RESEARCH SPOTLIGHT
P2Y12i monotherapy as a new and better alternative for long-term secondary prevention of CAD: The PANTHER study and case sharing
In brief
The PANTHER study, a meta-analysis of 7 randomized trials, suggested that the use of P2Y12 inhibitor (P2Y12i) monotherapy was associated with a 12% reduction in the risk of the primary composite endpoint of cardiovascular (CV) death, myocardial infarction (MI) or stroke when compared with aspirin monotherapy for the secondary prevention in patients with established coronary artery disease (CAD).1 It was also associated with a 23% relative reduction in the risk of MI. Notably, there was no increased risk of bleeding with P2Y12is vs. aspirin monotherapy.1
Background
Aspirin has been the cornerstone of secondary prevention in patients with established atherosclerotic cardiovascular disease (ASCVD) for decades.2 However, the recommended use of aspirin in this setting was mainly based on studies performed in the 1970s and 1980s.2 In recent years, a number of trials demonstrated superior ischemic protection with the addition of a P2Y12i to aspirin vs. aspirin alone, supporting the dual antiplatelet therapy (DAPT) to become a new standard of care (SoC) for the management of patients with acute coronary syndrome (ACS) or undergoing percutaneous coronary intervention (PCI).3,4 Yet, the combination therapy was shown to be associated with an increased risk of bleeding complications among CAD patients.5 Therefore, after the guideline-recommended duration of DAPT (i.e., about 3-12 months after the index coronary event), clinicians often discontinued P2Y12is so as to reduce the risk of bleeding, while keeping aspirin monotherapy for the long-term prevention of recurrent CV events.6 It was well understood that the preferential use of aspirin could be attributed to the lack of data regarding the safety and efficacy of P2Y12i monotherapy in the long-term secondary prevention of CAD.6 As such, PANTHER was conducted to compare the risks and benefits of P2Y12i and aspirin monotherapy for the secondary prevention of CAD, providing a clearer picture to clinicians regarding the most appropriate long-term antiplatelet for patients.
Methodology
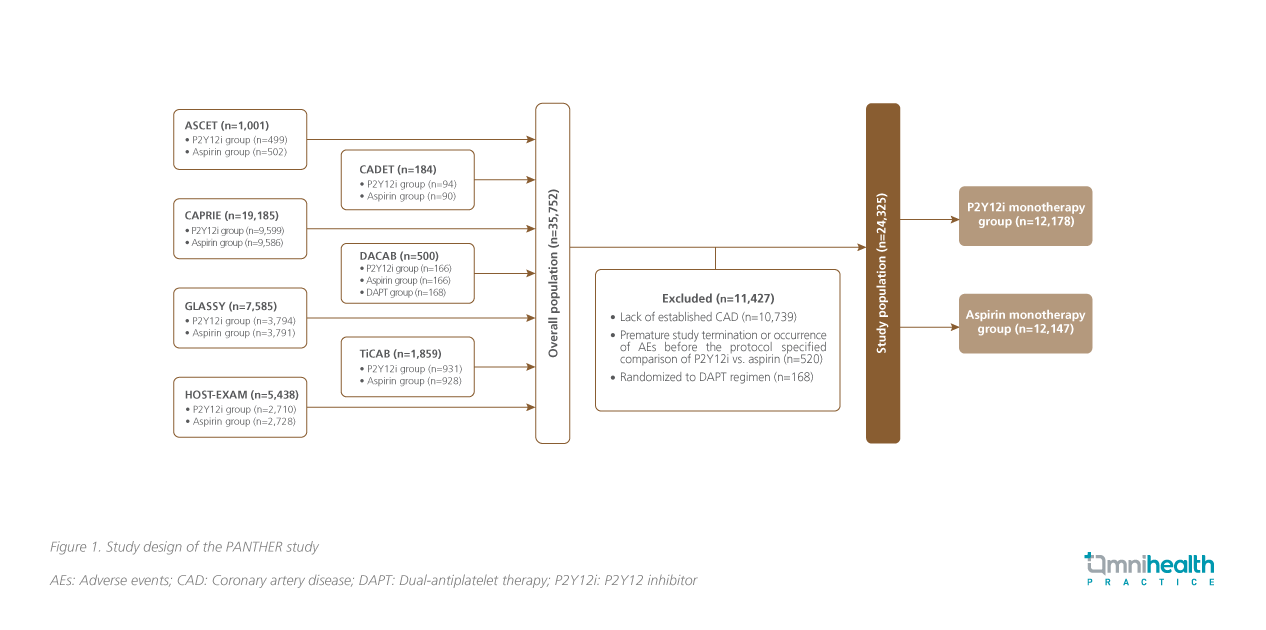
The PANTHER study was a meta-analysis of 7 randomized control trials designed to compare the efficacy and safety of P2Y12i monotherapy against aspirin monotherapy for the secondary prevention of CAD (figure 1).1 The trials included ASCET, CADET, GLASSY, CAPRIE, DACAB, HOST-EXAM, and TiCAB, involving a total of 35,752 patients with established CAD from 492 sites across 3 continents.1 Some 11,427 patients were excluded due to the lack of established CAD.1 Among the 24,325 patients who remained in the meta-analysis, 12,178 received P2Y12i monotherapy, while 12,147 received aspirin monotherapy.1
In the P2Y12i group, 62% received clopidogrel, and 38% received ticagrelor.1 The mean age of patients was 64.3 years, and 23.7% were Asians.1 Around 23.9% of patients were prescribed with proton-pump inhibitors (PPIs).1 The median treatment duration was 557 days.1 The primary efficacy outcome was a composite of CV death, MI and stroke.1 The pre-specified secondary outcomes were major bleeding and net adverse clinical events.1 Other secondary outcomes were the individual components of the primary outcome, all-cause mortality, ischemic or hemorrhagic stroke, defined and/or probable stent thrombosis, and gastrointestinal (GI) bleeding.1
Results
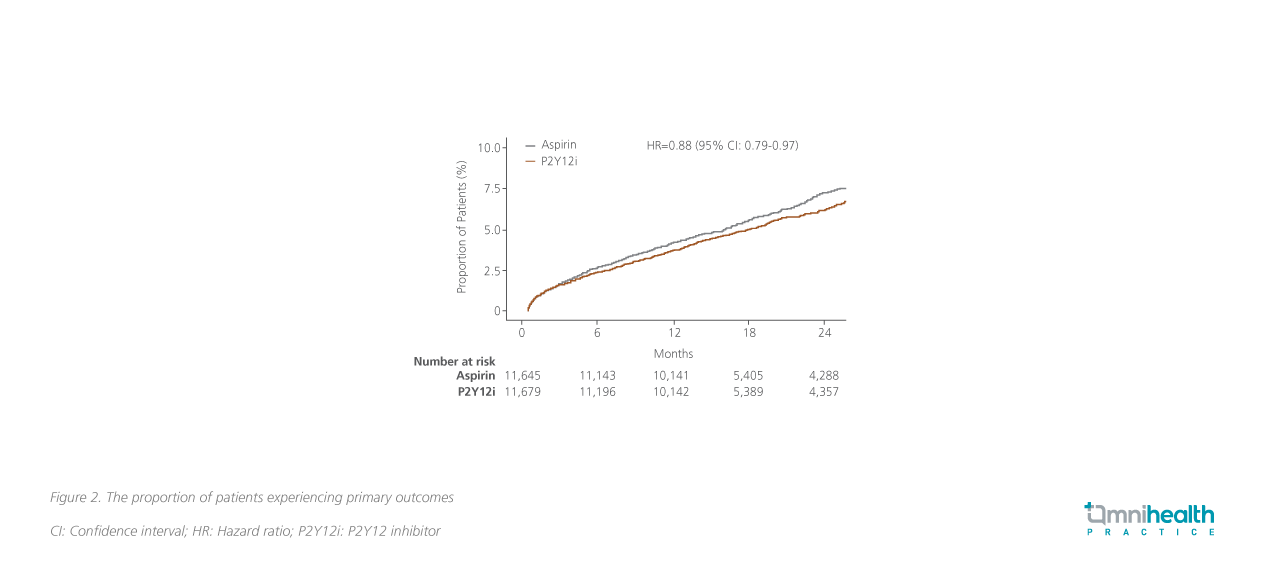
Results found that the primary outcome events occurred in 5.5% of patients receiving the P2Y12i monotherapy compared with 6.3% among those receiving the aspirin monotherapy (HR=0.88; 95% CI: 0.79-0.97; p=0.014) (figure 2).1 The number of patients needed to treat (NNT) to prevent 1 adverse event (AE) was 123.1 A subgroup analysis found that the risk reduction in primary outcome with P2Y12i monotherapy was more prominent among the Asian population vs. the overall population (HR=0.63; 95% CI: 0.46-0.87).1 For patients with prior PCI, the P2Y12i monotherapy was associated with a risk reduction of primary outcome by 30% when compared with the aspirin monotherapy (HR=0.70; 95% CI: 0.56-0.86).1
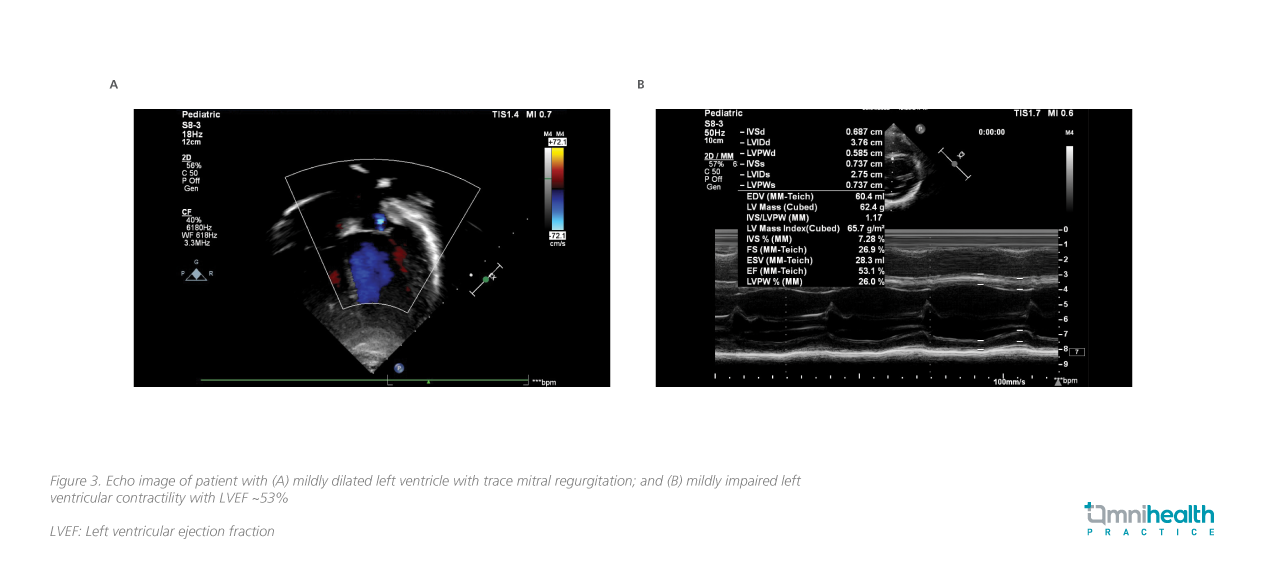
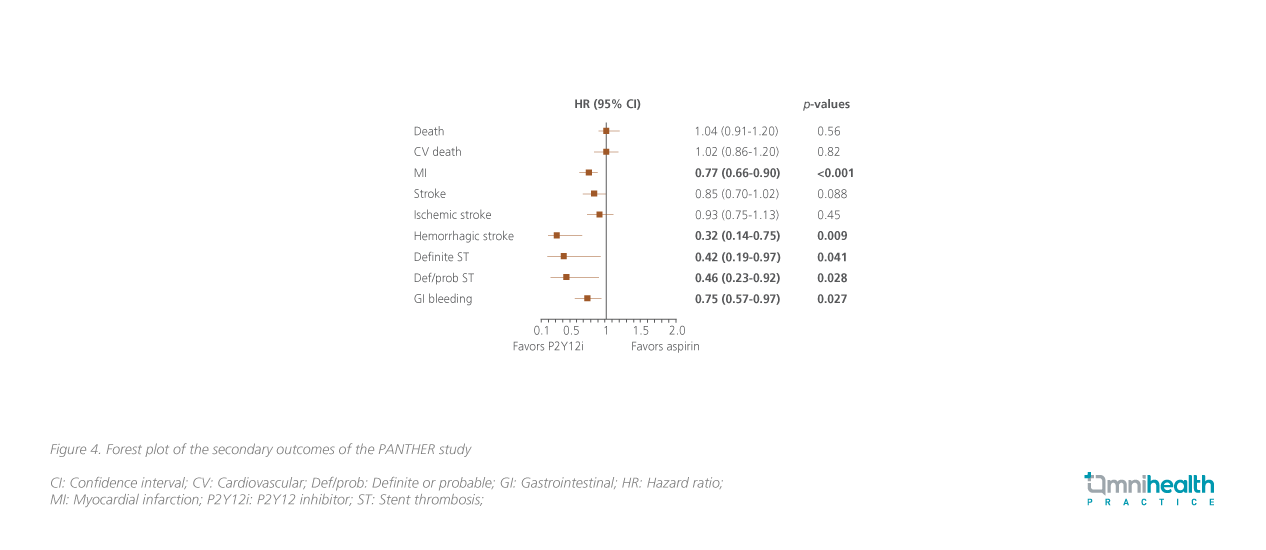
Regarding the secondary outcomes, both groups showed a comparable risk of major bleeding, with major bleeding events observed in 1.2% of patients receiving the P2Y12i monotherapy vs. 1.4% of those receiving the aspirin monotherapy (HR=0.87; 95% CI: 0.70-1.09; p=0.23) (figure 3).1 In addition, the P2Y12i monotherapy was shown to be associated with a 23% reduction in the risk of MI compared with the aspirin monotherapy, with these events occurring in 2.3% receiving the P2Y12i monotherapy and 3.0% receiving the aspirin monotherapy (HR=0.77; 95% CI: 0.66-0.90; p<0.001) (figure 4).1Additionally, the P2Y12i monotherapy also showed potential reductions in the risk of hemorrhagic stroke (HR=0.32; 95% CI: 0.14-0.75; p=0.009) and GI bleeding (HR=0.75; 95% CI: 0.57-0.97; p=0.027) when compared with the aspirin monotherapy (figure 4).1
Discussion
Dr. Hung, Yu-Tak commented that the positive findings of the PANTHER study provided new evidence and boosted clinicians’ confidence in choosing P2Y12i monotherapy over aspirin monotherapy for the long-term secondary prevention of CAD. He noted that this study included patients with similar baseline characteristics in Hong Kong and reckoned that the results were applicable to local practice. However, Dr. Hung observed that PATHNER included a higher proportion of patients having ACS when compared with patients in the local practice (60% vs. ~20%), indicating a higher ischemic risk of participants in the study.
“In fact, P2Y12i monotherapy has been widely used among local cardiologists for high-risk patients for years,” Dr. Hung said. Patients with risk factors, including smoking, diabetes, multiple-vessel diseases, multiple stents or history of acute MI, are more prone to recurrent CV events such as MI, which are generally serious or can even be life-threatening. As such, more potent P2Y12is such as ticagrelor are generally preferred for conferring a greater reduction in CV risk for these patients.
“In my practice, I always think about how to reap the ischemic benefits of the antiplatelet therapy, while keeping the risk of bleeding low,” Dr. Hung emphasized. Given the fact that P2Y12is have a potentially higher efficacy than aspirin, and the bleeding risk is generally comparable and manageable, Dr. Hung preferred continuing P2Y12i while stopping aspirin when the initial DAPT is completed. “Aspirin is not as safe as we once thought. I expect the role of aspirin in the secondary prevention of CAD will fade over time,” Dr. Hung stated.
During an interview with Omnihealth Practice, Dr. Hung shared a clinical case of a 47-year-old male with CAD whose condition was stabilized with aspirin + ticagrelor after the second PCI. This case reflected the need to treat high-risk patients with a more potent antiplatelet agent.
Case sharing
A 47-year-old male was admitted to the hospital due to complaints of chest pain and excessive sweating in May 2020. Upon initial medical examination, he was diagnosed with ischemic heart disease. He was subsequently treated with atorvastatin, aspirin and clopidogrel, and was discharged. Nevertheless, he was hospitalized again 3 days later owing to recurrent symptoms. The computed tomography (CT) scan of the coronaries suggested 60%-70% stenosis of the left anterior descending (LAD) artery. Cardiac catheterization was performed, and the intravascular ultrasound imaging identified heavy plaques burden in the LAD. PCI was performed, and a drug-eluting stent was implanted in his LAD.
After PCI, the patient was prescribed with 12-month DAPT with aspirin + clopidogrel, atorvastatin and famotidine. His condition had been stable until March 2022 when he complained of more serious chest pain radiating to jaw. Upon further investigation, transthoracic echocardiography suggested that his LAD artery was totally occluded. An electrocardiogram (ECG) also showed T-wave inversion, reflecting high-grade stenosis of the LAD. Biochemistry found a high level of creatine kinase MB (CKMB), suggestive of MI. Then, PCI was done again. The post-PCI medication was changed to aspirin + ticagrelor and ezetimibe + atorvastatin. The patient achieved a low-density lipoprotein cholesterol (LDL-C) of 1.5mmol/L and was stabilized on the DAPT of aspirin + ticagrelor for 1 year. P2Y12 antiplatelet as a monotherapy may be the best choice for his long-term secondary prevention.
Conclusion
The PANTHER study showed that P2Y12i monotherapy was associated with lower risks of CV death, MI, or stroke vs. aspirin monotherapy, while the risk of major bleeding was similar. The randomized evidence indicated the potential need for the change of SoC in the secondary prevention of CAD from long-term aspirin to more efficacious P2Y12i monotherapy. “It would be wise to consider long-term P2Y12i monotherapy rather than aspirin monotherapy among high-risk CAD patients, since aspirin is not as efficacious and safe as we once thought,” Dr. Hung agreed with the findings, adding that “Yet, PANTHER is still a meta-analysis instead of a well-controlled and randomized trial with the homogenous population.” More robust evidence is needed to confirm the role of P2Y12i monotherapy as a new and better SoC for the secondary prevention of CAD.

