CASE REVIEW
Case sharing: Brexpiprazole augmentation in MDD patients with anxiety symptoms provides the trifactor of clinical outcomes, patient compliance and functional recovery
Among patients suffering from major depressive disorder (MDD), more than half of them are encumbered with comorbid anxiety symptoms.1 They represent a more severe form of depression and are often associated with higher morbidity.2 Recovery is more difficult due to a reduced likelihood of response to antidepressant treatment (ADT), requiring treatment augmentation in some cases.2 In an interview with Omnihealth Practice, Dr. Tso, Kwok-Chu discussed the augmentation of treatment using brexpiprazole and its positive effects in reducing symptoms, adverse events (AEs) and non-compliance. To illustrate this, he shared a clinical case in which an MDD patient with anxiety symptoms was administered with brexpiprazole, demonstrating brexpiprazole’s ability to lead to better functional recovery among patients.
Background
MDD with anxiety symptoms signifies a higher impact on patient lives
Major depressive disorder (MDD) is characterized by pervasive low mood, low self-esteem, and loss of interest and enjoyment among other symptoms.3 A study showed that around 56% of MDD patients may also experience anxiety symptoms.1 This represents a more severe form of the disorder and is associated with greater suicidality and impaired functioning.2 These anxiety symptoms also reduce the patients’ compliance with antidepressant treatment (ADT).2 MDD patients with anxiety features generally have a worse prognosis, requiring a longer time to achieve remission.2 As explained by Dr. Tso, the current standard of care (SoC) is to assess compliance first. If remission is not achieved, strategies that may be considered include up-titration, switching medication classes and finally augmentation in that order. This primary treatment goal is to achieve symptomatic remission. Dr. Tso stressed the importance of functional recovery, stating that the resolution of somatic symptoms associated with anxiety is also essential to treatment.
Adopting a comprehensive treatment plan complete with treatment augmentation
As mentioned by Dr. Tso, augmentation is sometimes required in treating MDD patients with anxiety features. He explained that there is no fixed time for the initiation of augmentation, but it may be considered if a subpar response is identified by either the patient or clinician. Earlier augmentation is encouraged since it can lead to positive expectations for patients, which may improve compliance. When synergized with cognitive behavioral therapy (CBT), treatment can aid in establishing a therapeutic alliance with the patient, which is often associated with better outcomes.4 Clinicians should also consider the possibility of residual symptoms and relapse. Dr. Tso explained “My prescribing philosophy is that efficacy is not the only concern. If the patient cannot tolerate the regimen, they will default and miss the golden opportunity for treatment,” once adverse events (AEs) appear, patients tend to become less compliant with treatment, as such, the risks of drug-drug interactions (DDI) and AEs are important considerations.
Case sharing
Dr. Tso shared a case of a 63-year-old male patient. He used to be a Captain in the Fire Services Department but now retired. He has no history of drug or alcohol abuse, nor a family history of mental illness. He was divorced and is in a new relationship. He has an adult daughter from his first marriage.
The patient first presented in 2014 with a pervasive depressed mood. His chief complaints were insomnia, loss of interest and reduced energy level. Somatic symptoms including palpitations, muscle tension, fatigue and abdominal pain were also present. He reported that his then-girlfriend was pressuring him into marriage, which he was hesitant about due to his prior divorce, causing him considerable stress. He developed hypochondriasis, thinking that he had colorectal cancer. Multiple diagnostic checkups including colonoscopies failed to identify any morbidity, prompting a psychiatric referral.
Dr. Tso explained that the treatment goal would be to achieve symptomatic remission. This would help with improving cognitive functions on top of mood stabilization. It would also give him a better ability to resolve his interpersonal issues with his partner, which was the major cause of his anxiety. This helps with the patient’s functional recovery which included the capability for self-care, developing engaging hobbies, establishing healthy relationships, and forming strong social support in his later years.
The patient was initially treated with desvenlafaxine 50mg per day, with a later addition of pregabalin 75mg per day. This regimen was successful, achieving remission in both depressive and anxiety symptoms. However, there was a minor relapse with predominately anxiety symptoms in 2019, after which aripiprazole 2.5mg per day was added. His condition was stable until 2022, when he had anxiety, relapsing depressive symptoms, and somatic symptoms, which were related to his poor compliance. The dose of his medications were then increased to desvenlafaxine 100mg and aripiprazole 5mg per day.
In late 2022, another set of symptoms including episodic attacks of perplexity, self-muttering, disorientation and confusion developed with no recollection in between these attacks. Organic brain disorders, including temporal lobe epilepsy, were suspected on top of the pre-existing mood disorder, but magnetic resonance imaging (MRI) and electroencephalography (EEG) results were inconclusive. Lamotrigine was initiated after no significant improvement with empiric use of sodium valproate.
In February 2023, extrapyramidal side effects (EPSs) such as akathisia and Parkinsonian symptoms were observed. Dr. Tso then switched aripiprazole to brexpiprazole, starting at 0.5mg per day which led to a partial response in April 2023. The dose of his medications were gradually increased to lamotrigine 200mg and brexpiprazole 2mg per day. By May 2023, most symptoms had been resolved. Improvement in terms of emotional, physical, cognitive, social aspects was also observed including a supportive and trustful relationship built between the patient and his partner.
To avoid polypharmacy and risk of possible drug-drug interaction, pregabalin was gradually tapered off. The patient had a slight weight gain from 71.5kg to 73.3kg in 5 months, possibly related to an increased appetite upon symptoms remission. No other AEs were reported. His condition is now stable and was last followed-up in January 2024.
Discussion
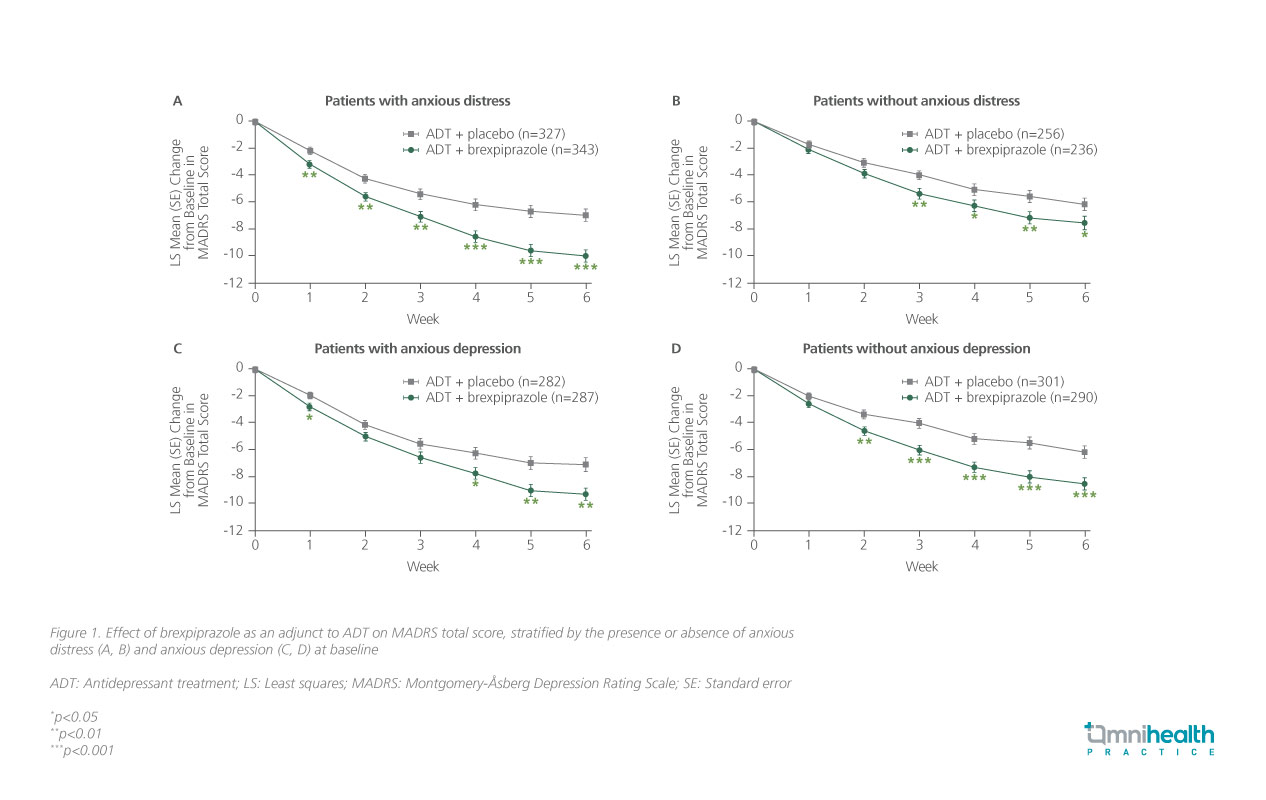
Regarding the success of brexpiprazole treatment in this case, Dr. Tso commented that newer drugs like brexpiprazole can fulfill both efficacy and safety outcomes to facilitate symptomatic remission which encompasses both depressive and anxiety symptoms. Brexpiprazole is a serotonin-dopamine activity modulator (SDAM) with partial agonistic activity at dopamine D2 and serotonin 1A (5-HT1A) receptors and is an antagonist at serotonin 2A (5-HT2A) receptors.5 The drug was initially approved for the treatment in schizophrenia, but its indication has since been expanded in several countries for augmentation of MDD treatment*.5 An ad hoc analysis showed that adjunctive brexpiprazole was effective in reducing depressive symptoms among MDD patients across subgroups stratified by the presence or absence of anxious distress, or anxious depression (figure 1).2
The high affinity of brexpiprazole for 5-HT1A and 5-HT2A receptors reduces the risk of EPS and improves anxiety symptoms.6,7 Similarly, a lower affinity to D2 receptors compared to other antipsychotics lowers the risk of EPS such as akathisia.7 This receptor affinity profile also corresponds to a lower risk of metabolic side effects, weight gain, and anticholinergic effects.8 For the reasons above, brexpiprazole is uniquely advantageous in limiting AEs. Dr. Tso highlighted that patients who are more sensitive to AEs, such as the elderly, patients with organic brain disorder, and patients with anxiety features can benefit from the reduced AEs of brexpiprazole. Such patients will then be more compliant with the treatment. This could provide better symptom control, functional recovery, and ultimately better life engagement once symptomatic remission is achieved.
Conclusion
Brexpiprazole is effective in reducing symptoms among MDD patients with anxiety features.2 Its lower risk of AEs compared to other antipsychotics allows for greater patient compliance.5,6 This leads to better functional recovery in patients in the long term, helping patients re-engage in their lives. Dr. Tso therefore stresses that symptomatic remission should also encompass the resolution of anxiety symptoms. He added that there is a need to establish reasonable expectations of treatment and then proceed with stepwise and continuous effort. Newer drugs like brexpiprazole can fulfill both efficacy and safety requirements.
*Note that in Hong Kong, brexpiprazole is only indicated as an adjunctive therapy to ADT in patients with MDD at a starting dose of 0.5-1mg per day, up to a maximum of 2mg per day. Maximum dose in adjunctive treatment of 3mg has not been approved as of Jan 2024. Treating MDD patients with anxiety features is currently an off-label use in Hong Kong.

