CONFERENCE UPDATEL: AHA 2021
AVATAR trial demonstrates early surgery benefits in asymptomatic patients with severe as
Aortic valve replacement (AVR) therapy is believed to improve symptoms, LV function and survival in symptomatic patients with severe aortic stenosis (AS).1 However, the indication for AVR in this group of patients remains a debate.1 And it is hypothesized that the strategy of early valve replacement in patients with severe AS in the absence of symptoms can be more beneficial than watchful waiting in carefully selected patients.1 Therefore, the Aortic Valve replAcemenT versus conservative treatment in Asymptomatic seveRe aortic stenosis (AVATAR) trial was conducted, by Professor Marko Banovic, Associate Professor of Cardiology at University Clinical Centre of Serbia and University of Belgrade Medical School, and his team to evaluate the safety and efficacy of early surgical AVR in asymptomatic patients with severe AS and normal LV function.1 This is a physician-initiated, prospective, multicentre, randomized, open-label, parallel group trial performed in 9 medical centres in 7 European Union (EU) countries to reach minimum of 35 prespecified events.1 The primary composite endpoints included all-cause death, myocardial infarction, stroke or unplanned hospitalization for heart failure.
The eligible 157 asymptomatic patients at median age of 67, with severe AS (Aortic valve area ≤1.0cm2, mean aortic valve gradient ≥40mmHg or peak aortic jet velocity >4.0m/second), left ventricular ejection fraction (LVEF) >50%, and median predicted mortality risk according to the Society for Thoracic Surgeons (STS) PROM score of 1.7%), underwent exercise tolerance testing to confirm the absence of symptoms or functional limitations.2 The patients were randomly allocated to early surgical AVR (n=78) or conservative treatment, i.e., watchful waiting with guideline-directed management (n=79).1 The main exclusion criteria were symptoms confirmed by exercise, LVEF <50% at rest, very severe AS (Aortic jet velocity >5.5m/s), requiring aortic or other valve surgery, had previous cardiac surgery, and major comorbidities or life expectancy (<3 years).2 Of the 72 patients who underwent early surgical AVR, 53% and 47% received a mechanical valve and bioprosthetic valve, respectively.1 The median time from randomization to surgery in the early surgical AVR group was 55 days.1 In the conservative treatment group, 25 patients underwent surgery, and 40% of them received a mechanical valve.1 The median time from randomization to surgery in the conservative treatment group was 400 days.1 However, negative exercise testing was mandatory for inclusion as emphasized by Prof. Banovic.1
Results showed that only the MOCA-score had a significant difference between groups with a more favorable effect in patients taking warfarin (Difference of -0.96, 95% CI: -1.8 to -0.13, p=0.02). There was no difference observed between the groups at 2 years in the changes of specific cognitive domains such as memory, executive function, language, or attention as stated by Prof. Caramelli.2 It is believed larger study should be able to demonstrate difference between the two drugs, at least this trial showed us there are more mechanisms to drive cognitive decline, and that it may be more than just the choice of anticoagulation.
After a mean follow-up of 32 months, those assigned to undergo early surgical AVR had a lower rate of the primary composite endpoint than the patients assigned to a conservative strategy of watchful waiting [15.2% vs. 34.7%, HR=0.46; 95% CI: 0.23-0.9, p=0.02] (Figure 1).1
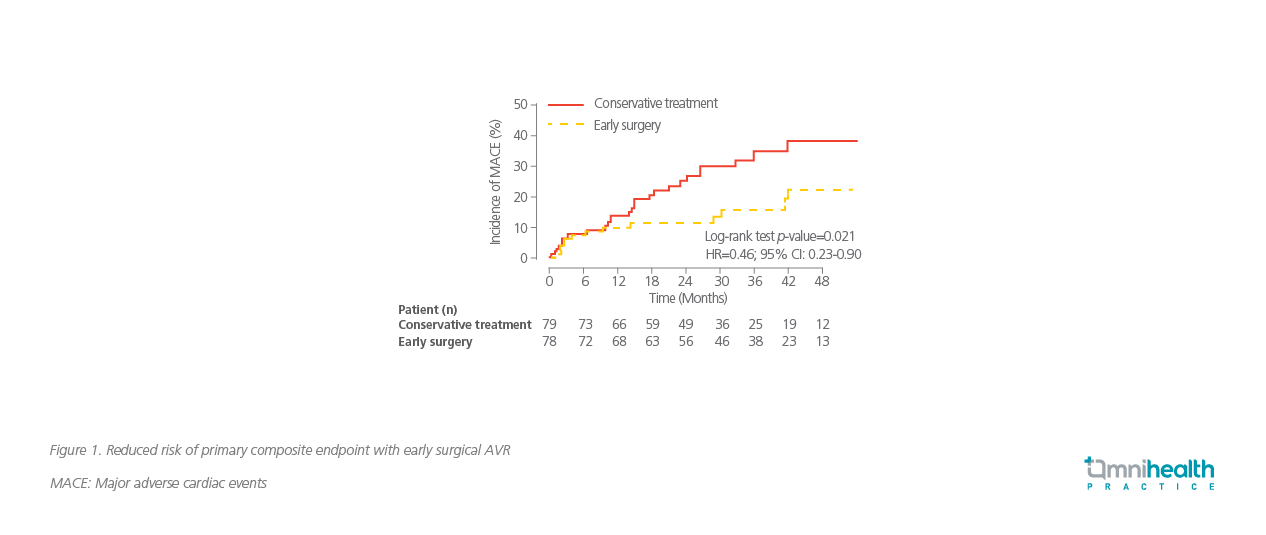
A significantly lower rate of the secondary endpoints in terms of all-cause mortality (HR=0.56; 95% CI: 0.214-1.27; log-rank p=0.16) and heart failure hospitalization (HR=0.32; 95% CI: 0.18-1.19; log-rank p=0.075) was observed in surgical AVR arm versus conservative treatment arm.2 There were no significant differences between the two arms among other secondary endpoints, which included repeated major adverse CV events [3.8% vs. 8.9%; odds ratio (OR)=0.41; 95% CI: 0.1-1.65], thromboembolic complications (2.6% vs. 2.3%; OR=1.03; 95% CI: 0.14-7.67) and major bleeding (5.1% vs. 1.3%; OR=3.52; 95% CI: 0.37-32.68).2 The rate of operative mortality in the early surgery group was 1.4% (One patient).1 Therefore, early surgical AVR in asymptomatic patients with severe AS seems to provide better clinical outcomes as compared to the conservative treatment.1
Prof. Banovic concluded “AVATAR trial has proven the benefits of early surgery in asymptomatic patients with severe, mainly degenerative AS and normal LV function, resulting in lower incidence of all-cause death, acute MI, stroke, or unplanned HF hospitalization.”

