MEETING HIGHLIGHT
A paradigm shift in acute hyperkalemia management with sodium zirconium cyclosilicate in the ED setting
Given its high rates of complications and mortality, hyperkalemia is traditionally difficult to manage, particularly in the emergency department (ED) setting. In a webinar on the best practice of hyperkalemia in emergency and intensive care, Professor. W. Frank Peacock discussed the prevalence and severity of hyperkalemia in the emergency medical setting, demonstrating the significance of sodium zirconium cyclosilicate (SZC) as a potassium binder to manage hyperkalemic patients safely and effectively in the ED. Rapid reduction in K+ (potassium ions) has not only reduced the mortality risk but also enabled emergency physicians to spend less time managing hyperkalemic patients, thus helping reduce the clinical burden of the ED.
The physiology of hyperkalemia in relation to the potassium level
Potassium is involved in many physiological processes, including the contraction of skeletal and cardiac muscles, allowing them to function properly.1 Approximately 98% of potassium in the body is intracellular, while the remaining 2% is located in the extracellular space.2 The delicate balance between intracellular and extracellular potassium is thus vital for proper body function.2 Besides, there is a dose-dependent relationship between hyperkalemia and fatal arrhythmias, i.e., the higher the potassium level, the greater the mortality risk.3 In general, a normal potassium level is between 3.5mEq/L and 5mEq/L, while the in-hospital mortality rate of hyperkalemia is about 13.6% when potassium reaches a level of 6mEq/L.4 In the long-term follow-up (median=17.3 months), the all-cause mortality rate is up to 42.5% after an episode of severe hyperkalemia.5 Therefore, hyperkalemia is a life-threatening condition that warrants emergent treatment to prevent cardiac arrhythmias and subsequent complications.5
The common associated conditions with hyperkalemia
Chronic kidney disease (CKD) is the most common associated condition in hyperkalemic patients, as the pathophysiology of CKD will lead to a decrease in potassium excretion.1,3 The use of medications in treating CKD alters kidney physiology in a way that will eventually increase serum potassium levels.1 This includes angiotensin-converting enzyme (ACE) inhibitors, angiotensin II receptor blockers (ARBs), spironolactone, and non-steroidal anti-inflammatory drugs (NSAIDs).1 These medications alter the kidney’s ability of potassium excretion, thereby increasing the serum potassium levels.1 Other common conditions relating to hyperkalemia include cardiovascular disease, diabetes and liver disease.5
Defects of the traditional hyperkalemia treatment options
Typically, hyperkalemia is treated in the ED with medications, including intravenous calcium, glucose, insulin, and beta-agonists such as inhaled salbutamol, with the aim of reducing the potassium levels in the blood in short term.3 Insulin-glucose can temporarily lower the serum potassium levels by causing potassium to move from the extracellular environment into the cells.3 Although this treatment option is effective, it can only last for 4-6 hours and does not eliminate K+. Rebound hyperkalemia is frequent, and there is also a significant risk of hypoglycemia.3
With regard to treatment with beta-agonists, salbutamol causes a shift of potassium into the intracellular space, which is also a short-term solution for hyperkalemia management. But like insulin/glucose, rebound hyperkalemia will occur without further interventions.3 Among the treatment options, dialysis is an effective way to manage hyperkalemia.3However, it is often difficult to perform quickly, and is costly in the ED.3
Sodium polystyrene sulfonate (SPS) is another option. This potassium-binding hyperkalemia treatment was first introduced in 1958.6 SPS is a non-selective, cation-exchange resin binding potassium in the large intestine with an onset of action within 2-24 hours.7,8 SPS is associated with gastrointestinal (GI) adverse events (AEs), including diarrhea, nausea and vomiting, making SPS hard to tolerate.7 Besides, a serious AE related to SPS is colonic necrosis, which is a life-threatening condition, leading SPS to receive a black box warning in 2009.7
The introduction and advantages of sodium zirconium cyclosilicate
SZC is a microporous zirconium silicate compound designed as a selective potassium trap.9 Given the structure of SZC, there is no systemic absorption or metabolism of this medication.10 Regarding its efficacy, a single dose of 10g of SZC reduces the potassium levels by 0.4mEq/L in the first hour,0.6mEq/L in the second hour, then by 0.7mEq/L at 4 hours in severe hyperkalemia patients (K>6).11 Normalization of hyperkalemia in ED patients is associated with a 50% mortality reduction.12 The mortality rate of patients with a potassium level of 6mEq/L is about 13.5%, while those with a potassium level of 5.3mEq/L is 4%.11 By estimation, when the potassium level can be lowered by 0.7mEq/L, the absolute and relative mortalities will decrease by 9.5% and 54%, respectively.11
The superiority of sodium zirconium cyclosilicate over sodium polystyrene sulfonate
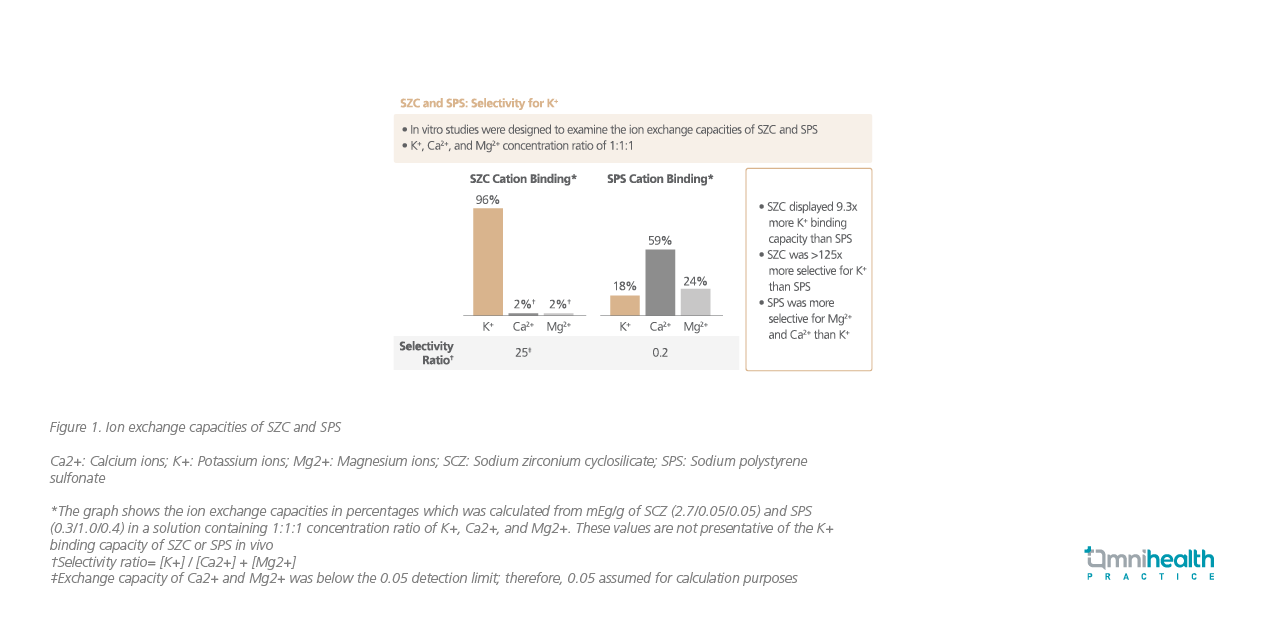
SZC is not absorbed and thus selectively traps potassium in the GI tract.13 While it does not bind to substances like calcium as other binders do, the potassium binding capacity of SZC is 9.3 times that of SPS.13 Furthermore, SZC is 125 times more selective for potassium than SPS (figure 1).13 Lastly, since SZC is insoluble, it does not expand when it comes to contact with water in the GI tract and therefore does not cause profound diarrhea which is frequently associated with SPS.13
The HARMONIZE trial demonstrates rapid potassium reduction by sodium zirconium cyclosilicate
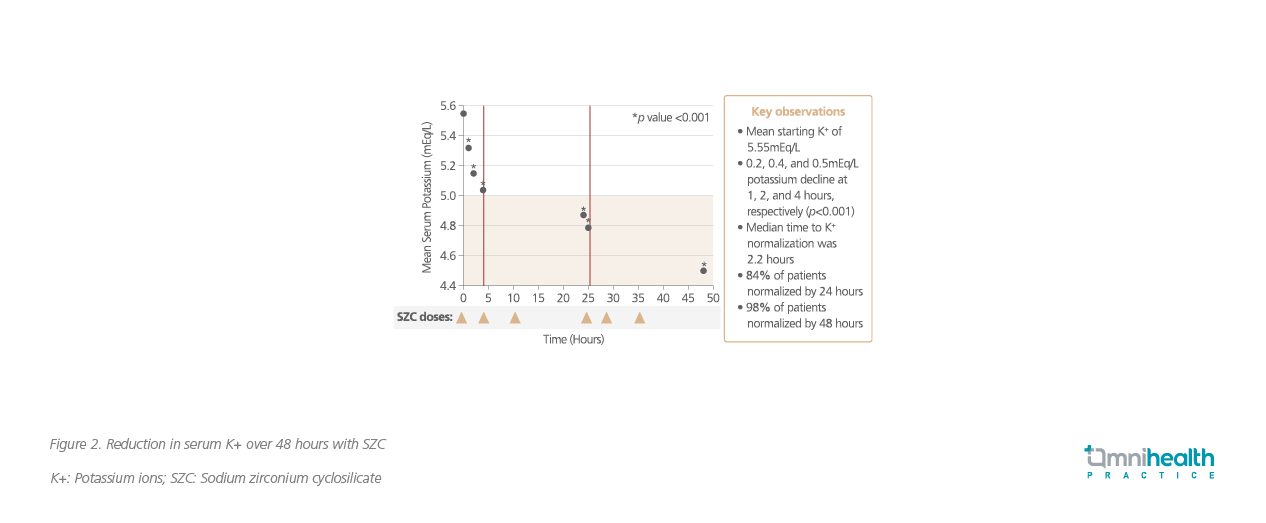
In the HARMONIZE trial, hyperkalemic patients were prescribed SZCdaily for a month to assess its efficacy and safety.9 It was reported that the use of SZC provided rapid and sustained reduction in the potassium levels in hyperkalemic patients (figure 2).9 Patients were given 10g of SZC 3 times daily in the first 48 hours of the study.9This led to a rapid reduction in the potassium levels, often after the first dose.9 The median time to the potassium level normalization was 2.2 hours.9 Overall, 84% of patients achieved normokalemia by 24 hours of SZC dosing and 98% were normokalemic within 48 hours of the SZC treatment.9 In this trial, SZC was clearly superior to placebo in reducing hyperkalemia and it was generally well-tolerated.9 A lower rate of GI AEs was observed in 5g and 10g SZCwhen compared with placebo in the 28-day maintenance phase.9
The ENERGIZE trial shows good tolerability of sodium zirconium cyclosilicate
In the ENERGIZE trial, blinded SZC + insulin/glucose therapy was compared with blinded placebo + insulin/glucose therapy. The investigators reported that where SZC demonstrated a good tolerability, AE profile in the first 24 hours was similar between the treatment groups.14 Furthermore, the use of SZC in the ED was not found to be associated with an increased risk of hypokalemia.14 Important ED work flow considerations were that patients on SZC were less likely to require rescue therapy (15.6% SZC vs. 30.6% placebo from 0 to 4 hours) or dialysis (33.3% SZC vs. 48.6% placebo overall).14 Finally, in hyperkalemic patients, there was a higher discharge rate among those given SZC than the standard care (39.4% SZC vs. 32.4% placebo).14
The use of sodium zirconium cyclosilicate in the ED
In the ED, SZC is administered to help reduce the potassium levels sustainably, while dialysis is arranged for patients in need (figure 3).11,14,15 The current standard of care (SoC) of using salbutamol, insulin and glucose only contributes to the transient improvement in the potassium levels. Once this levels begin to rebound, it requires extra work and time for the ED physicians and nurses to manage hyperkalemia.3,16 In particular, the use of insulin will increase the risk of hypoglycemia, especially when the insulin treatment hasto be repeated. Thus, patients who receive insulin require careful periodic monitoring to avoid hypoglycemia. In case of occurrence of hypoglycemia,the insulin treatment can lead to seizures and death, leading to dangerous complications of hyperkalemia if not quickly corrected.3,16
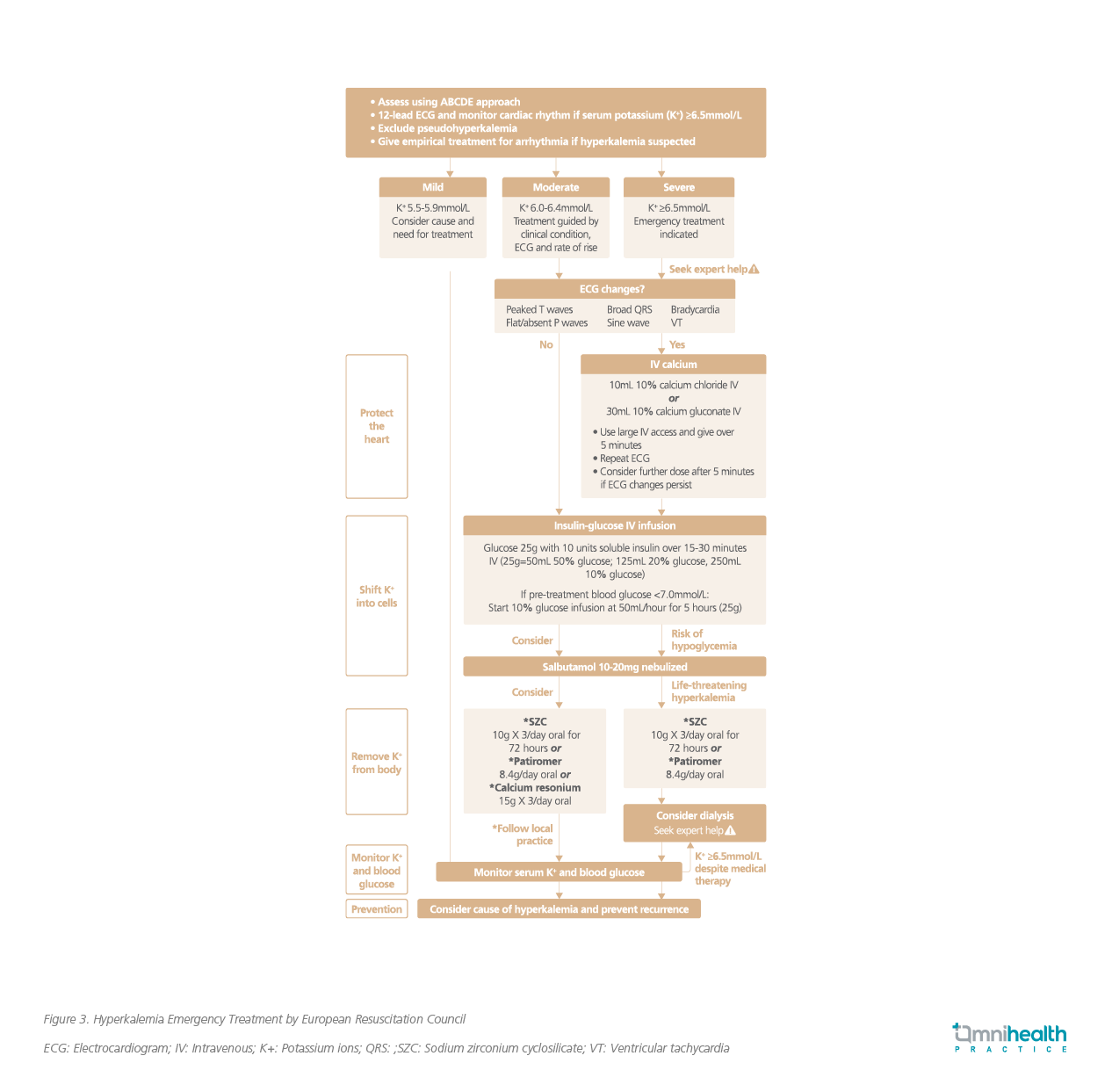
Compared with previous potassium binders, SZC likely lowers the potassium levels faster and has a longer duration of efficacy.13,14 One hour after administration, the drug begins to exert its effects and a significant reduction of the potassium levels are observed after 4 hours.14 The National Institute for Health and Care Excellence (NICE) guidelines recommend SZC as an option for treating acute life-threatening hyperkalemia in the ED, if it is used in conjunction with the standard care for the medical condition.17 These guidelines state that “SZC could be a useful addition to emergency care”.17 Considering that this medication helps reduce the rate of admission in patients with hyperkalemia and allow them to be discharged home, the guidelines deem SZC as cost-effective and a wise use of healthcare resources.17
Examples showcase the efficacy of sodium zirconium cyclosilicate
Prof. Peacock then shared 2 examples of clinical cases that demonstrated the efficacy of SZC (figure 4). Both examples started with the same potassium levels, with the first patient receiving SoC, while the second patient received SoC + SZC. The first patient (SoC treatment) required more time and follow-up care from the ED physicians. This increased the workload and resulted in the ED physicians only being able to take care of 13 patients during their shift, and consequently the patient had a hypoglycemic seizure.
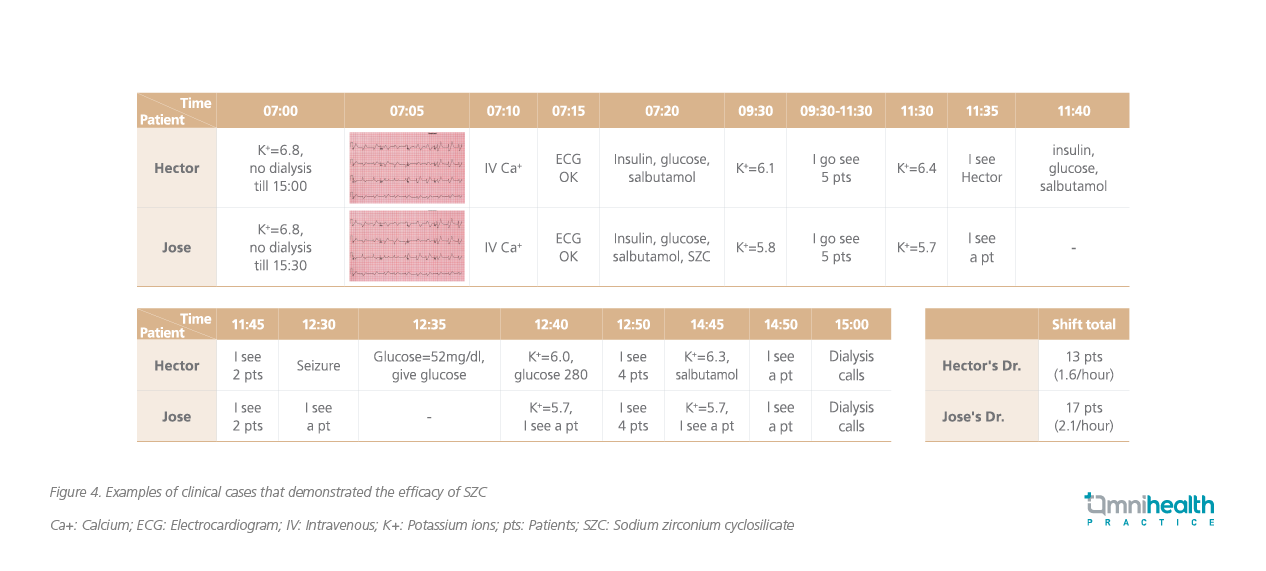
The second example is the same hyperkalemic patient who received the SoC + SZC. This time, far fewer treatments were required by the ED physicians, and the patient had an uncomplicated course in the ED prior to dialysis. In this second patient, the K+ level was well controlled by SZC. The ED physicians were able to handle 17 patients in their shift, illustrating that the adoption of SZC in treating hyperkalemia can optimize the use of healthcare resources and physician time. Patients can be managed well and safely while awaiting the dialysis services.
Conclusion
Traditionally, hyperkalemia is a life-threatening and difficult medical condition to be managed in the ED. The traditional hyperkalemia treatment options are often temporary and may associated with several AEs, e.g., diarrhea, hypoglycemia and even colonic necrosis. The introduction of SZC has led to a paradigm shift in the treatment of acute life-threatening hyperkalemia. The drug is a safe, effective in both acute and chronic hyperkalemia treatment. Adoption of SZC in the ED will help optimize the use of healthcare resources and physician time. This medication is also well tolerated with a demonstrated safety profile, making it more appealing and practical than old-generation potassium binders. In the acute management of hyperkalemia, SZC is becoming part of the SoC.

