CONFERENCE UPDATE: AHA 2021
Guidelines for the evaluation and diagnosis of chest pain
Chest pain is one of the most common reasons for patients to present to the emergency department, and the acute coronary syndrome (ACS) needs to be distinguished from a variety of other cardiac and non-cardiac diseases that may cause chest pain.1 Which is the dominant and most frequent symptom for both men and women ultimately diagnosed with ACS. Women may be more likely to present with accompanying symptoms such as nausea and shortness of breath. The first-ever clinical guideline from the American College of Cardiology (ACC) and American Heart Association (AHA) for the evaluation and diagnosis of patients with chest pain who are sent to the emergency department, provides recommendations and algorithms to conduct initial assessment of chest pain for triaging patients effectively on the basis of the likelihood that the symptoms may be attributable to myocardial infarction (MI).1
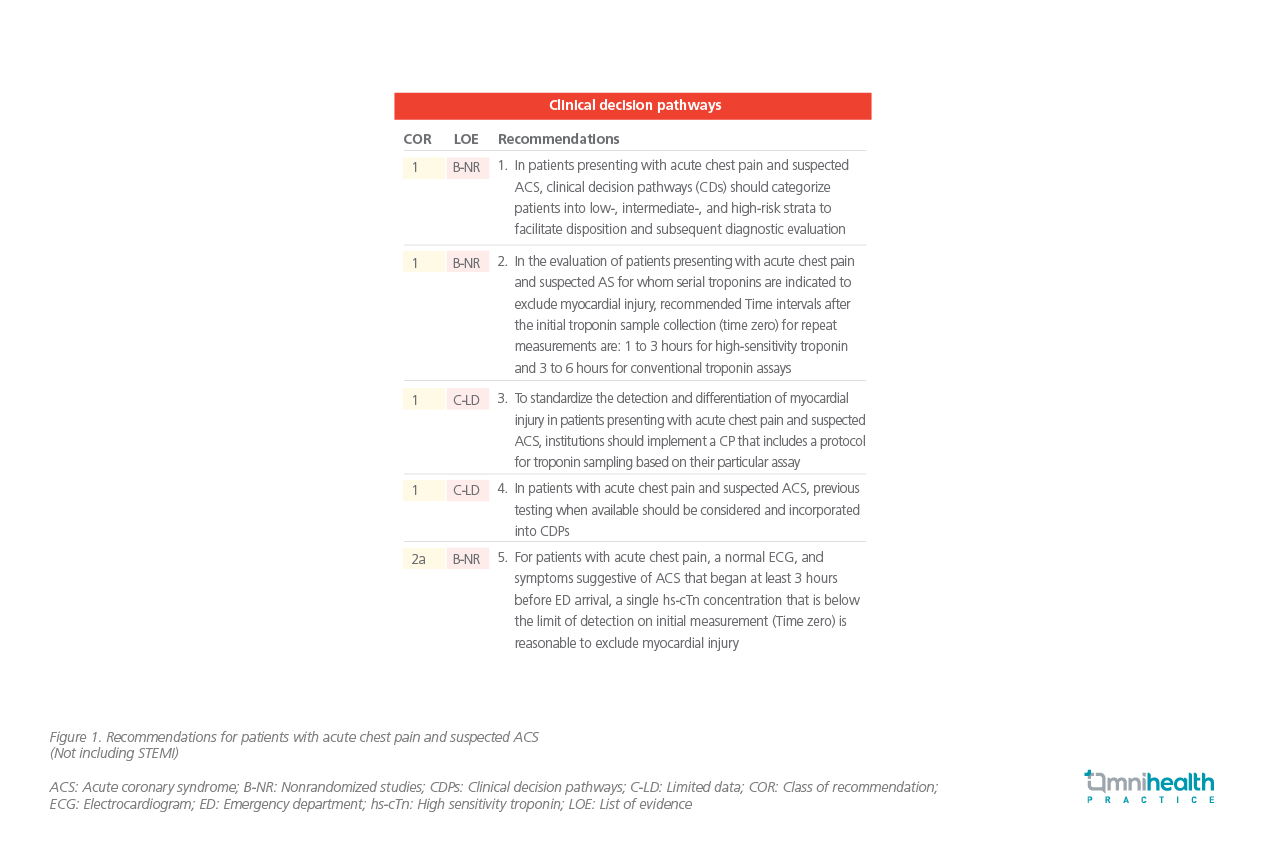
As embarked by Professor Phillip D Levy, professor of the emergency medicine and assistant vice president for research at Wayne State University in Detroit, the new guidelines recommend that clinicians should employ standardized risk assessments, clinical decision pathways (CDPs), as well as tools to assess the chest pain and quickly identify the source, like MI or other heart complications.1 In patients presenting with acute chest pain and suspected ACS, CDPs should categorize patients into low-, intermediate-, and high-risk strata to facilitate disposition and subsequent diagnostic evaluation.1 Importantly, the use of high sensitivity cardiac troponins (cTn) was also recommended as the preferred standard for establishing a biomarker diagnosis of acute MI, for more accurate detection of myocardial injury, and estimate a patient’s probability of ACS or risk of 30-day major adverse cardiovascular events (MACE).1,2 He further added that the patients presenting with symptoms of acute chest pain or ACS initially evaluated in office setting should be transferred to emergency department as soon as possible for cTn testing or other diagnostic testing.2 The recommended time intervals after the initial troponin sample collection for repeat measurements are 1 to 3 hours for high-sensitivity troponin and 3 to 6 hours for conventional troponin assays.
Prof. Levy also emphasized, CDPs based on cTn results for chest pain in the emergency department and outpatient settings should be used routinely, to standardize the decision making for low, intermediate, and high-risk stratification patient groups.2 To rapidly detect and exclude acute myocardial injury, incorporating time-dependent serial cTn sampling is important. To standardize the approach to patient care and ensure consistency in decision-making, CDPs should be implemented at the institutional and multidisciplinary level. There are multiple CDPs to choose, for example, the History, Electrocardiogram (ECG), Age, Risk factors, and Troponin (HEART), the Emergency Department Assessment of Chest Pain Score (EDACS) pathway, modified accelerated diagnostic protocol to assess patients with chest pain symptoms using troponin as the only biomarker (m-ADAPT), no objective testing rule (NOTR), and high-sensitivity troponin (2020 ESC/hs-cTn) pathways, but all generally involve single or serial cTn measurement (Figure 1).2
Over the past decade, the quality of evidence supporting clinical indications for non-invasive testing has grown dramatically. Selective use of testing, optimization of lower cost evaluations, reducing layered testing, and deferring or eliminating testing when the diagnostic yield is low, should be the core focus. For intermediate-risk patients with acute chest pain who have known CAD and present with new onset or worsening symptoms, guideline-directed medical therapy should be optimized before additional cardiac testing is performed. “CDPs as well as the use of structured risk assessment using evidence-based protocols for patients presenting with acute or stable chest pain should be used in the emergency department and outpatient settings.” Prof. Levy highlighted.

