RESEARCH SPOTLIGHT
Awake prone positioning in the pandemic era: A potential alternative to prevent IMV in patients with respiratory failure
In brief
The 18-day single-center experience of awake prone position (APP) in patients admitted to the intensive care unit (ICU) of Pamela Youde Nethersole Eastern Hospital in Hong Kong (PYNEH) with severe acute respiratory syndrome coronavirus 2 (SARS-CoV2) infection demonstrated the effectiveness of APP in improving respiratory parameters, minimizing the use of invasive mechanical ventilation (IMV), and potentially providing a low-cost and safe treatment option for patients with respiratory failure.1
Background
Acute respiratory distress syndrome (ARDS) is a life-threatening condition of critically ill patients, characterized by severe progressive hypoxemia in the absence of any evident cardiogenic pulmonary edema, and is defined by patients’ PaO2/FiO2 ratio of less than 300.2 Its incidence has increased during the COVID-19 pandemic, in which 17-41.8% of patients presenting with COVID-19 pneumonia developed ARDS, and 5-32% required intensive care.3-7 This has significantly diminished intensive care resources and added to the burden of healthcare workers worldwide.8 For example 60% of the total ICU capacity in the public hospitals was taken up by the critically ill COVID-19 patients in Hong Kong.1 Among patients with moderate-to-severe ARDS, IMV is often needed for life support.9 Nevertheless, IMV can be associated with ventilator-induced lung injury (VILI), ventilator-associated pneumonia (VAP) with increased mortality. The high mortality of 42.1% was observed among intubated COVID-19 patients in ICU of PYNEH, and other series.1,8 In addition, IMV may not be available in medical centers or hospitals with resource constraints when the number of patients in need of intensive care is high.
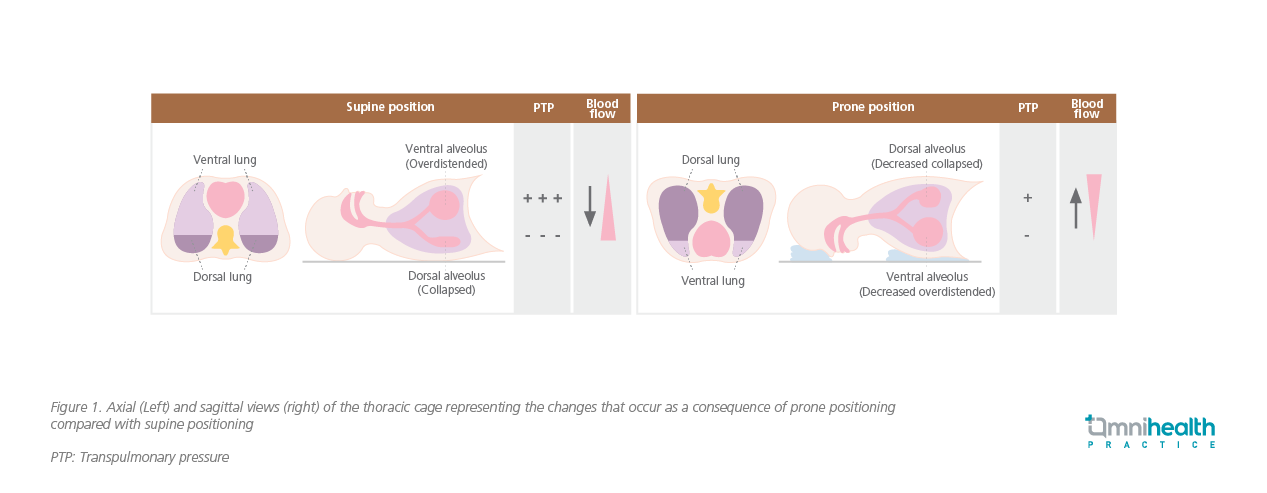
Given the serious complications from IMV and its resource implication, a safe, effective and lower-cost alternative is warranted to prevent the use of IMV. Prone positioning (PP) is one of such possible options. PP is a technique to improve gas exchange and has been used for the treatment of severe hypoxemia in patients with ARDS since 1970s.10 Compared with supine position (SP), PP reverses the vertical pleural pressure gradient, which becomes less positive in the dorsal regions of the lung, thus effecting a more even tidal volume distribution in patients and resulting in an improved overall alveolar ventilation and ventilation-perfusion matching (Figure 1).10 Its clinical efficacy has been consistently reported by more than 40 years of clinical trials which showed that oxygenation status was improved in about 70% of ARDS patients with survival benefit, with the earlier initiation of PP, the better clinical outcomes.10,11 That said, existing data are mostly derived from patients who have already been intubated, while the literature for non-intubated patients is relatively less available.8
In light of this, enormous efforts have been put into testing PP in non-intubated, spontaneously breathing, COVID-19 and non-COVID-19 patients, a technique which is now known as APP, for its effectiveness in reducing ICU admission and IMV use in recent years.12 Several overseas studies have shown the promising results of APP in improving oxygenation and respiratory rate in ARDS patients, especially when combined with non-invasive ventilation or high-flow nasal cannula (HFNC).12 The positive findings of the studies in APP have attracted Dr. Man’s and Dr. Lam’s attention and interest since this technique has never been tested locally and is not commonly used in Hong Kong before the COVID pandemic. Due to its low-risk and low-cost nature, Dr. Man et al. believed that proving its effectiveness with a local study and applying it in local clinical practice would certainly be beneficial to both patients as well as alleviating the local health burden. Hence, they conducted a retrospective, single-center study at the ICU of PYNEH to confirm its potentially prominent results on local COVID-19 patients with respiratory failure.1
Methodology
This single-center study is by far the first APP study in non-intubated COVID-19 patients with respiratory failure in Hong Kong.1 In this study, the medical records and data in clinical management and information systems of COVID-19 patients admitted to ICU of PYNEH between 28 Nov-15 Dec 2020 were retrospectively reviewed.1 The laboratory and respiratory parameters that have been analyzed included oxygen saturation (SpO2), partial pressure of oxygen (PaO2), fraction of inspired oxygen (FiO2), partial pressure of carbon dioxide (PaCO2), respiratory rate, and respiratory rate-oxygenation (ROX) index.1 The overall rates of intubation, ICU mortality, and hospital mortality among patients with or without APP were also assessed.1
Results
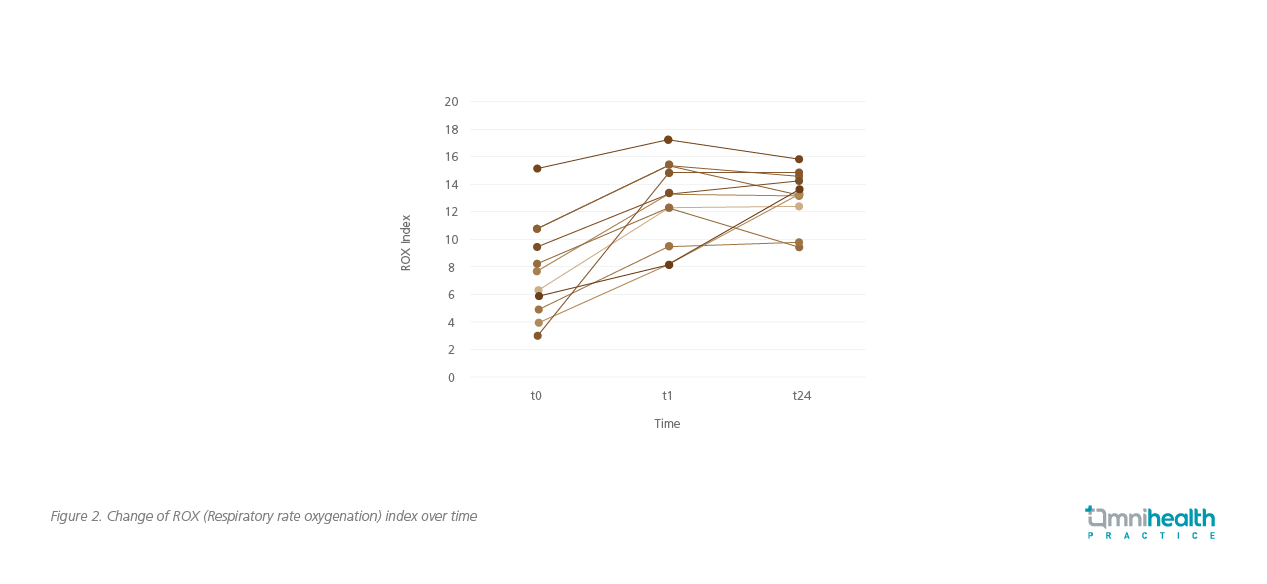
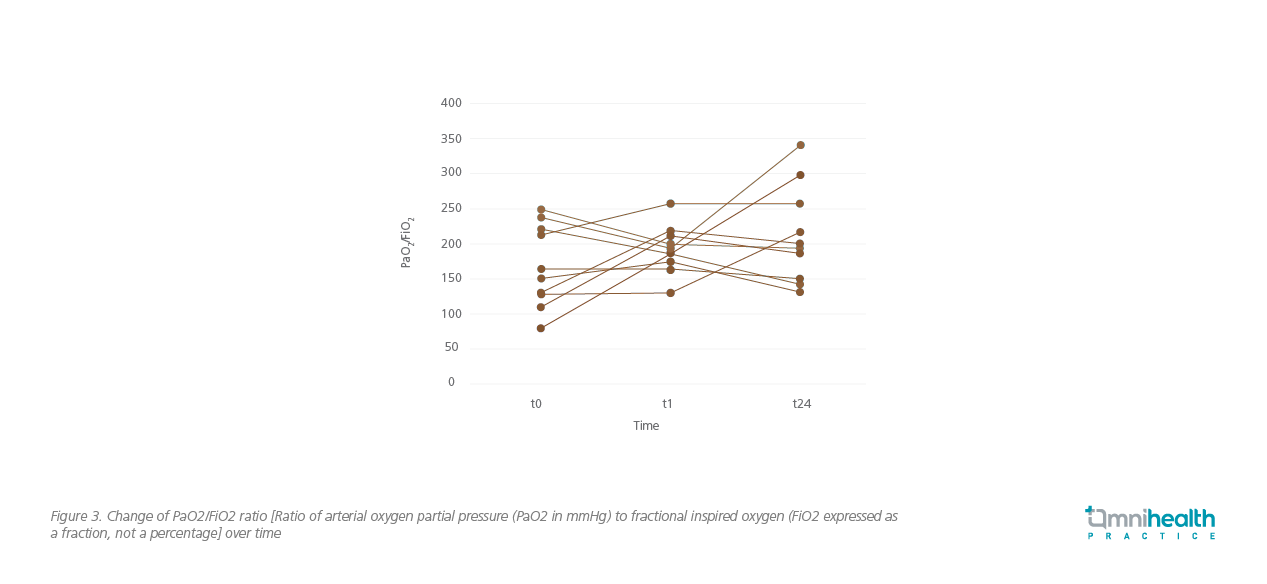
A total of 18 patients were included in this study. Among them, 11 patients received awake APP, while the remaining 7 patients had either been intubated already or were unable to cooperate with the healthcare workers.1 For patients with APP, the median duration of APP was 18 hours.1 Significant improvement in SpO2 (95% vs. 92%, p=0.008), FiO2 (0.4 vs. 0.5, p=0.003), SpO2/FiO2 (240 vs. 184, p=0.005), respiratory rate (19 vs 26, p=0.006), and ROX index (13.22 vs. 7.67, p=0.003) (Figure 2) was observed 1 hour after proning.1 PaO2, PaCO2, and PaO2/FiO2 (Figure 3) were also improved.1 The ICU mortality and hospital mortality for patients with APP were much lower than the patients without APP (9.1% vs. 42.9%, and 18.2% vs. 42.9%, respectively).1 In terms of safety, APP was well tolerated. 2 patients developed grade 1 pressure sore on the chin and face.1 However, no major hemodynamic compromise or dislodgements of important tubing or lines were observed.1
Discussion
This local study has demonstrated improvement in respiratory parameters and a favorable trend towards low rates of intubation and ICU mortality among the non-intubated COVID-19 patients with respiratory failure in Hong Kong, echoing the positive findings of previous APP studies and highlighting APP’s potential for wider application in local clinical practice for preventing the use of IMV in COVID-19 patients with respiratory failure. Its application in non-COVID-19 patients with respiratory failure warrants further investigation.
Despite the demonstrated benefits, Dr. Man and Dr. Lam suggested the treatment decision on the use of APP in clinical practice should be made on a case-by-case basis. The current management approach for intubated patients with ARDS is mainly supportive with an aim to maintain the patients’ oxygen saturation level using minimal amount of oxygen to achieve a target between 88% to 96%, and plateau pressure <30cm H2O.13 Additionally positive end-expiratory pressure (PEEP) should be ≥5cmH2O, adjusted with tidal volume to minimize driving pressure, respiratory rate can be increased to maintain an acceptable minute ventilation after removing unnecessary instrumental dead space, and permitting hypercapnia in the absence of right heart failure or raised intracranial pressure.13 APP with or without HFNC could serve as a feasible initial option in patients with ARDS. With awake prone positioning, patients’ abilities to ingest, speak and mobilize are retained. This is beneficial to their overall quality of life and is crucial to their rehabilitation. With its potential effectiveness to reduce the demand for IMV, the strain on ICU resources could be lowered. Preventing intubation can also reduce the infection risk for healthcare workers. Nevertheless, they still highlighted the importance of timely escalation to higher levels of management approach, particularly IMV, if the non-intubated patients have insufficient response to APP. Treatment escalation should be based on close monitoring of patients’ clinical responses and assessment on patients’ condition. Although IMV can be associated with ventilator-induced lung injury and ventilator-associated pneumonia, it should not be delayed in patients who fail non-invasive support. In the meantime, Dr. Man and Dr. Lam stressed that it is crucial to investigate the underlying etiology of ARDS so as to identify the causative agents and to have them treated.
This study had several limitations. First, there was no standardization in intubation criteria, and the decision to proceed with IMV was mainly based on physicians’ clinical judgment. Second, validated methods to assess patients’ comfort and compliance were not utilized. Medications including analgesics and sedatives were used when necessary to minimize discomfort from APP and to facilitate prone positioning. Finally, although there was statistically significant improvement in respiratory parameters, the favorable trend towards lower rates of intubation and ICU mortality were not statistically significant due to the small sample size. Therefore, future randomized controlled studies to verify the effectiveness of APP in the local population, as well as to address the uncertainties of APP such as optimal APP duration, initiation time, treatment endpoints, predictors of responders, are warranted.
Conclusion
All in all, APP was shown to have improved the respiratory parameters of non-intubated patients with respiratory failure. Although not all the findings were statistically significant due to small number of participants, a favorable and promising trend towards lower mortality and intubation rates were observed in this local study. Given its relative ease of use, fairly low incidence of adverse events, APP has been adopted and extensively studied in COVID-19 patients with respiratory failure in other countries.14 It is anticipated that, with more high-quality evidence becoming available, adoption of APP in local clinical practice can be realized in a foreseeable future and will be beneficial to patients and the healthcare system.

