EXPERT INSIGHT
Improving multiple sclerosis management in Hong Kong through integrative Western-Chinese medicine approach
Multiple sclerosis (MS) is among the most common central nervous system (CNS) inflammatory demyelinating diseases with an estimated global prevalence of 1 in 3,000 people in 2020.1 Although MS is regarded as relatively uncommon in the Asia Pacific Region and even rarer in Hong Kong with a local prevalence of 0.77 per 100,000 people in 1999, a recent study revealed that the local MS prevalence was 6.9 per 100,000 people in 2020, which was higher than mainland China and Taiwan.2,3 In an interview with Omnihealth Practice, Dr. Alexander Lau explained the rising trend of MS in Hong Kong over the past decade. To better manage MS, Dr. Lau also discussed the opportunity of having an integrative platform that combines both Western and Chinese medicine as a comprehensive approach for long-term MS treatment.
Improved diagnostic tools lead to rising MS prevalence
Compared with other chronic illnesses, MS is a particularly devastating neurological disease as it is most prevalent in young adults during their most productive years with symptoms onset typically before 30-years-old.2 In the past, MS diagnosis could be delayed to an upward of 5 to 10 years from symptom onset. With recent advances in diagnostic tools, including the revised McDonald criteria for the diagnosis of MS, improved magnetic resonance imaging techniques, and, utilization of body fluid biomarkers, the accuracy of MS diagnosis has been substantially improved and the diagnostic delay was reduced to less than 1 year. Besides, education campaigns organized by both private and public organizations have raised the patients’ awareness, propelling them to seek neurologists and specialists’ consultation for early detection of signs and symptoms of MS. Together, clinicians can now make more accurate MS diagnosis while distinguishing it from other diseases that can clinically or radiologically mimic MS. All the above may have attributed to a marked increase in the local MS prevalence from 2008 to 2015.3,4
The paradox of rapid inflammatory control versus neurodegeneration from chronic inflammation
In view of an increase in local MS prevalence, a variety of disease-modifying therapies are made available in Hong Kong to manage these newly diagnosed MS patients. However, most pharmacotherapies are targeted towards the suppression of inflammation, but cannot reverse the neurodegeneration caused by chronic inflammation within the brain. Indeed, recovery of MS patients from early inflammation is often achievable due to brain functional reserve from neuroplasticity.5 However, without adequate treatment, MS patients who initially experience relapse-remitting MS (RRMS) suffers from more chronic inflammation that leads to CNS scarring, often complicated with brain function deterioration and early onset neurodegeneration. Moreover, RRMS patients who advanced to secondary progressive MS (SPMS) can have compartmentalized inflammation within the CNS, where many current pharmacological options cannot effectively exert the therapeutic benefits. As neurological disabilities can be slowly accumulated throughout the disease course of MS, the treatment goal should not be limited to immediate inflammatory control, but rather to achieve no evidence of disease activity (NEDA) or minimal evidence of disease activity (MEDA) early to prevent disease progression or further relapse. As clinical trials of new drugs are underway, which show the potentials of penetrating the blood-brain barrier and modulating the immune system within the brain, it is highly likely that MS can be controlled to an almost cured state with the appropriate adoption of diagnostic tools and pharmacotherapies to prevent the accumulation of neurological disabilities.6
Unmet local needs to support MS patients with neurological disabilities
Whereas appropriate pharmacotherapies can help prevent the progression or relapse of MS, the existing neurological disabilities remain an irreversible aspect of MS treatment. Notably, many patients will develop fatigue and cognitive symptoms due to MS chronicity, which cannot be treated by pharmacotherapies alone. In Western countries, especially Scandinavian countries, MS is a common illness that patients and neurologists often engage in open discussions, along with supportive and caring resources to address those neurological disabilities.1 In the short-term, physiotherapy and occupational therapies, especially after recent relapse, can help hasten recovery and neurological functions so as to restore daily activities and working capacity.7 In the longterm, regular physical exercise may help improve neurological functions and protect against depression associated with MS.7 As MS is still a relatively rare disease in Hong Kong despite the recent rising trend, many supportive measures are not readily available and yet to be sufficient.2,3 From clinical experience, approximately 70% of local chronic disease patients will seek Chinese herbal medicine (CHM) instead to improve their quality-of-life, prompting the need to evaluate the benefits and safety of adopting an integrative Western and Chinese medicine approach in the treatment of MS.
A novel platform to provide integrative Western and Chinese pharmacological support
From the neurologist’s perspective, MS is a well-defined disease that its treatment is based on an individualized approach dependent on the observed symptoms and the patient’s response. While to the Chinese medicine practitioners (CMPs), MS is not a well-characterized diagnosis in Chinese Medicine, and its treatment is based on a holistic approach to restore health. In a practical setting, CHM is a non-target specific treatment approach and cannot replace the Western medicine for disease control such as rapid immunomodulation. However, fatigue and cognitive symptoms associated with MS remain difficult to treat with pharmacotherapies, and that CHM may help reduce the extent of side effects experienced over the chronic management of MS. When taking the local clinical setting into consideration, an ideal approach would therefore be a complementary strategy involving both Western and Chinese medicines, without excluding each other. As such, the HKIIM of the CUHK initiated the first integrative medicine pilot program for MS in 2016, offering a novel platform for neurologists and CMPs to collaborate on the diagnosis, assessment, monitoring, and treatment of MS.8
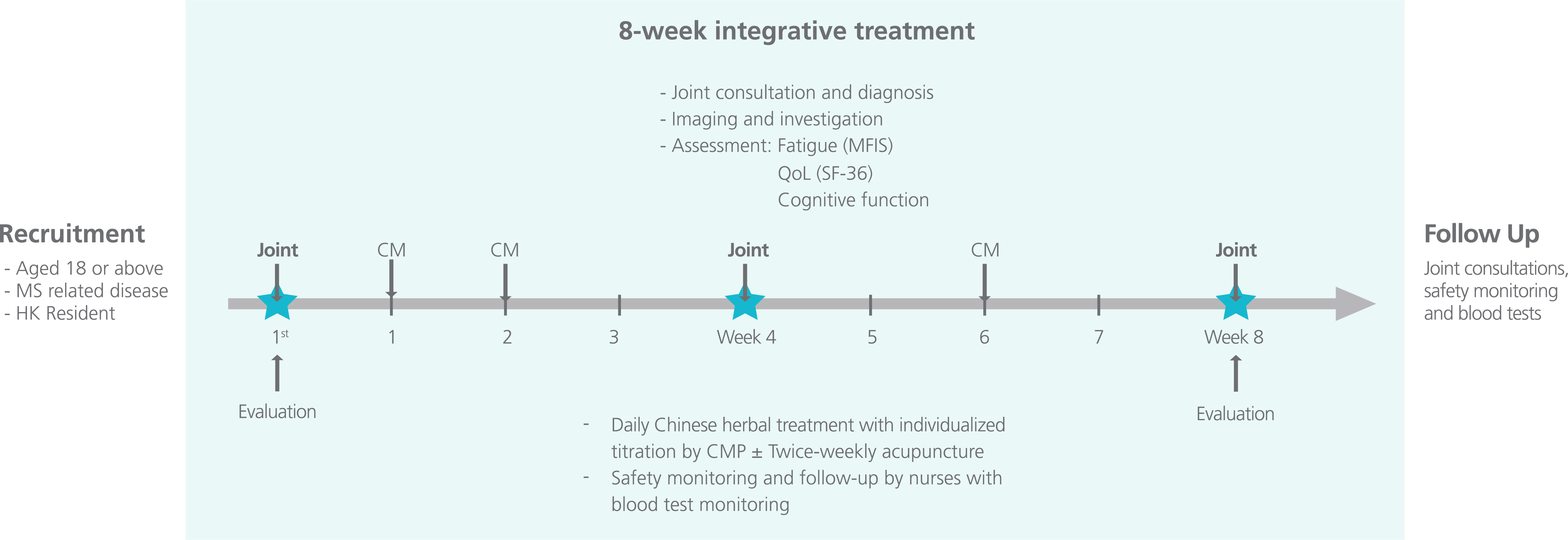
Under this program, MS patients received an 8-week integrative, semi-structured medicine approach where they were jointly managed by neurologists, CMPs and nurses at the HKIIM clinic (Figure 1).8,9 In addition to the standard-of-care pharmacotherapy backbone, patients were assessed by CMPs at the beginning of each week and received CHM and/or acupuncture as prescribed.8 Clinical toxicologists assessed the potential herb-drug interactions of the integrative approach and monitored the safety signals of those patients.8 All patients who completed the 8-week integrative program or discontinued the treatment would return to the standard-of-care management for MS.
Local case sharing under the program
In a patient treated with the aforesaid integrative approach, a 60-years-old gentleman with progressive MS was enrolled in the program due to intolerable fatigue. Although he could still exercise in the morning, he suffered from muscle pain in his two legs and had to resort to using wheelchair due to the exacerbated fatigue. In the course of 8-week integrative treatment, he reported improved stamina from the add-on CHM, resulting in reduced daily naps and increased working duration. He could get up from bed easier due to reduced fatigue and the walking test confirmed his improvement in mobility. Although he did not perceive any noticeable improvement on cognitive function, he reported reduced pain and improved bladder control that have significantly improved his quality-of-life. Since the pilot program only lasted for 8 weeks, the patient’s CHM was stopped and a marked reduction in stamina was observed afterward. He then requested to re-enroll in the program and was provided with another 3 months of CHM. During that period, he reported significant stamina recovery.
In general, a majority of patients reported marked improvement in fatigue with over 40% having improvement scores after the 8-week integrative treatment. In terms of cognitive function, neuropsychiatric tests indicated mild-to-moderate improvement, while patients reported an approximately 10 to 20% improvement only. This discrepancy in perceived cognitive function improvement can be attributed to the relatively short treatment duration and difficulty to assess subjective cognitive improvement. In terms of safety, the integrative treatment was generally well-tolerated. It was also noted that less than 5% of patients discontinued treatment due to insignificant symptom improvement or did not wish to visit the clinic on a weekly basis. No patients discontinued treatment due to adverse events.
Establishing a collaborative platform as the first step of achieving integrative medicine
Based on the 8-week pilot program, it is suggested that a more intensive CHM regimen in the early treatment phase followed by intermittent maintenance may improve disease control from pharmacotherapy, supporting the effectiveness of an integrative Western and Chinese medicine approach in managing MS. However, the clinical setting is different than the 8-week pilot program where dedicated resources were allocated to meet the needs of MS patients. In particular, patients in the real world often have difficulty in identifying a local clinician that is familiar with both Western and Chinese medicine.
During the pilot program, the HKIIM offered a platform where MS patients can receive same day and one-stop consultation from both the neurologists and CMPs. In practice, certain clinics, such as specialized cancer clinics, have multidisciplinary teams consisting of oncologists, surgeons and radiologists, who will assemble to design a comprehensive treatment plan for patients, whereas the teams are typically made up of Western medicine practitioners. In fact, many CMPs in Hong Kong have not received extensive Western medicine training, and are not licensed to prescribe medications or have the privilege to request blood tests or X-ray examinations for disease diagnosis. Likewise, many local Western medicine practitioners may have limited knowledge in Chinese medicine, and prefer only to prescribe Western medicine to avoid treatment uncertainties. Noting that Western medicine is an evidence-based medical approach whereas Chinese medicine is a holistic-based approach, therefore, establishing a systematic collaborative platform based on the pilot program is critical to ensuring routine education and communication between practitioners of different disciplines.
Under this collaborative platform, MS patients who require rapid disease control can be referred to neurologists, while those who require pain relief or physical therapies can be referred to CMPs. Whenever conflicts in treatment principles arise, specialists from other disciplines can be immediately consulted to compromise a collaborative treatment plan. In the need of certain medical services, the platform can also offer the services to both Western medicine practitioners and CMPs. Most importantly, this platform can encourage practitioners to better understand the limitations of their practices and consider the potential of utilizing treatment from a different discipline to achieve the most optimal MS management.
A takeaway to Western and Chinese medicine practitioners
The success of the pilot integrative treatment program gives rise to the opportunity of combining two diverse treatment approaches for the sake of further improving the quality-of-life of MS patients. While CHM is a locally preferred and widely accepted treatment for chronic diseases, an integrative approach with Western pharmacotherapies can help improve the cognitive symptoms and fatigue associated with MS and better manage its long-term disease course. To maximize medical care for MS patients, establishing a collaborative platform for Western and Chinese medicine practitioners would be the first step to drive a patient-centric integrative treatment approach for the better support to MS patients in Hong Kong.

