CASE REVIEW
Evolocumab as added value for plaque stabilization and regression in statin-treated CAD patients
Coronary artery disease (CAD), also known as coronary heart disease or ischemic heart disease, is an atherosclerotic disease characterized by the formation of plaques on the inner walls of coronary arteries, subsequently blocking blood supply to the heart.1 CAD manifestations include stable angina, unstable angina, myocardial infarction and sudden cardiac death.2 CAD is estimated to be afflicting 126 million individuals (1,655 per 100,000) worldwide and is the most common cause of heart disease deaths in Hong Kong.3,4 Since plaque progression is associated with significantly increased cardiovascular (CV) risks in CAD patients, enormous efforts have been made to achieve plaque stabilization and regression among these patients so as to reduce the occurrence of future CV events.5,6 In an interview with Omnihealth Practice, Dr. Fung, Chi-Yan Raymond discussed the added value of evolocumab for plaque stabilization and regression in statin-treated CAD patients, as well as possible strategies to reduce CV risks in CAD patients.
Background
Clinical implications of plaque formation
Atheromatous plaque is caused by the accumulation of cholesterol, macrophages, foam cells, mineral crystals, and oxidative products, etc., in the subendothelial space due to dysfunctional endothelium.7 Formation of plaques on the inner walls of coronary arteries leads to stenosis of the blood vessels, possibly cutting off blood supply to the heart, thus resulting in CAD manifestations such as myocardial infarction.1,2 However, data have shown that the prevalence of acute coronary events may not always be associated with the degree of stenosis or plaque volume.7 Interestingly, acute coronary events could happen in CAD patients with less than 50% stenosis in the coronary blood vessels.7 This could be attributed to the rupture of the unstable plaques, called “thin-cap fibroatheroma.”7 The occurrence of plaque rupture would release its highly thrombogenic lipid content into the blood circulation, causing thrombus formation, instantly blocking the cardiac blood supply, and resulting in myocardial infarction.7 In these regards, 2 management approaches, namely plaque regression and plaque stabilization, have been proposed to reduce CV risks and the occurrence of coronary events among CAD patients with less than 50% stenosis and thin cap fibroatheroma.8
Current management approach and challenges
Currently, CAD patients with acute coronary events are managed with percutaneous coronary intervention (PCI). However, PCI is usually performed on the culprit lesion only, and the success of PCI depends on the stability of the culprit plaque. Therefore, pharmacological treatment with lipid-lowering agents before or after PCI might be warranted to stabilize the culprit lesion and prevent rupture of non-culprit plaques. Statin, a lipid-lowering agent and the current standard of care for CAD risk management, demonstrated their efficacy in plaque regression and stabilization among CAD patients from several studies.9 Robust evidence has also shown that statin was effective in reducing CV events in CAD patients with elevated CV risks.9 However, many CAD patients, despite optimal treatment with statins, still experience recurrent CV events.9 This implied that statin alone might not be sufficient to mitigate CV risks in CAD patients. According to the results of a meta-analysis study, plaque progression was halted at a low-density lipoprotein cholesterol (LDL-C) threshold of 1.94mmol/L, and the reduction of plaque burden started to occur when the LDL-C levels were lowered to <1.8mmol/L.10 Therefore, combination lipid-lowering therapy with statin and non-statin therapeutic agents is warranted to achieve a sufficiently low level of LDL-C in order to start showing the effect of plaque regression and stabilization.
Demand for non-statin, lipid-lowering and highly efficacious drugs
Evolocumab, a proprotein convertase subtilisin/kexin 9 (PCSK9) inhibitor, is one of the options. In combination with maximum tolerated statin, evolocumab is indicated for treating adults with established atherosclerotic CV disease to reduce CV risks by lowering LDL-C levels.11 “There were studies showing that evolocumab was effective in inducing plaque regression and stabilization due to its prominent lipid-lowering effect,” said Dr. Fung. To illustrate the role of evolocumab in CAD management, Dr. Fung shared a clinical case of an acute coronary syndrome (ACS) patient.
Case report
A 50-year-old man was hospitalized due to complaint of chest pain. His medical history is notable for diabetes mellitus type 2, hypertension, dyslipidemia, and smoking prior to hospitalization. The initial medical examinations found xanthomas in the patient’s eyelids and thickened Achilles tendons (i.e., tendon xanthomata). The blood test result showed an elevated level of troponin, indicating the presence of heart injury. Although the patient has been taking atorvastatin 10mg once daily for his dyslipidemia treatment, the serum LDL-C level was found to be at a high level of 4.4mmol/L. The angiograms showed a serious narrowing in the left anterior descending artery (LADA) and a 40% stenosis in the right coronary artery (RCA). PCI was warranted for his stenotic LADA and was performed immediately. Further examination on the RCA by optical coherence tomography (OCT) using near-infrared light showed the presence of lipid-rich plaques with a thin fibrous cap (<65µm), implying that he was at risk of plaque rupture and future acute coronary events. The Dutch Lipid Clinic Network Score (DLCNS) of this patient was greater than 8. According to the dyslipidemia management guidelines, an aggressive lipid lowering therapy to achieve a targeted LDL-C level below 1.4mmol/L should be adopted. Therefore, a regimen of high-dose statin and ezetimibe was prescribed. However, LDL-C level remained high at 3.5mmol/L after 3 weeks of high-dose statin and ezetimibe treatment. Considering the situation, evolocumab was added on top of the initial treatment. Approximately 4 weeks later, LDL-C level was greatly lowered to 1.01mmol/L.
After undergoing PCI and receiving aggressive lipid-lowering triple therapy, the patient’s condition was stabilized, and he no longer complained of chest pain. Since there is no more concern over his cardiac condition, he was encouraged to exercise more and establish a healthy and “heart-friendly” lifestyle. No adverse event regarding the use of evolocumab was reported by this patient.
Discussion
Preventing future CV events is the major management goal for ACS patients. PCI is the first-line management approach if the angiograms show a stenosis of >50% in the coronary arteries. However, PCI is often performed on culprit lesions only, while leaving the non-culprit lesions untouched. This will leave the patients at high risk of future acute coronary events since non-culprit plaques could rupture and lead to thrombus formation if the fibrous cap of the plaque is too thin (i.e. <65µm). In addition, success of PCI depends on the stability of the plaque. Therefore, achieving plaque stabilization as well as plaque regression among ACS patients is vital.
It is not a common practice in Hong Kong to perform the post-PCI atherosclerotic imaging to assess the plaque status. However, given the serious consequences of plaque rupture, preventive measures should be adopted to achieve plaque stabilization. Some Japanese real-world studies have shown that intensive lipid-lowering treatment could achieve plaque stabilization and even regression in ACS patients with any degree of stenosis no matter whether they will undergo PCI or not.12,13 The results of these real-world studies showed that those ACS patients who achieved plaque regression had a lower rate of cardiovascular events, a low rate major adverse cardiac and cerebrovascular events, a significantly higher rate of event-free survival.12,13
Plaque stabilization and regression can be achieved through intensive lipid-lowering therapy with high-dose statin and evolocumab. The efficacies of evolocumab in plaque stabilization and regression were demonstrated by two randomized clinical trials below:
The GLAGOV study: Efficacy of evolocumab on plaque regression
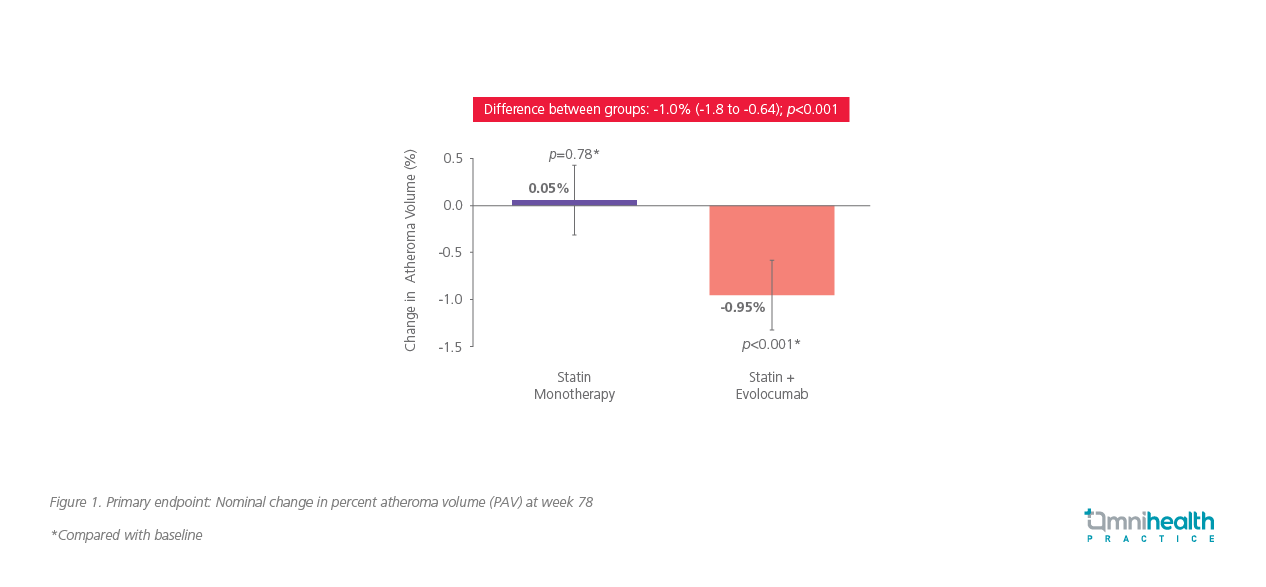
A multicentered, randomized clinical trial, the GLAGOV study, was performed to evaluate the efficacy of evolocumab in plaque regression.14A total of 968 patients with angiographic coronary disease were recruited.14 These patients were randomly assigned into the study group receiving monthly evolocumab 420mg subcutaneous injection and maximally tolerated statin, and into the control group with placebo and statin.14 The efficacy of evolocumab for plaque regression was evaluated by the nominal change in percent atheroma volume (PAV) from baseline to week 78, using serial intravascular ultrasonography (IVUS) imaging.14
During the 76-week treatment, the evolocumab group achieved a significantly lower LDL-C level than the placebo group (0.95mmol/L vs. 2.40mmol/L), with a difference of 1.46mmol/L (95% CI: 1.38-1.54).14 The PAV was decreased by 0.95% (p<0.01, compared with baseline) in the evolocumab group and increased by 0.05% (p=0.78, compared with baseline) in the placebo group.14 The difference of the nominal change of PAV between the 2 groups was -1.0% (95% CI: -1.8% to -0.64%; p<0.001) (Figure 1).14
A post-hoc analysis of the study revealed that patients with baseline LDL-C levels <1.81mmol/L would have a more favorable effect on the change in PAV with the evolocumab treatment (-1.97% vs. -0.35% in the placebo group).14 The between-group difference was -1.62% (95% CI: -2.5%-0.74%; p<0.001).14
The HUYGENS study: Efficacy of evolocumab on plaque stabilization
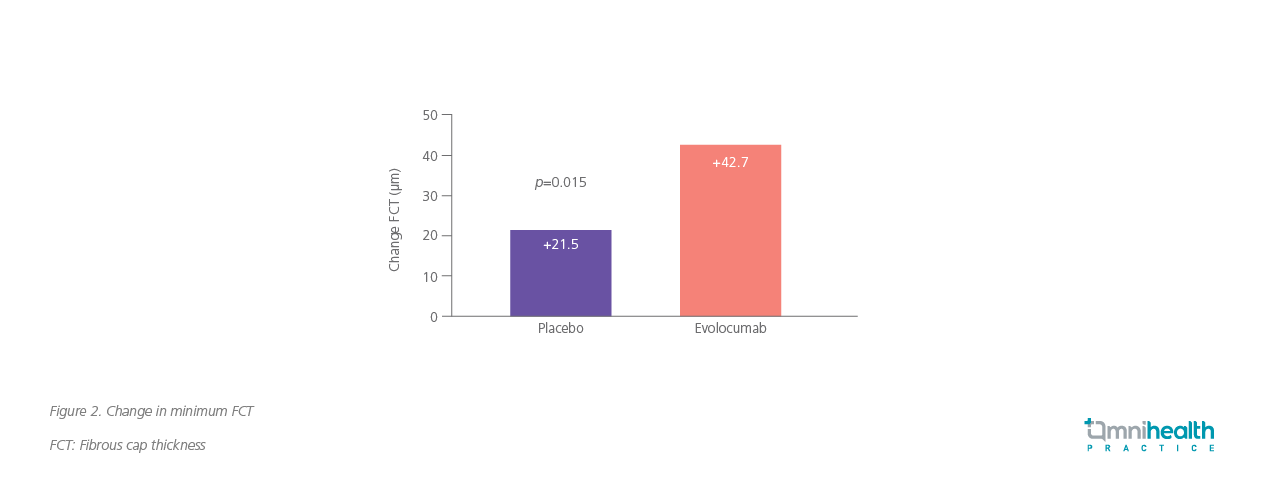
As for plaque stabilization, evolocumab’s efficacy has been shown by the HUYGENS study which aimed to determine the impact of adding evolocumab to statin therapy on plaque phenotype in patients who have experienced ACS.15 About 160 patients with non-ST-elevation myocardial infarction (NSTEMI), LDL-C ≥1.55mmol/L on high-intensity statin or ≥2.07mmol/L on low-to-moderate-intensity statin or ≥3.36mmol/L without statin therapy, and coronary angiography showing 20%-50% stenosis in target blood vessels, were recruited.15 These patients were subsequently given maximally tolerated dose of statin and were randomly assigned into the study group with evolocumab and statin, and into the control group with placebo and statin.15 The baseline LDL-C levels of the evolocumab group and placebo group were 3.63mmol/L and3.67mmol/L, respectively.15 The minimum fibrous cap thickness (FCT) of plaques, measured by OCT, of the 2 groups were also similar (56.6µm vs. 54.6µm).15 The efficacy of evolocumab for plaque stabilization was evaluated by the change in minimum FCT.15
After 50-weeks treatment, evolocumab group achieved a significantly lower LDL-C level of 0.73mmol/L from 3.63mmol/L, compared with 2.25mmol/L attained by the statin plus placebo group from 3.67mmol/L.13 The minimum FCT was increased by 42.7µm in the evolocumab group, while the increase was only 21.5µm in the statin plus placebo group (p=0.015) (Figure 2).15
The relationship between LDL-C level and the change in FCT, was established.13 As shown in Figure 3, lowering LDL-C levels increased FCT, and FCT continued to thicken without plateau even when LDL-C was as low as 0.3mmol/L.15 On the other hand, thickening of the fibrous cap became more obvious when the decrease in LDL-C level was greater than 1.55mmol/L (Figure 4).15


Conclusion
The most common cause of ACS in CAD patients is plaque rupture. The risk of recurrent coronary events is particularly higher in patients who have experienced ACS before. Since there was evidence showing that treatment with statin alone might not be sufficient in lowering LDL-C level and reducing CV risks among CAD patients, the addition of a highly efficacious, non-statin drug into the lipid-lowering treatment is needed. Given the benefits in plaque regression and stabilization as shown by the two randomized clinical trials, evolocumab is likely an ideal treatment option for the CAD patients for reduction of CV risks and prevention of future coronary events.

