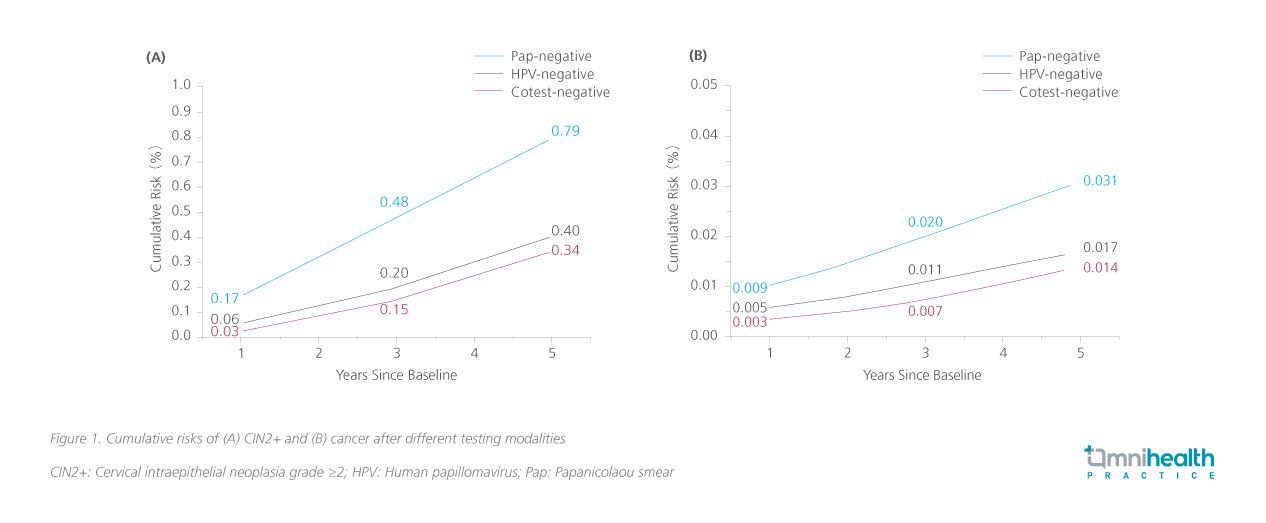
More recent pooled analyses on patients receiving stand-alone HPV tests or co-testing with cytology had up to 70% greater protection against invasive cervical carcinoma over cytology alone.5 At 2.5 years after study enrolment, the detection rate of invasive cervical carcinoma was significantly lower in patients screened with HPV-based tests with a rate ratio (RR) of 0.45 (95% CI: 0.25-81).5 The better detection of invasive cervical carcinoma with HPV-based testing has allowed screening intervals to be extended to 5 years without compromising the efficacy of these tests.5 In fact, a negative co-testing result has been shown to incur the lowest cumulative risk compared with HPV-only or cytology-only tests in terms of CIN2+ and cancerous lesions.6 In a large-scale population-based study, co-testing offered significant improvements over cytology alone and marginal improvements over HPV alone (figure 1).6
The HKCOG guidelines included algorithms for both HPV stand-alone testing and co-testing modalities, however, Dr. Wong endorsed the co-testing model for its precision as it allows concomitant triaging of HPV-positive women to avoid over-investigations and treatments. The guidelines also listed specific guidance on who to test, how to test, and how often to test, and suggested that for any HPV-based testing to be considered effective, it needs to be clinically and analytically validated and should target on high-risk strains alone including HPV16 and HPV18, instead of other strains that may be unrelated to cervical cancer.1
Comparing available screening options
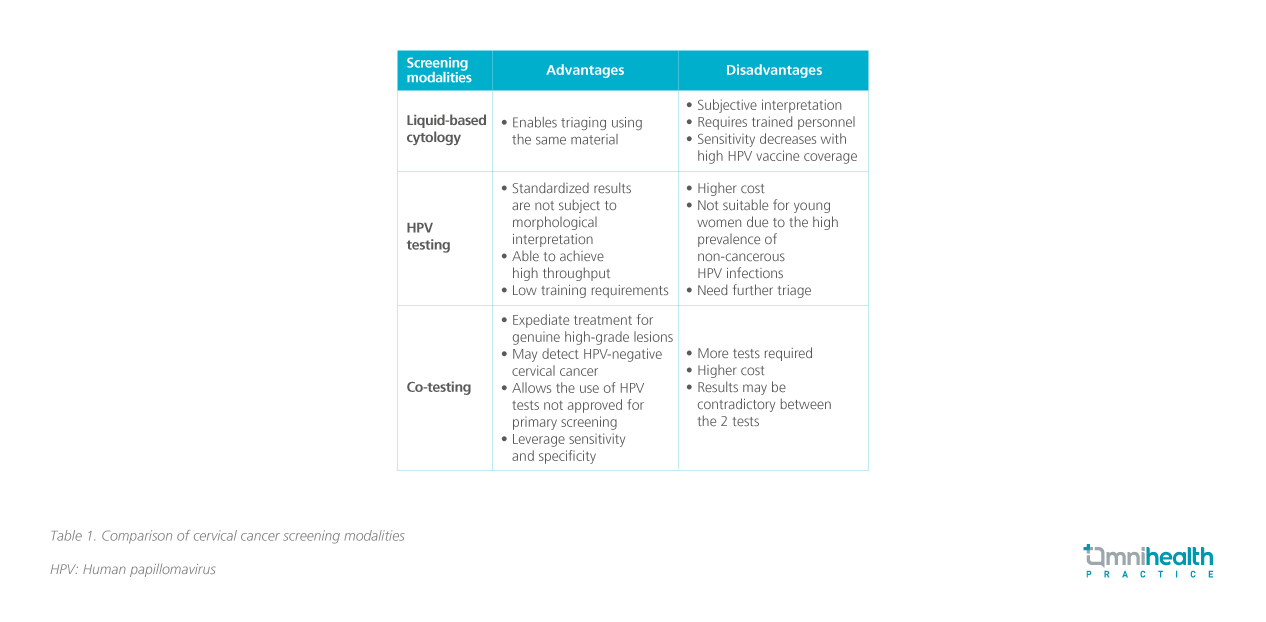
Despite the many advantages of HPV testing and co-testing, Dr. Wong reminded that the value of cytology screening alone is not lost. Cytology alone offers additional benefits like opportunistic detection of other infections such as herpes, trichomonas, bacterial cells, fungal cells, HPV-independent squamous cell carcinoma of cervix and secondary malignancies. Dr. Wong added that cytology offers guidance for colposcopy, and helps differentiate squamous or glandular lesions. A brief comparison of the 3 screening modalities listed in the HKCOG guidelines is presented in table 1.7
Triage after initial screening to avoid overtreatment
The addition of a cytology test as triage is recommended for those with a positive HPV screening test in the HKCOG.1 The low specificity and high sensitivity of HPV testing may lead to higher rates of false positive results and result in many patients being referred for colposcopy.1 Although colposcopies are generally recognized as low-risk procedures, they can cause significant anxiety and discomfort in patients receiving the procedure.8 Increased colposcopy rates also incur a major burden on both the patient and the healthcare system by increased referral for additional treatments and costs.9 Procedures such as the loop electrosurgical excision procedure (LEEP) may be more common as a result, which may lead to higher chances of preterm delivery.9
In the updated guidelines, colposcopy was not offered reflexively for patients with positive stand-alone HPV tests.1 In Hong Kong, further triaging should be conducted to confirm cytology findings and avoid over-referral to colposcopy.1 Triaging cytology results with HPV test is recommended in ASCUS cases.1 Even among low-grade squamous intraepithelial lesions (LSILs), some of these lesions may be transient and resolve spontaneously over 2 years and may not necessitate further treatment.1
Co-testing as the model of best-fit
Dr. Wong acknowledged that although there is no definitive best method of triaging, HPV and cytology co-testing has presented itself as one of the more suitable options in Hong Kong. Considering the needs and resources available to the local population, co-testing allows for an efficient paradigm of concurrent screening and triaging. It can also reduce the impact of false negative HPV test alone and detect HPV-independent cervical cancer.
Regarding the situation in Hong Kong, Dr. Wong said that there is longstanding infrastructure and training in place to support the extensive use of cytology for triaging alongside the lately recommended HPV-based screening. Non-profit organizations like The Family Planning Association of Hong Kong (FPAHK) offer screening tests for women as well as training on cervical cancer screening and colposcopy for healthcare professionals. Co-testing with HPV and cytology is an instantaneous and concomitant way of screening and triaging.1 It reduces the burden of treatments and spaces out testing intervals to 5 years compared with the 3-year interval with cytology-only testing.1 With co-testing, the frequency of appointments and the anxiety associated with treatment may be reduced without an increased risk of delaying treatment.
Efficacy of co-testing in local populations
A prospective randomized controlled trial conducted in the Hong Kong population recently has proven the value of co-testing over cytology only.9 In the study, 15,955 women between the ages of 30 and 60 were screened and were randomized 1:1 to be managed according to the liquid-based cytology (LBC) results alone (control arm) or LBC together with HPV test (intervention arm).9
The study population had cytology-testing habits at baseline with 94.3% having had prior screening and 47.2% having had annual screening prior to entry.9 The rate of detection of CIN2+ lesions was significantly higher in the intervention arm (0.95% vs. 0.38%; OR=2.50; 95% CI: 1.65-3.88; p<0.001).9 However, at 36 months, CIN2+ became significantly lower in the intervention group (0.08% vs. 0.35%; OR=0.23; 95%CI: 0.08-0.57; p=0.003), showing that the addition of HPV screening led to an earlier detection of CIN2+ lesions.9 The effectiveness of screening is well-demonstrated in the subgroup of women who had never been screened before the study, where both arms had similar rates of CIN2+ detection at baseline (p=0.162) with no additional CIN2+ lesions detected in the subsequent rounds.9
The study was initiated prior to the publication of the updated guidelines, thus the protocol included colposcopy immediately after a positive high-risk HPV test.9 As a result, there was a 4-fold increase in colposcopy rate (10.6% vs. 2.4%; p<0.001) which echoes the concern with overtreatment.9
Pointing the way forward
Besides the 3 modalities of testing recommended by the HKCOG guidelines, other innovations were also mentioned and may help increase the accessibility of testing by allowing them to obtain samples in the privacy of their own homes.10 In a study investigating the effectiveness of HPV self-sampling among women who are reluctant or unable to attend regular screening, the uptake rate has reached more than 60% with a concordance rate of 90% compared with clinician-sampled specimens, opening up new possibilities for screening to reach a wider population.10
Conclusion
Co-testing with HPV and cytology is both sensitive and specific in cervical cancer screening, facilitating appropriate follow-up and reducing the burden of colposcopy overtreatment. It also allows for concurrent screening and triaging and is effective in local populations who are mostly HPV-vaccinated and attend screening regularly. Dr. Wong concluded that cervical cancer screening is an evolving practice and that stakeholders need to be prepared for the changes in screening modality and be aware of the latest evidence on screening from around the world.
"Co-testing with HPV and cytology is an instantaneous and concomitant way of screening and triaging"
Dr. Wong, Ching-Yin Grace
Specialist in Obstetrics and Gynaecology

