MEETING HIGHLIGHT
Scalable solutions for mid-tier obesity: Revisiting the role of IGBs
With obesity and metabolic syndrome reaching alarming levels in Malaysia, clinicians are looking beyond conventional approaches to expand the bariatric toolbox.1,2 Among the emerging options, intragastric balloons (IGBs) are gaining momentum as a minimally invasive, endoscopic solution to support the initial step in weight loss alongside lifestyle change.1-3 At the recent “Intragastric Balloon” workshop hosted by the Department of Surgery, Hospital Canselor Tuanku Muhriz (HCTM) UKM in Kuala Lumpur, leading experts in bariatric innovation shared their perspectives on advancing IGB therapy in clinical practice. Dr. Jeffrey Brooks, inventor of the Spatz adjustable IGB system, outlined the evolution of balloon technology and its unique clinical edge; Professor Dato’ Nik Ritza Kosai Nik Mahmood, senior consultant and head of the hospital’s upper gastrointestinal and metabolic surgery unit, highlighted the integration of IGBs with pharmacologic therapies into care pathways; while Dr. Loo Guo Hou, general and bariatric surgeon at HCTM UKM, underscored the pivotal role of lifestyle modification and structured follow-up in translating short-term outcomes into sustainable long-term success.
The role of gastric volume in obesity: Evolution of IGB technology
Obesity is recognized as a complex, chronic disease associated with increased risks of diabetes, hypertension, cardiovascular disease, and other comorbidities.4 Central to its pathophysiology is excessive caloric intake, often associated with an enlarged fasting gastric capacity.5 One intuitive intervention is gastric volume reduction, achieved either through surgical resection or via space-occupying devices that create a sense of fullness.5 IGBs, first introduced in 1982 by Nieben, are designed on this principle, reducing gastric capacity, modifying gastric emptying and accommodation, and thereby stimulating satiety to curb caloric intake.1,5 For patients with obesity (body mass index [BMI] 30-40kg/m²) who have not responded to lifestyle modifications alone, the American Gastroenterological Association (AGA) recommends IGBs in combination with supervised behavioral therapy.6
The development of IGB technology reflects decades of innovation aimed at improving safety, tolerance, and patient convenience.7 The first generation of IGBs introduced in the 1980s was associated with severe complications such as balloon deflation and migration, leading to early market withdrawal.7 This prompted the emergence of safer designs, notably saline-filled silicone balloons inserted and removed endoscopically.7
Modern advancements have transformed the landscape, introducing more patient-friendly options.7 In this context, IGBs can be classified both by adjustability, whether the balloon volume can be modified after placement and by their placement method, which may be endoscopically or via a swallowable capsule.3,5 Building on this framework, the latest innovation involves swallowable balloons, encapsulated in a small capsule attached to a thin catheter.5,7 Once ingested, their position in the stomach is confirmed radiographically, after which the balloon is inflated and the catheter removed.5,7 Uniquely, one of these balloons is designed to spontaneously deflate and pass naturally through the gastrointestinal tract after four months, thereby eliminating the need for an endoscopic removal procedure (figure 1).5,7,8
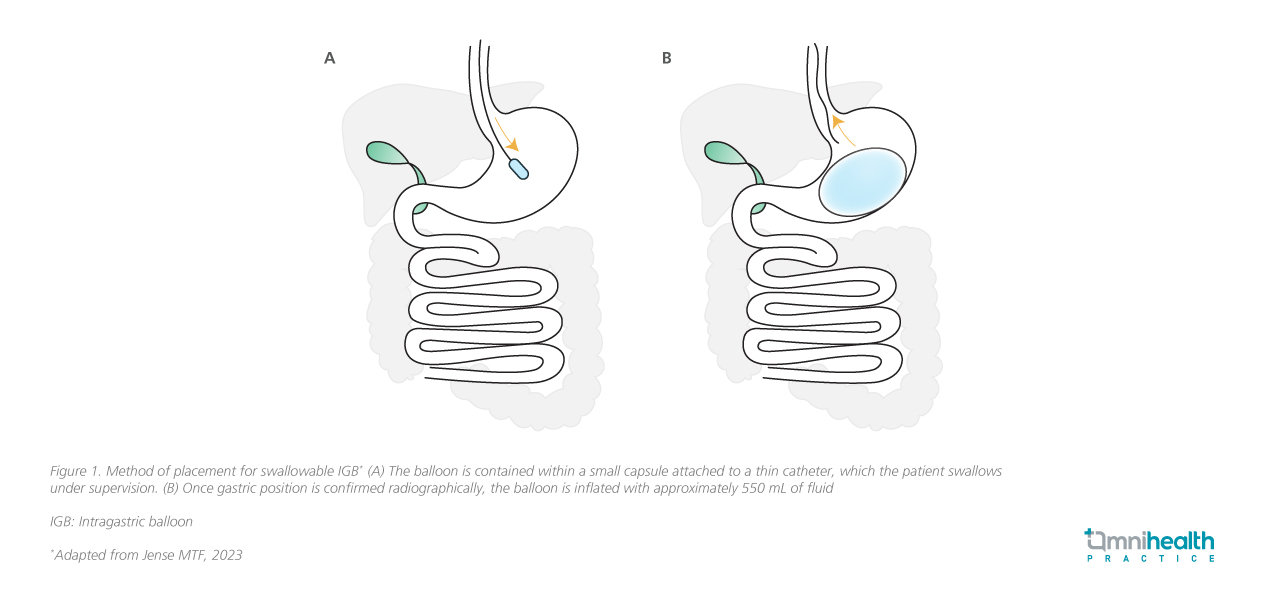
In Malaysia, swallowable IGB has emerged as a favored choice for non-surgical weight loss.9 It offers the key advantage of not requiring anesthesia or endoscopy for placement or removal—patients can simply swallow it, and it self-deflates after four months.4,9 This makes it particularly appealing to patients, offering enhanced practicality and ease of use.9 However, by forgoing pre-implantation endoscopic screening, there is a risk of missing mucosal lesions (such as erosions or ulcers) or anatomical abnormalities (like a hiatus hernia), which could potentially increase the risk of complications during therapy.4 Therefore, careful patient selection and pre-placement screening using imaging or detailed history-taking are essential to minimize risks.3 In terms of weight loss outcomes, swallowable balloons have demonstrated a TBWL of around 12-14% at four months, which is significant compared to lifestyle modification alone.5
While no single tool is a panacea for obesity, IGBs are uniquely positioned to fill the gap between lifestyle interventions and bariatric surgery.5 Their minimally invasive nature and flexibility in design make them especially valuable in resource-diverse settings.5 “In Malaysia, the resurgence of interest in IGB therapy is fueled by growing patient awareness and the introduction of newer devices, such as adjustable and swallowable IGBs”, shared by Prof. Nik.
Personalized volume adjustments: A game changer in IGB tolerance and long-term success
Another significant advancement is the development of adjustable IGB (aIGB), which permit volume adjustments throughout the treatment period and enable longer therapy duration.7 Traditional static-volume IGBs often fail to accommodate the variability in patient anatomy, gastric tolerance, and satiety thresholds.12 These limitations can lead to early intolerance or premature device removal, particularly within the initial weeks post-implantation.12 Additionally, the therapeutic efficacy of static balloons tends to decline after 3-5 months, potentially leading to weight regain even while the device remains in place.12,13
Building on the foundational concept of gastric volume reduction, Dr. Brooks further explored the clinical rationale behind aIGB. This fluid-filled silicone balloon includes a thin, removable catheter that enables clinicians to modify balloon volume in situ, not only at implantation, but throughout the full treatment period.5 The adjustability offers several key advantages.12 In cases of significant post-procedural intolerance, a down-adjustment can reduce gastric distension and alleviate symptoms such as nausea, vomiting, abdominal discomfort, or acid reflux, allowing patients to stay on track and avoid unnecessary early removal.5,12 Additionally, an up-adjustments several months into therapy can also help overcome weight loss plateaus and enhance the satiety effect, extending the clinical benefits of the balloon.12
Dr. Brooks noted that while a typical inflation volume is 500mL, tailoring this to patients’ body habitus is critical; for example, more compact or shorter individuals may start at 400mL to minimize intolerance without compromising effectiveness. He also addressed rare technical complications, such as balloon hyperinflation due to microbial contamination, which can be managed in adjustable systems by deflating and replacing the saline without full device removal. However, he cautioned against frequent or late-stage volume changes, emphasizing IGBs are short-term tools to support behavioral change, not as a permanent fix. With a maximum implantation period of 12 months, the longest of any approved IGB, the adjustable device offers a longer therapeutic window for patients to engage in dietary re-education and lifestyle modification.5 Clinical evidence demonstrates that adjustable IGBs can achieve up to 15% total body weight loss (TBWL) at 32 weeks, significantly outperforming lifestyle interventions alone.4 Furthermore, the “up-adjustment” procedure, commonly performed around 18 weeks, can deliver an additional 5.2% TBWL, enhancing overall outcomes.4
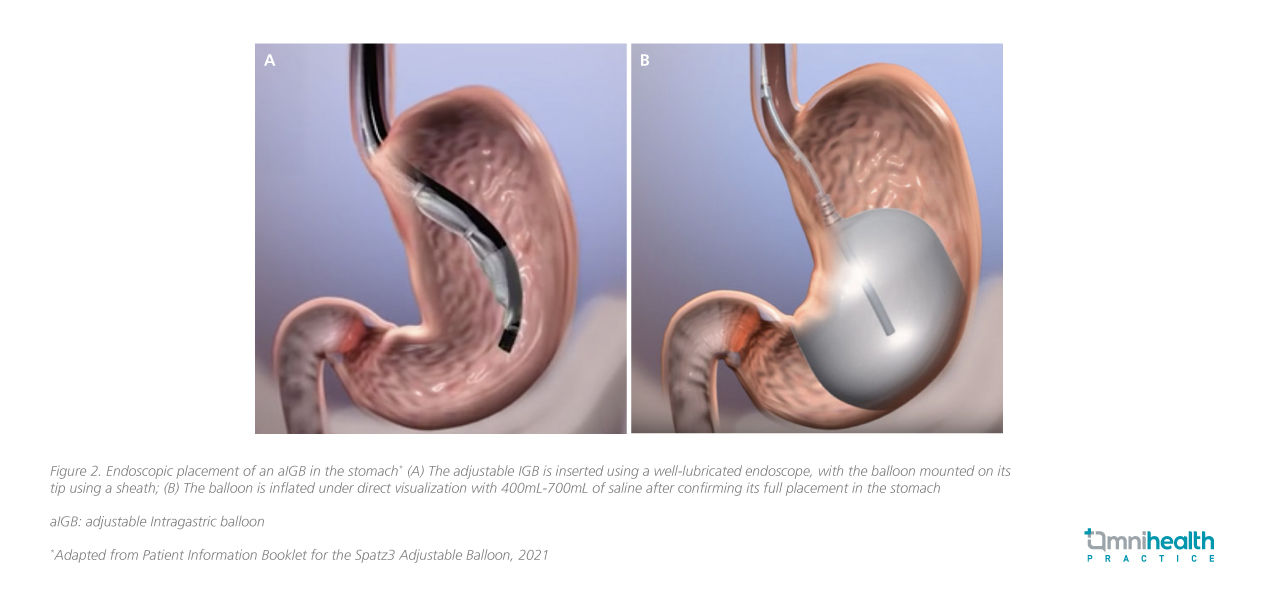
In clinical practice, each type of IGB follows distinct placement and removal protocols.10 For example, non-swallowable IGB placement is typically performed endoscopically under sedation, with the balloon introduced into the stomach and filled with 400mL-700mL of saline mixed with methylene blue (figure 2).5,11
Beyond the balloon: Clinical insights on patient management and sustainable weight loss
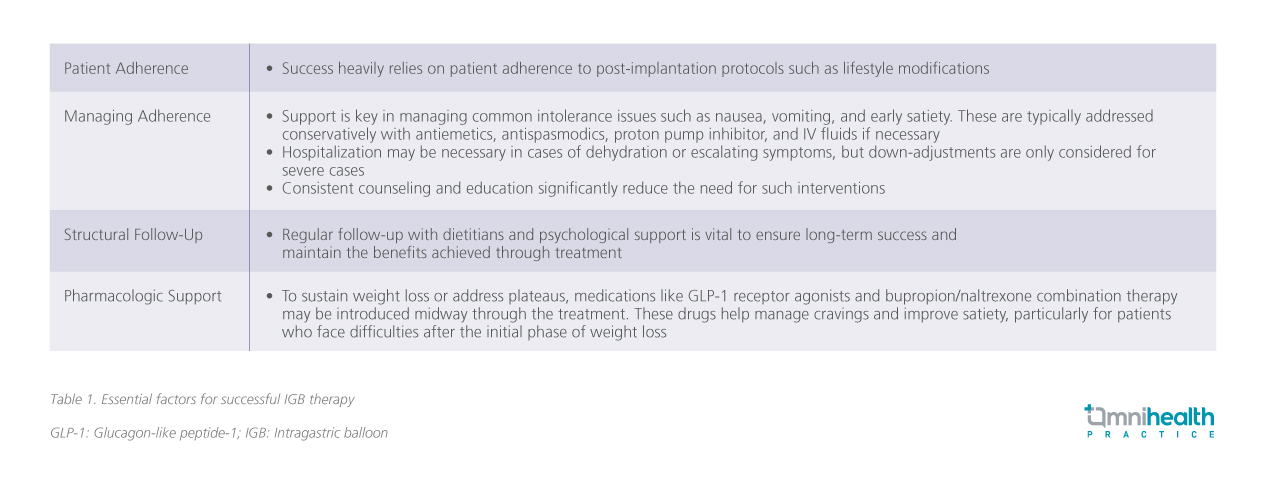
Clinical experience at HCTM, as shared by Prof. Nik, demonstrates that both adjustable and swallowable IGBs can lead to significant weight loss, with some patients achieving up to 20% TBWL. Beyond initial results, he emphasized practical strategies to support long-term weight maintenance, underscoring the importance of integrating IGB therapy with structured lifestyle interventions and ongoing clinical support (table 1).
Lifestyle modifications play a crucial role in supporting weight loss and long-term success following IGB placement.14 As Dr. Loo explained, “The balloon is only the first step. The real transformation comes when patients commit to healthier routines that last beyond the device itself.” Following the early adjustment phase, patients gradually progress from a puréed diet to a soft diet, and eventually to regular meals, allowing the stomach to adapt comfortably to the IGB.10 Long-term success, however, depends on more than the device itself—it requires sustainable lifestyle changes that continue well beyond balloon removal.14
Patients are encouraged to follow a balanced, hypocaloric diet designed to create a daily deficit of around 1,000kcal, typically ranging from 800-1,400kcal per day based on individual energy expenditure.14 Keeping detailed records of food intake and physical activity helps reinforce healthy habits, while aiming for at least 30 minutes of moderate exercise five days a week supports ongoing weight control.14 Walking, jogging, swimming, cycling, or aerobic ball games are all suitable options.14
Underscoring the value of structured follow-up, Dr. Loo noted, “Regular visits, ideally every four weeks with the same physician and nutritionist, allow us to troubleshoot challenges early, keep patients motivated, and ensure the results are not just temporary but sustainable.” Such consistent support helps patients translate short-term results into lasting change.14
Lastly, Dr. Brooks offered a insightful analogy: the balloon is not a calorie-burning device or a punitive mechanism, but rather a “personal trainer whispering in your ear.” It helps patients recognize early satiety cues such as mild bloating or belching, before more overt signals like nausea or vomiting appear. Encouraging this mindful approach shifts responsibility to the patient and supports sustainable behavioral change.
Conclusion
In conclusion, IGBs serve not only as a catalyst for weight loss but also as a tool for cultivating self-awareness in eating behaviors.14 The paradigm for obesity management is evolving to resemble chronic disease models, integrating short-term interventions like IGBs for initial weight reduction with long-term pharmacotherapy and lifestyle measures to maintain success.3 When paired with structured lifestyle changes and ongoing support, it can help transform short-term results into sustainable, long-term success and help close the widening gap in obesity treatment strategies.3,14

