EXPERT INSIGHT
Cervical cancer elimination in Hong Kong by enhancing HPV vaccination, routine screening and disease awareness
Cervical cancer (CC) is the 4th most common female cancer globally, claiming more than 300,000 women’s lives in 2018.1 In Hong Kong, the incidence of CC remained high at around 7 per 100,000 women in 2019, which was still below the World Health Organization’s (WHO) target of fewer than 4 per 100,000 women.1,2 Thanks to the availability of the Human papillomavirus (HPV) vaccine, enormous efforts have been made to increase the local vaccination rate among eligible females for the prevention of CC.3-5 Yet, since HPV vaccination cannot treat pre-existing HPV infection, nor do they offer 100% CC protection, screening remains the key to allow for early identification of pre-cancerous disease and timely intervention for increasing the likelihood of cure.3 In an interview with Omnihealth Practice, Dr. Poon, Che-Mun Patricia discussed the importance of HPV vaccination and regular screening among eligible women, regardless of their vaccination status. While providing an update on the current progress of CC elimination in Hong Kong, she also shared a clinical case of a stage III CC patient with low disease awareness and highlighted the difficulty facing grassroots women in the fight against CC.
HPV vaccination to prevent CC
Studies have revealed that persistent HPV infection is the leading cause of CC.3 Among the 200 identified HPV subtypes, 12 were found to be carcinogenic, with HPV-16 and HPV-18 accounting for 50% and 10% of all CC cases and being associated with a 435-fold and a 248-fold increased risk of CC, respectively.3 Other subtypes include HPV-31, -33, -34, -35, and -58, each of which constituted about 2%-5% of cases.3 Since about 80% of women will be infected at some point in their lifetime, CC could cause a tremendous health burden to the society.3 Therefore, it is crucial to come up with effective measures to reduce the incidence of CC.
In 2006, the United States (US) Food and Drug Administration (FDA) approved the first HPV vaccine for the prevention of infection against the 4 most common subtypes of HPV, i.e., HPV-6, -11, -16, and -18.3 In 2016, the 9-valent HPV vaccine, which also covered HPV-31, -33, -34, -35, and -58, became available in Hong Kong, offering strong protection against about 90% of local CC cases.4,5
HPV vaccination is thus far the most effective way to prevent CC when it is administered before sexual activities begin.4 It is generally recommended for girls aged 9-26 years if not previously vaccinated.3For individuals aged 9-14 years, HPV vaccine can be given in 2-dose series, with the second dose administered 6-12 months after the first dose.6 For individuals aged 15-45 years, 3 doses of HPV vaccine should be scheduled at months 0, 2 and 6.6
Cervical screening is necessary, regardless of the HPV vaccination status
In fact, HPV vaccine cannot treat pre-existing HPV infection. As HPV vaccine has only become available since the mid-2000, many older women could have been infected with HPV and are at a high risk of CC.3,7 For younger individuals who have been vaccinated, it should be reminded that the risk of CC is not totally eliminated as some HPV-negative cases have been reported.3 Hence, cervical screening remains indispensable for all women beginning at the age of 20s for the identification of early signs of malignancy in the cervix.3
Papanicolaou cytology (Pap) smear is the current standard of cervical screening, which is performed by cytological collection from the transformation zone of the cervix.3,8 The specimens will be processed with specific staining, and that microscopic analysis will detect the presence of abnormal cytological findings and classify them from negative for cervical intraepithelial lesion (NILM) and malignancy to squamous cell carcinoma (SCC), according to the Bethesda system.8 Results of a collaborative study by the International Agency for Research on Cancer (IRAC) revealed a significant percentage reduction by 93.5% in the cumulative incidence of CC in women aged 35-64 years who have been screened with cervical cytology before age 35.7 Nevertheless, the Pap smear was reported to have a sensitivity of 55.4% only.3 Of note, the combination of HPV screening and genotyping has achieved a high sensitivity of 94.6% and is recommended for enhancing the accuracy.3
In general, Pap tests should be performed every 3 years, with HPV co-testing every 5 years until age 65.3 For women aged ≥30 years, it is recommended that they should also undergo a pelvic examination annually.3
WHO CC elimination initiative and its implementation in Hong Kong
Given the advancement in HPV vaccination and cervical screening over the past 2 decades, the WHO defines CC as a preventable and curable malignancy in females, as long as it is detected and managed early.1 Generally speaking, early-stage CC (stage I or II) can be effectively treated with surgical options, such as cryosurgery or hysterectomy with or without radiotherapy (RT) or chemoradiation, yielding a cure rate as high as 80%.3,9 For very large lesions (i.e., >4cm) or diseases of more advanced stages (e.g., stage III), RT with concurrent chemotherapy is usually the standard of care for primary treatment, achieving a relatively lower cure rate of 60%.3,9
In 2018, the WHO set an ambitious goal to eliminate CC globally, calling for all participating countries to reach and maintain a low incidence rate of CC to below 4 per 100,000 women by 2030 (in 2019, the incidence rate of CC in Hong Kong remained high at about 7 per 100,000 women) through boosting the HPV vaccination rate (i.e., 90% of girls by age 15), cervical screening (i.e., 70% of women to be screened with high performance tests by age 35 and again by age 45), as well as timely treatments for 90% of women with pre-cancer or more invasive disease.1,2
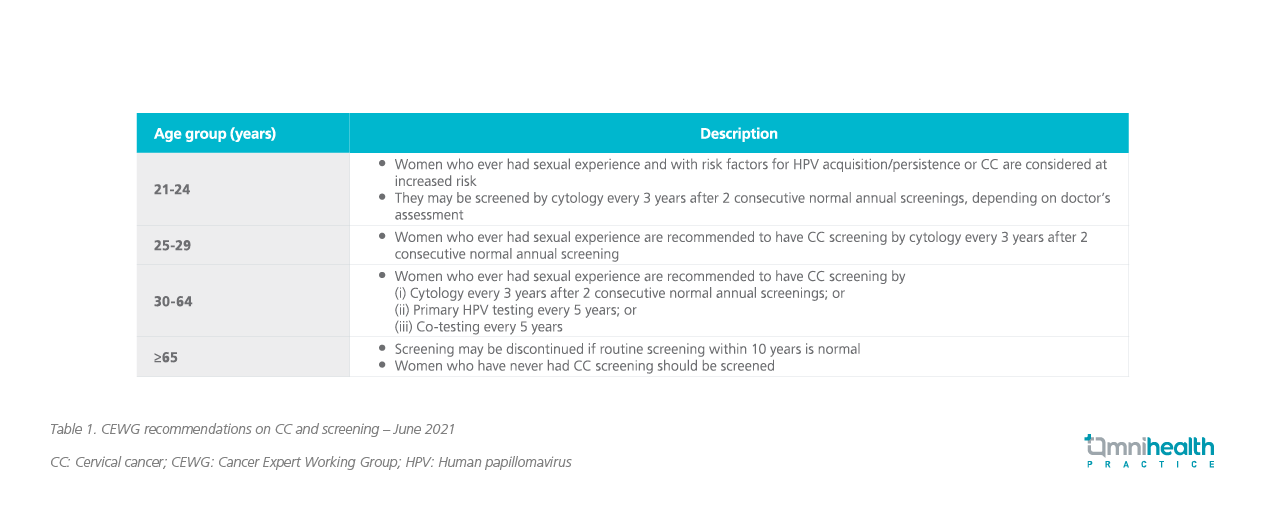
In response to the WHO’s call and recommendations, the health authorities in Hong Kong have included HPV vaccine in the Hong Kong Childhood Immunization Program (HKCIP), starting from the 2019/20 school year.7 All eligible female primary school students at suitable ages will receive HPV vaccination for the prevention of CC.7 Since HPV vaccine cannot treat pre-existing HPV infection, nor do they offer 100% protection from CC, the local health authorities stress that HPV vaccination should not replace CC screening and recommend that eligible women should undergo routine screening based on their risk of CC, regardless of their HPV vaccination status (table 1).7
Case sharing: A looming threat of low CC awareness among older grassroots women
A 58-year-old, blue-collar woman without past medical history sought medical attention due to heavy post-menopausal bleeding in 2016. She had been in menopause for 3 years when the bleeding started with spotting a few months earlier, which was mistaken as resumption of menstrual cycle by the patient. The patient had never received HPV vaccination, nor did she undergo regular gynecological check-up. Upon further examination, computed tomography (CT) and magnetic resonance imaging (MRI) scans revealed a large tumor of 5-6cm in the cervix, which had spread to the surrounding structures in the pelvis, confirming the diagnosis of stage III CC.
While surgery was no longer feasible for this patient, she was then managed with chemoradiation, i.e., RT, followed by cisplatin. After the cisplatin regimen, the patient, fortunately, achieved a complete response. During the whole course of treatment, she did not experience any major adverse events (AEs) and could still go to work, thanks to the advanced techniques in RT that enable radiation beam delivery to the tumor more accurately.
Despite the good response, the patient was worried about future relapse. Dr. Poon reassured her that the cure rate of stage III CC was relatively high (i.e., 60%), along with sufficient follow-up with her every 3-6 months. As of July 2022, the patient has remained in complete remission for more than 4 years.
Importance of early disease awareness
Dr. Poon reckoned that this patient was fortunate to have achieved a complete response and did not experience any serious adverse events (SAEs), despite the intensive chemoradiation therapy, since according to the literature, 40% of stage III patients could experience disease progression to metastatic state even with optimal treatment and eventually die of the disease. “Ideally, she could have come to me a few months earlier when she noticed the spotting. At earlier disease stages, surgery might still be feasible, and systemic therapies which are associated with more AEs could have been avoided,” Dr. Poon said, adding that “However, low disease awareness prevented the patient from doing so and made her miss the optimal treatment time.” Dr. Poon believed that this issue could be more serious among older grassroots women, particularly those who could hardly make ends meet and do not have time to care about their health. “Since every woman has the chance of getting CC, we need to do more to educate women on how to identify early signs of the disease, as well as the importance of early diagnosis,” Dr. Poon suggested.
Conclusion
All in all, the elimination of CC in Hong Kong is highly possible, thanks to the availability of the effective 9-valent HPV vaccine, the HPV vaccination campaign, and increased cervical screening, regardless of the HPV vaccination status. Unfortunately, low disease awareness among older grassroots women is an unaddressed issue and an obstacle to the quest for total eradication of CC. Further efforts might be warranted to educate and raise the awareness of early signs of CC among this group of women, so that earlier, simpler and safer treatments with a higher chance of cure could be rendered.

