EXPERT INSIGHT
HFNC oxygen supplementation and SF ratio prognostication in the COVID-19 pandemic
To manage the large influx of patients during the Omicron surge of the coronavirus disease 2019 (COVID-19), the Hospital Authority (HA) expanded the use of high-flow nasal cannula (HFNC) oxygen therapy devices in the general wards of hospitals in Hong Kong.1 In an interview with Omnihealth Practice, Dr. Tong, Chak-Kwan and Dr. Chan, Yu-Hong John shared their recently published study on the learnings from HFNC use in the general ward setting, describing its benefits in terms of 28-day mortality.1 They also highlighted the prognostic value of the ratio of oxygen saturation (SpO2)/fraction of inspired oxygen (FiO2) (i.e., SF ratio) in settings where a full evaluation using the Respiratory Rate Oxygenation (ROX) index may not be feasible, proposing that the SF ratio can be used to guide counselling and facilitate communication of the care plan with patients or their loved ones.1
HFNC oxygen therapy as respiratory support in general wards during the Omicron surge
During the Omicron surge, Hong Kong was devastated with infection numbers peaking in March 2022 at over a million cases.1 The high transmissibility of this variant, coupled with a low vaccination rate among the elderly population of >60 years old, was a fatal combination, putting them at an elevated risk for respiratory failure, particularly among those with multiple comorbidities.1 During that time, many patients infected with COVID-19 in Hong Kong, who developed acute hypoxemic respiratory failure (AHRF), were managed in the general wards.1
Prior to the pandemic, HFNC oxygen therapy was rarely used in Hong Kong outside of ICUs.1 To combat the Omicron surge, it was implemented in general wards across the Prince Margaret Hospital (PMH) and the North Lantau Hospital (NLTH).1 HFNC oxygen therapy is well-established in patients with acute hypoxemic respiratory failure, offering a decreased work of breathing and improvement in gas exchange for these patients.2 For patients with AHRF, HFNC oxygen therapy was shown to significantly reduce the 90-day mortality rate compared to standard oxygen and other non-invasive ventilation measures.2 Per the World Health Organization (WHO) recommendations, high-flow and non-invasive ventilation may be used in COVID-19 patients with acute respiratory distress syndrome (ARDS).3 Besides reducing mortality rates, other studies involving COVID-19 patients have also shown a reduction in intubation with HFNC use.4
During the Omicron surge, the use of HFNC devices in Hong Kong became widespread.1 It delivers up to 60L/min of humidified gas admixture at 31oC, 34oC, or 37oC.1 Oxygen is delivered with a FiO2 between 0.21 and 1.00 via a low-resistance nasal cannula.1 The default settings of HFNC were 40L/min flow with a FiO2 set at 40% and was given to patients who required >4L/min of oxygen via nasal cannula to maintain an SpO2 of ≥92%.1 Settings were further adjusted according to patients’ SpO2 and respiratory status.1
Effective application of HFNC oxygen therapy: A retrospective cohort study
From 17 March to 30 April 2022, Dr. Tong, Dr. Chan and their team conducted a retrospective cohort study at PMH and NLTH to investigate the benefits of HFNC oxygen therapy in patients with COVID-19 in the general wards.1 Patients who received HFNC oxygen therapy for indications other than AHRF or were subsequently admitted to the ICU were excluded from the study.1 In the end, 49 patients with COVID-19-related respiratory failure treated with HFNC oxygen therapy were included in the final analysis.1
The majority of participants were male (n=34/49) and the mean age among the entire cohort was relatively high at 77.5 years.1 A total of 67.3% (n=33) patients received COVID-19 antiviral medications whilst the rest did not due to delayed presentation.1 These patients had a mean COVID-19 threshold cycle (CT) value of 22.32.1 They had a mean Charlson Comorbidity Index (CCI) of 5.55, a mean clinical frailty score (CFS) of 5.27, and a modified chest X-ray CXR score of 9.16.1 The mean Comorbidity-Age-Lymphocyte count-Lactate dehydrogenase (CALL) score was 11.3 which represented >50% risk of progression of COVID-19 pneumonia.1 Up to 51.0% (n=25) of the cohort was vaccinated, with 10 participants having received 2 doses and 7 participants having completed the full vaccination schedule.1 Notably, almost all patients (n=48) had dexamethasone treatment, and 44.9% (n=22) had positive bacteriological growth in sputum culture.1 Dr. Chan commented that oxygen supplementation is a supportive therapy, and that combating the virus with antivirals and inflammation with glucocorticoids are still the primary goals of treatment in severe COVID-19 diseases.
The primary objective of the study was to assess the 28-day mortality.1 Encouragingly, over half of the patients (53.1%; n=26) survived at 28 days after the initiation of HFNC oxygen therapy, and 46.9% (n=23) survived their index hospital admission.1 It was concluded that the use of HFNC oxygen therapy is feasible in the general ward setting and when intensive care service is in short supply, the use of HFNC oxygen therapy outside the ICU for patients with AHRF should be considered.1 Data on the predictors of non-survivors were also extrapolated and revealed that patients had similar 28-day mortality outcomes regardless of their baseline characteristics such as age, sex, whether they stayed in old age homes, treatments received, and laboratory values (p>0.05 for all).1 The study results showed that “Even patients triaged out from the ICU can be managed in the general wards (with HFNC oxygen therapy) as the survival rate was over 50%.”
The prognostic value of SF ratio in predicting survival
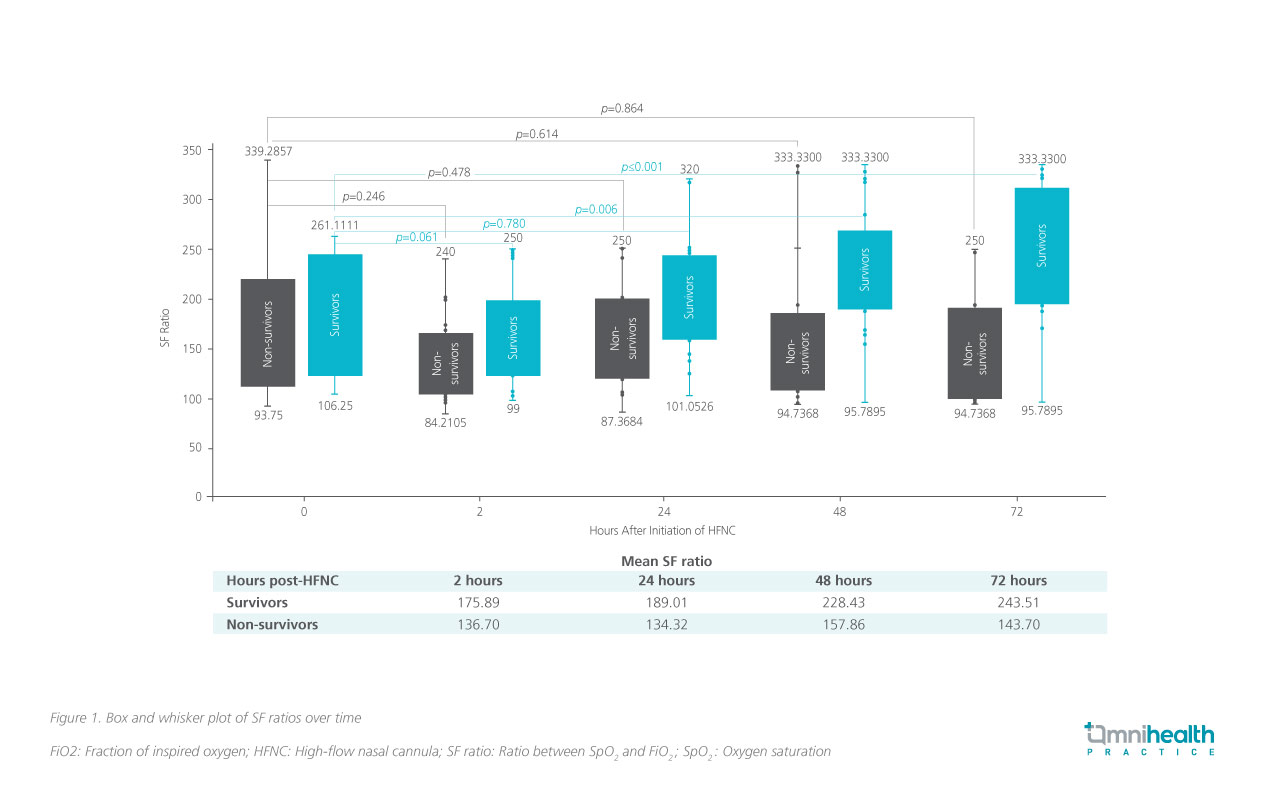
Dr. Tong reflected that in the setting of a pandemic, traditional tools (e.g. the ROX index) may not be feasible to be used as it may be difficult to capture the respiratory rate (RR) and partial pressure of oxygen (PaO2) when the patient is in isolation.1 Studies have also shown that RR is not always captured accurately by hospital personnel.5 In this study, SF ratio presents itself as an invaluable tool to assess patients in a simpler manner.1 It is a practical and specific index in predicting 28-day survival and guides the care plan even in resource-limited settings.1 In the analysis, survivors had a statistically higher SF ratio compared to non-survivors (p<0.05).1 Significant improvements in SF ratio at 48 hours (p=0.006) and 72 hours (p<0.001) compared with baseline were observed in 28-day survivors, indicating a lower probability of mortality (figure 1).1
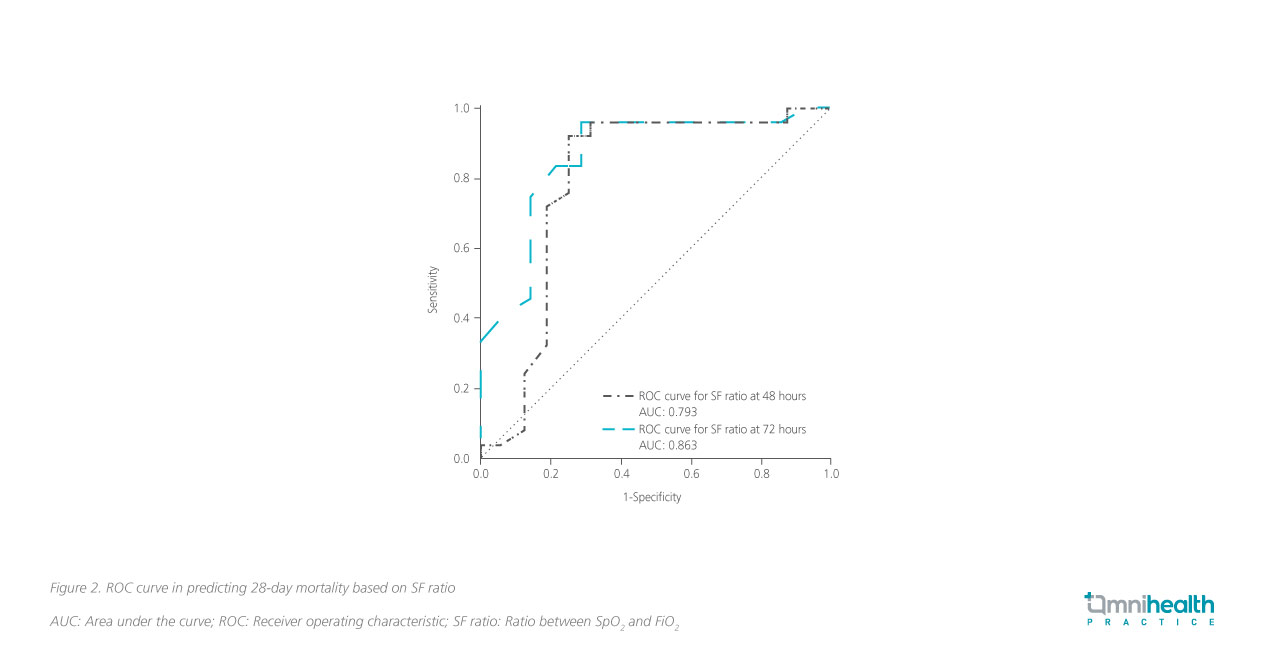
To further elucidate the association between SF ratio and 28-day survival, a receiver operating characteristic (ROC) curve was plotted to identify the threshold value that predicts mortality at 48 and 72 hours (figure 2).1 At 48 hours, an SF ratio cut-off of <160 had 92% sensitivity and 75% specificity in predicting mortality, conferring a 79% accuracy of predicting mortality.1 Similarly, at 72 hours, an SF ratio cut-off of <191 had 83% sensitivity and 79% specificity in predicting mortality, conferring an 86% accuracy in predicting mortality.1 If no improvement in SF ratio is observed at 48 or 72 hours after initiation of HFNC oxygen therapy, continuation of life-sustaining treatment should be reconsidered.1 These clinical indicators may help differentiate patients unlikely to benefit from continuing respiratory support, without jeopardizing those who may still benefit.1
Optimizing care plan and counselling for better patient care
In the study, 73.5% (n=36) patients had a Do-Not-Attempt Cardiopulmonary Resuscitation (DNACPR) order with a mean CFS of 5.42, in which the 28-day mortality was 61.1% (n=22).1 However, 30.6% (n=11) of patients with a DNACPR order survived their index hospital admission with the use of HFNC oxygen therapy.1 This is important because these patients might have been otherwise excluded from using respiratory support.1
To optimize the care plan, Dr. Chan suggested comprehensive counselling should be added to reach a consensus with the patients or their families at the start of HFNC therapy whenever possible.1 It is important to work out a well-defined set of therapeutic goals that include continuation or withdrawal of life-sustaining treatment when reviewing the care plan.6 Dr. Tong seconded that besides being a pragmatic tool, the SF ratio could also help in the process of informing loved ones about the status of the patient.1 Medical futility can be established over a time-limited trial of a few days.1 If no further progress is made, a resolution may then be jointly reached to withdraw the life-sustaining treatment.1 This approach may limit the unnecessarily extended use of life-sustaining therapy in these patients, which is especially important in a resource-limited setting.1
Conclusion
Since the Omicron surge, HFNC oxygen therapy has been widely used in the general ward setting. It offers a feasible option of oxygen supplementation with mortality benefits outside of the ICU, even among patients with a DNACPR order. A comprehensive care plan with well-defined treatment goals may be realized with appropriate counselling informed by the SF ratio, especially under resource-limited settings where a full evaluation with the ROX index may not be feasible.

