INDUSTRY ESSENTIAL
Navigating anticoagulation strategies for preventing recurrent events in NVAF patients with ischemic stroke despite DOAC
In brief
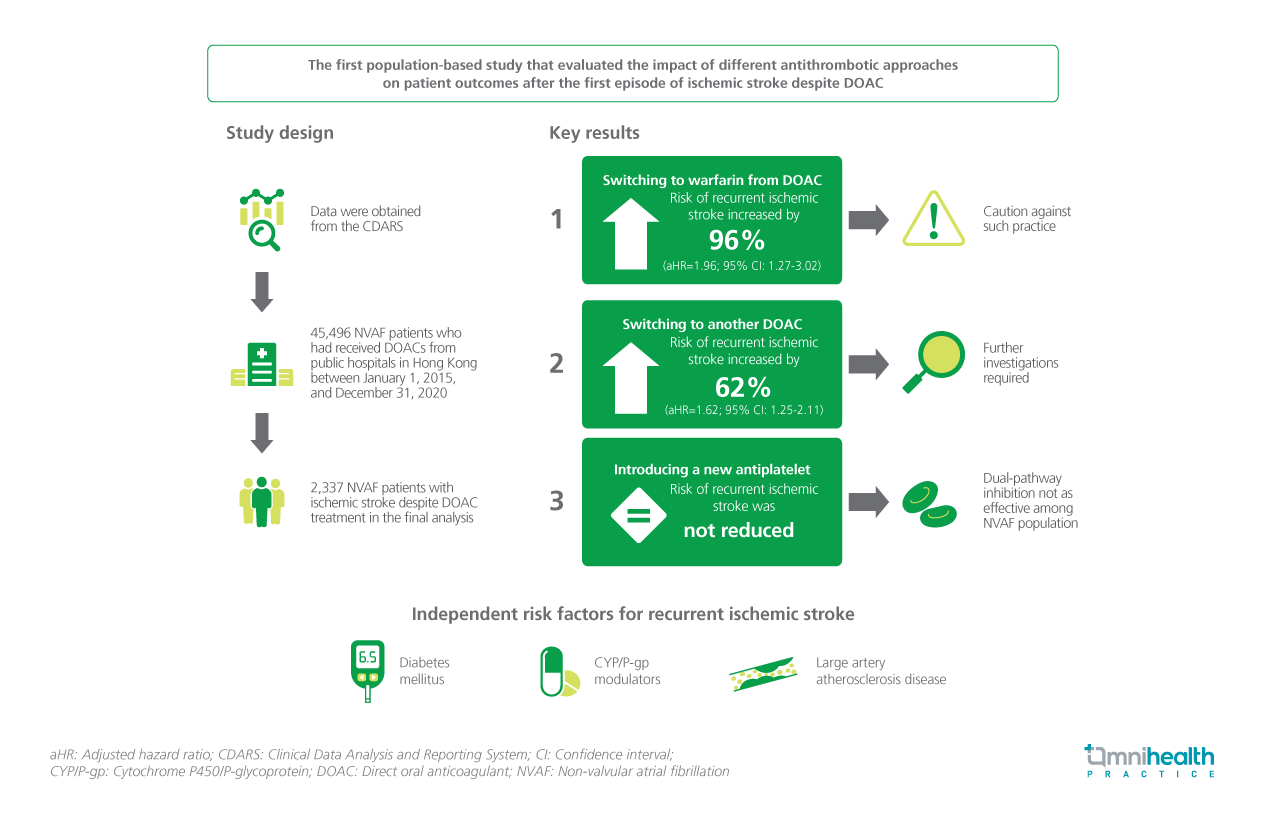
The increasing incidence of ischemic stroke in patients receiving direct oral anticoagulants (DOACs) highlights the heightened risk of subsequent ischemic events.1 Yet, the effectiveness and safety of antithrombotic regimens following this condition remain uncertain.1 In this investigation, patient outcomes were compared between those receiving DOACs with or without an alternative antithrombotic regimen, and the risk factors for recurrent ischemic stroke while on anticoagulation were identified.1 The 6-year study period, spanning January 1, 2015 to December 31, 2020, included 45,946 non-valvular atrial fibrillation (NVAF) patients administered DOACs for stroke prevention.1 Among them, 2,908 patients experienced an ischemic stroke despite the DOAC treatment, and 2,337 NVAF patients were included in the final analysis.1 The findings demonstrated that switching to warfarin (aHR=1.96; 95% CI: 1.27-3.02; p=0.002) or another DOAC (aHR=1.62; 95% CI: 1.25-2.11; p<0.001) was associated with an elevated risk of recurrent ischemic stroke compared with maintaining the same DOAC therapy.1 Furthermore, the addition of an antiplatelet agent did not exhibit a reduced risk of recurrent ischemic stroke.1 The risk factors of recurrent ischemic stroke include diabetes mellitus (DM), concurrent cytochrome P450/P-glycoprotein (CYP/P-gp) modulators, and large artery atherosclerotic disease (LAD).1
Background
In spite of the demonstrated efficacy of DOACs in preventing ischemic stroke in NVAF patients, approximately 30% of NVAF patients who developed stroke were on oral anticoagulant prior to stroke onset.1 As a result of the surging prescription of DOACs, a concomitant increase in the incidence of ischemic stroke despite DOAC was noticed.1 Given that those who have previously experienced ischemic stroke exhibit a greater likelihood of recurrent events, secondary prevention is critical for mitigating the risk.1 Currently, clinicians possess the discretion to either maintain patients’ current DOAC therapy, transition to an alternative DOAC or warfarin, or introduce an antiplatelet agent as an adjunct therapy to supplement the existing treatment regimen.1 However, the effects of these different antithrombotic approaches on patient outcomes are still not clearly comprehended.1
Methodology
This study was a population-based analysis aimed at comparing the clinical outcomes of NVAF patients who experienced an ischemic stroke despite DOAC treatment.1 The analysis focused on patients who either continued with the original DOAC therapy, switched to another DOAC or warfarin, or had an additional antiplatelet agent prescribed.1 The goal was to understand the relationship between these alternative anticoagulation strategies and patient outcomes, specifically the reduction in the risk of recurrent ischemic stroke.1 By gaining insight into this association, it is hoped that this study could inspire future treatment decisions and enhance patient outcomes.1
In this investigation, clinical data were obtained from the Clinical Data Analysis and Reporting System (CDARS), a comprehensive database encompassing clinical information of over 90% of Hong Kong's 7.5 million residents.1 A total of 45,496 NVAF patients who had received DOACs, including apixaban, dabigatran, edoxaban, or rivaroxaban, were identified from the public hospitals in Hong Kong between January 1, 2015, and December 31, 2020, and the majority of these patients (n=42,588) did not experience an ischemic stroke.1 The exclusion criteria included patients with active malignancy, mitral stenosis, left ventricular thrombus, valvular replacement, left atrial appendage occlusion (LAAO), atrial septal defect (ASD), polycythemia rubra vera (PRV), essential thrombocytosis, and thrombophilia.1 Patients who discontinued anticoagulation after the stroke event or had inappropriate DOAC dosage relative to body weight, renal function, and age at stroke onset were also excluded.1 The final analysis encompassed 2,337 NVAF patients with ischemic stroke despite the DOAC treatment, distributed among the “DOAC unchanged” (n=1,652; 70.7%), the “switched DOAC” (n=477; 20.4%), and the “switched to warfarin” (n=122; 5.2%) groups.1 Among 1,652 patients in the “DOAC unchanged” group, 249 patients (15.1%) were started on antiplatelet agents within 8 weeks of the first ischemic stroke despite DOAC.1
The primary outcome assessed was recurrent ischemic stroke following the initial episode of ischemic stroke despite the DOAC therapy.1 The secondary outcomes included intracranial hemorrhage (ICH), acute coronary syndrome (ACS), and all-cause mortality (ACM).1
Results
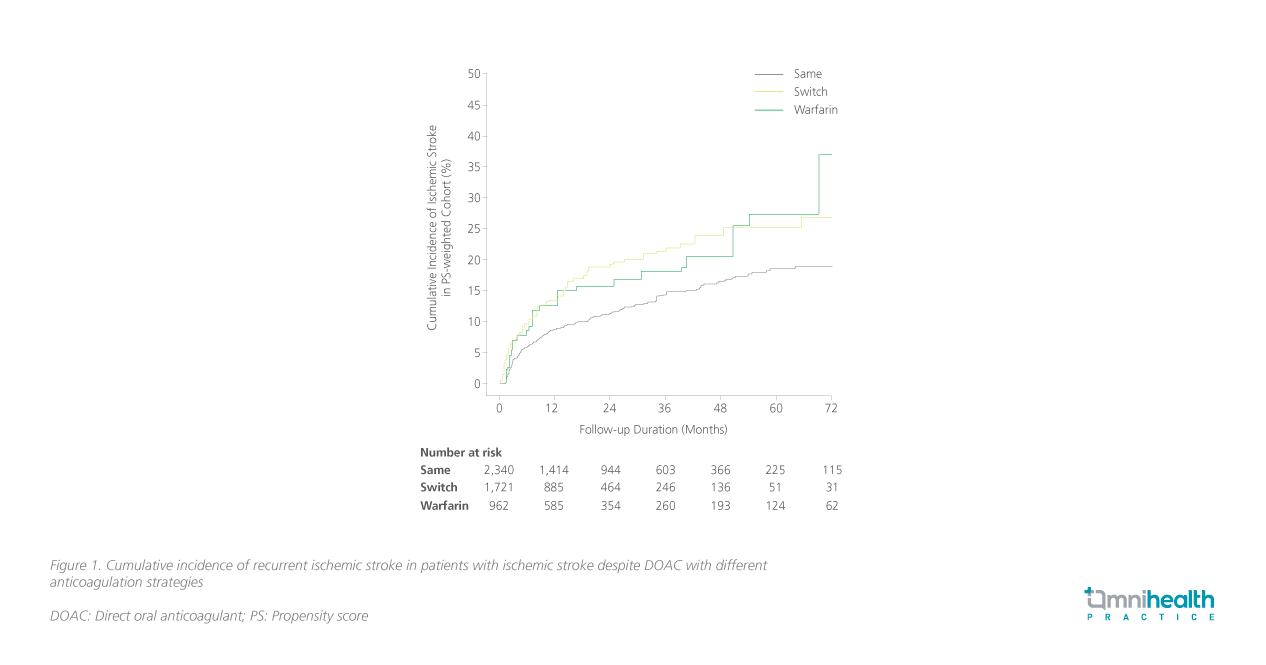
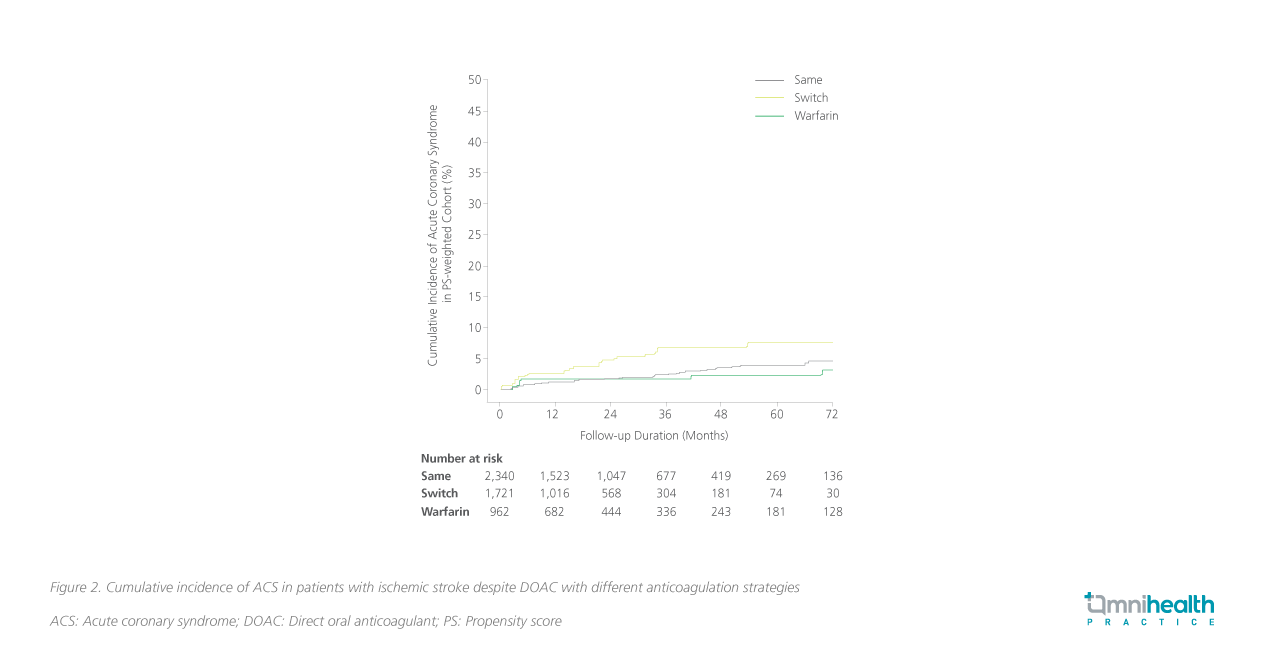
Upon comparison with the “DOAC unchanged” group, a transition from the initial DOAC treatment to warfarin following an ischemic stroke event was associated with a 96% augmented risk of recurrent ischemic stroke (aHR=1.96; 95% CI: 1.27-3.03; p=0.002) (figure 1).1 Similarly, switching the original DOAC with an alternative DOAC manifested a 62% elevation in the risk of ischemic stroke recurrence (aHR=1.62; 95% CI: 1.25-2.11; p<0.001).1 Furthermore, the “switched DOAC” group exhibited a more than two-fold increase in the risk of ACS in comparison to the “DOAC unchanged” cohort (aHR=2.18; 95% CI: 1.29-6.67; p=0.003) (figure 2).1 However, the analysis revealed no discernible escalation in the risk of ICH and ACM among the different anticoagulation strategies (table 1).1
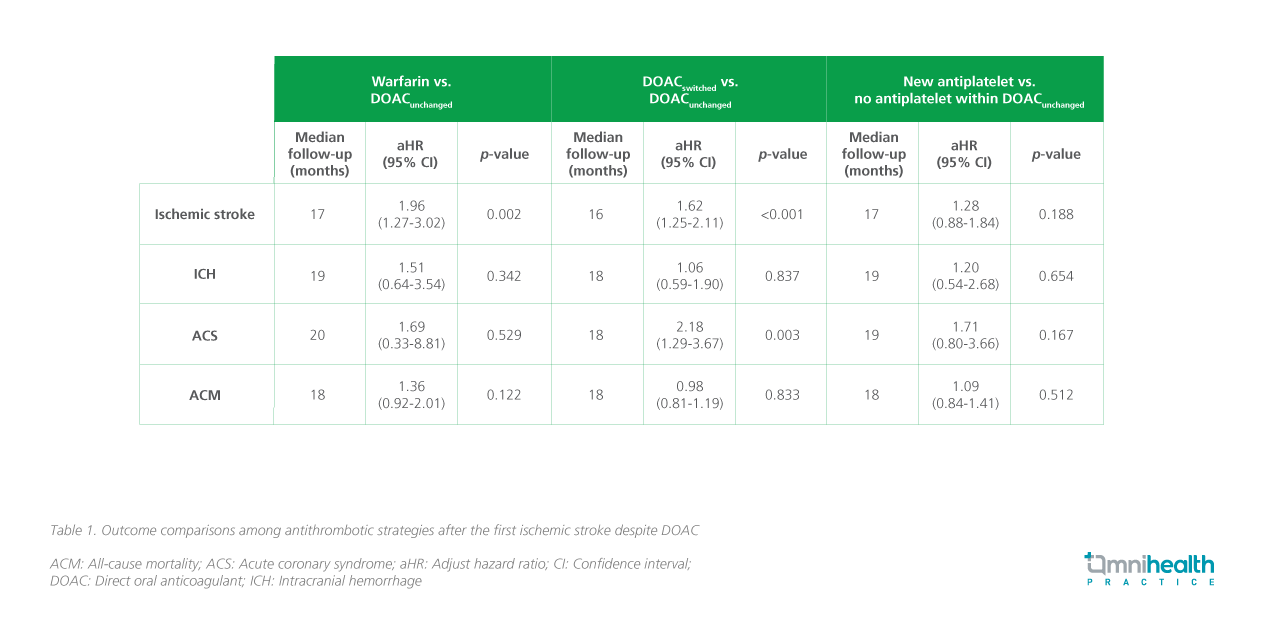
Within the “DOAC unchanged” group (n=1,652), a new antiplatelet was introduced in 249 patients (15.1%) within 8 weeks after the first ischemic stroke despite DOAC.1 The findings indicated that the addition of an antiplatelet agent did not significantly decrease the risk of recurrent ischemic stroke (aHR=1.28; 95% CI: 0.88- 1.84; p=0.188), ICH (aHR=1.20; 95% CI: 0.54-2.68; p=0.654), ACS (aHR=1.71; 95% CI: 0.80-3.66; p=0.167), or ACM (aHR=1.09; 95% CI: 0.84-1.41; p=0.512) (table 1).1
The study also identified several associated risk factors of recurrent ischemic stroke, including advanced age (aHR=1.02; 95% CI: 1.00-1.03; p=0.029), the history of DM (aHR=1.49; 95% CI: 0.73-1.20; p=0.002), the use of CYP/P-gp modulators (aHR=1.39; 95% CI: 1.05-1.84; p=0.021), and LAD (aHR=2.84; 95% CI: 1.16-6.91; p=0.021).1
Discussion
This is the first population-based study that evaluated the impact of different antithrombotic approaches on patient outcomes after the first episode of ischemic stroke despite DOAC.1 The key findings of this study were: 1) Switching to warfarin or another DOAC was associated with an increased risk of recurrent ischemic stroke; 2) Introduction of a new antiplatelet agent to the original DOAC therapy would not reduce the risk of recurrent ischemic stroke; and 3) Advanced age, DM, the concurrent use of CYP/P-gp modulators and LAD were predictors of recurrent ischemic stroke.1
Due to the demonstrated higher risk of recurrent ischemic stroke with warfarin, this study cautioned against the practice of switching to warfarin after the first ischemic stroke event, unless the benefits outweigh the risks.1 Warfarin may still be indicated when patients have severe renal insufficiency, antiphospholipid syndrome, or valvular atrial fibrillation.1 Interestingly, switching to another DOAC also showed an increased risk of recurrent ischemic stroke and ACS, with an unclear underlying mechanism.1 Further studies are needed to confirm the association.1
Furthermore, although some studies showed that the combination of an antiplatelet and a DOAC could confer cardiovascular (CV) protection to patients with atherosclerotic diseases, this study did not find such a clinical benefit of additional antiplatelet therapy in NVAF patients with ischemic stroke despite DOAC.1 The result suggested that this dual-pathway inhibition strategy might be not as effective among the NVAF population.1
Notably, although DM was shown to be a risk factor for recurrent ischemic stroke, the mean glycated hemoglobin A1c (HbA1c) was not significantly different among patients with or without recurrent ischemic stroke.1 Further studies are required to determine whether a more stringent long-term glycemic control would be conducive to reducing the risk of recurrent events among these patients.1
Yet, there are several limitations to this study.1 Firstly, as a retrospective study, unmeasured confounders might exist.1 Factors such as the DOAC level, compliance, and competing stroke etiologies could have biased comparisons.1 Secondly, the sample size of the warfarin group was comparatively small.1 Therefore, although the warfarin group exhibited a numerically higher incidence of ICH when compared with the “DOAC unchanged” group, the study was not powered to ascertain statistical significance.1 Thirdly, LAAO represents an alternative intervention for patients with ischemic stroke despite DOAC. However, the outcomes of these patients were not assessed in the current investigation.1 Lastly, it is important to note that 98% of the study population was ethnic Chinese, potentially limiting the applicability of the findings to other populations.1
Conclusion
In conclusion, this study highlighted an elevated risk of recurrent ischemic stroke in NVAF patients who switched to warfarin following an ischemic stroke despite the DOAC treatment, emphasizing caution regarding this approach.1 Additionally, the investigation revealed no significant clinical benefits associated with adjunctive antiplatelet therapy in this patient population.1 While DM, the use of CYP/P-gp modulators, and LAD were identified as predictors of recurrent ischemic stroke, further research is required to determine whether stringent glycemic control, DOAC level monitoring, and routine screening for carotid and intracranial atherosclerosis may contribute to a reduction in ischemic stroke recurrence among these patients.1
Graphical abstract