EXPERT INSIGHT
Reimagining CKM care: A local blueprint for health system transformation
The growing recognition of cardiovascular-kidney-metabolic (CKM) syndrome as a complex, interconnected health condition has prompted a paradigm shift in chronic disease management within healthcare systems.1 In Hong Kong, where aging demographics and lifestyle-related risk factors are driving a surge in CKM-related conditions, there is an urgent need for a more integrated and proactive care model.2 In an interview with Omnihealth Practice, Professor Tan, Guang-Ming emphasized the value of adopting a localized CKM health framework—one that prioritizes early detection, fosters multidisciplinary collaboration, and drives systemic reforms to enhance patient outcomes and transforms the healthcare landscape.
Seizing the moment for CKM integration
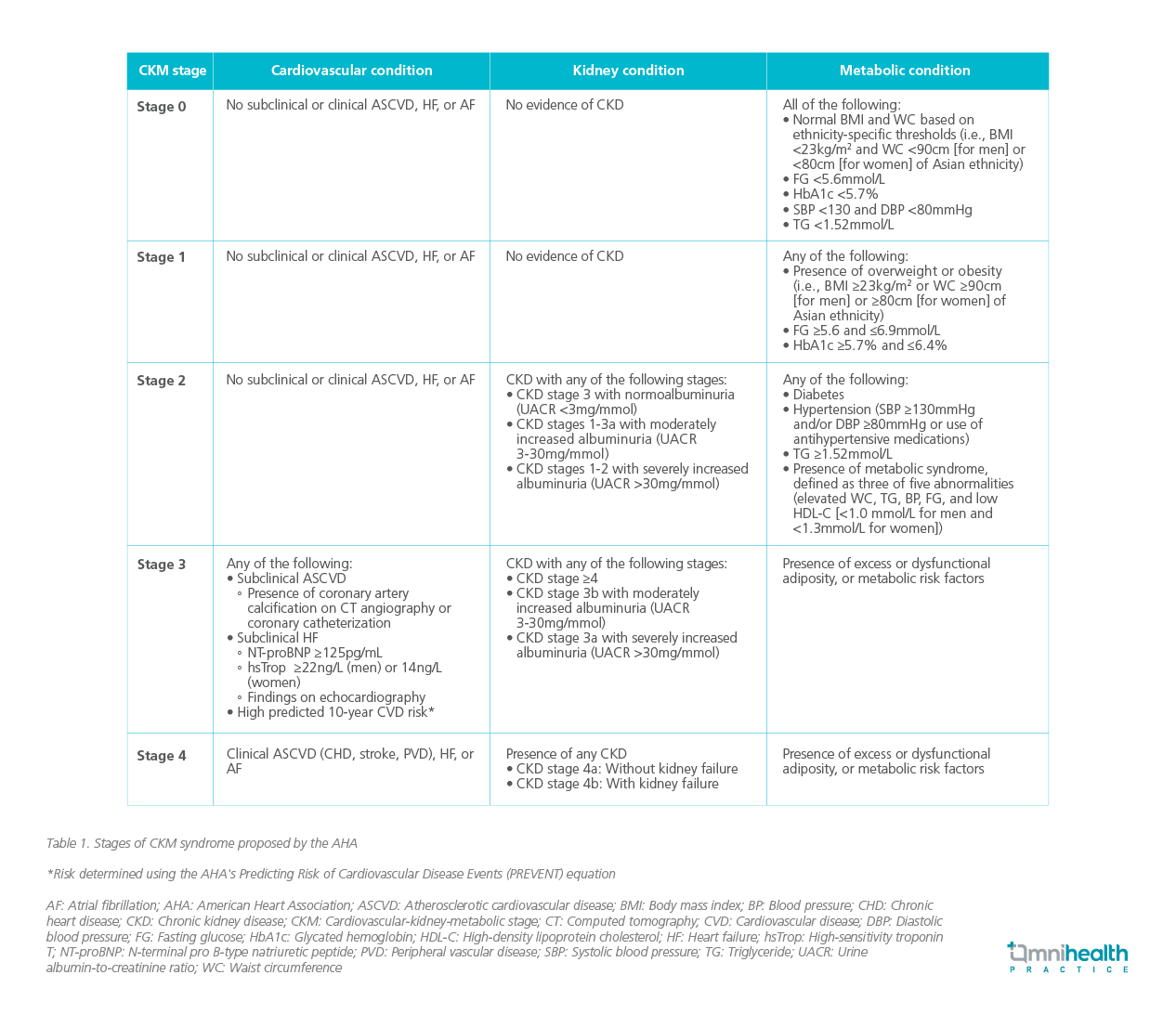
The CKM syndrome is a multi-system entity characterized by the interconnected progression of atherosclerotic cardiovascular disease (ASCVD), atrial fibrillation (AF), heart failure (HF), chronic kidney disease (CKD), excess adiposity, metabolic syndrome, and diabetes mellitus (DM) (table 1).2 The American Heart Association (AHA) coined the term in response to the emergence of two new medication classes—sodium-glucose cotransporter 2 (SGLT2) inhibitors and glucagon-like peptide-1 (GLP-1) receptor agonists—that have overlapping indications for preventing and treating diabetes, CKD, and heart disease.2 CKM conditions often coexist and exacerbate each other, highlighting the urgent need for a more integrated approach to care.3 By recognizing CKM syndrome as a comprehensive, multi-system disease, the framework promotes early detection, holistic treatment strategies, and improved long-term outcomes.2
A lifelong framework for local CKM screening and prevention
The burden of CKM syndrome is heavy worldwide and Hong Kong is no exception.1,2 Hong Kong faces a growing health burden driven by an aging population and lifestyle-related risk factors, leading to increasing rates of the CKM syndrome.1,2 Prof. Tan highlighted that “Early intervention during childhood and adolescence is critical in preventing the progression of CKM syndrome, particularly in light of the rising prevalence of obesity and metabolic disorders among youth.” As such, screening and early detection have become vital components in managing CKM syndrome.2 The Hong Kong College of Physicians (HKCP) recommends a tiered screening schedule based on individual risk levels for asymptomatic adults aged 21 and above.2 Assessments of measurements such as body mass index (BMI), waist circumference, blood pressure, lipid levels, and glycemic status, are advised every 3 to 5 years for those at low risk (CKM stage 0), every 2 to 3 years for individuals at elevated risk (stage 1), and annually for those with established conditions such as diabetes or hypertension (stage 2).2
These recommendations are consistent with the American Diabetes Association (ADA)'s guidance to screen asymptomatic adults aged 35 and older, and overweight or obese adults with risk factors, for prediabetes or diabetes every three years if no abnormalities are detected. The adoption of a unified CKM framework for early detection, fosters coordinated treatment across multiple specialties, and informs policy reforms aimed at addressing these overlapping health issues more effectively.2 Initiatives like the Primary Healthcare Blueprint, the Chronic Disease Co-Care Pilot Scheme (CDCC), and various Risk Assessment and Management Programmes (RAMPs) play a pivotal role in supporting and expanding access to screening services.2 Prof. Tan noted, “The CKM health framework can be integrated into Hong Kong’s healthcare system by leveraging its universal and well-connected public healthcare infrastructure, alongside a strong private sector, to support early detection, screening, and effective management of CKM syndrome.” These strategies aim to intercept CKM syndrome at earlier stages, ultimately reducing its long-term health and societal impacts.4
The way forward for integrated care
Building on these foundational screening and prevention efforts, the next critical step lies in transforming how CKM care is delivered—through a more integrated, system-wide approach that aligns clinical practice with the complex nature of the syndrome. As Prof. Tan emphasized, “This evolution emphasizes both vertical integration—enhancing collaboration between primary care providers and specialists—and horizontal integration, which promotes multidisciplinary cooperation across medical subspecialties.” Together, they aim to address the complex, multi-system nature of CKM syndrome more effectively.
General practitioners and family doctors play a vital role in the CKM care model, leading efforts in early detection, lifestyle intervention, and long-term monitoring.2 While medications like SGLT2 inhibitors and GLP-1 receptor agonists offer proven benefits, their use is often limited by cost, prescribing restrictions, and patient preferences.2 Moreover, important diagnostic tests such as albuminuria and N-terminal pro B-type natriuretic peptide (NT-proBNP) remain underutilized in clinical practice, despite their proven value in assessing CKM-related risks.1,2 From a primary care perspective, CKM syndrome presents a valuable opportunity to deliver holistic, patient-centered care.3 Although it can be challenging to motivate patients to take medications for asymptomatic conditions like hypertension or CKD, framing treatment around cardiovascular risk reduction—a concept patients understand—can improve adherence and engagement.3
To support this approach, public awareness must be strengthened through early detection initiatives, health-promoting environments, and reduced barriers to healthcare access.2 Continuous professional development is also essential to keep healthcare professionals updated on the latest evidence-based practices, including the optimal use of emerging pharmacotherapies and lifestyle interventions.2 Prof. Tan highlighted that community education campaigns, screening programs, and professional outreach—such as seminars, public talks, and free screening kits—can further empower healthcare providers to promote early intervention and long-term prevention.
Systemic barriers and policy solutions
To translate the vision of integrated CKM care into practice, it is crucial to understand the practical challenges faced by frontline healthcare providers. Several systemic barriers continue to hinder the effective implementation of this model in Hong Kong.2 These include limited access to essential medications, long wait times at overburdened specialty clinics, fragmented care across providers, and a lack of comprehensive local data to guide decision-making.2 To overcome these challenges, policy and system-level reforms are essential. Prof. Tan highlighted that “To support widespread adoption of the CKM framework, policy changes should focus on integrating care vertically and horizontally, relaxing prescription rights, educating primary care providers to manage complex CKM cases, empowering patients, and enhancing private-public collaboration.”
Prof. Tan mentioned a few key solutions in the CKM framework, including expanding co-care models to strengthen collaboration between primary and specialist care.2 He suggested improving access to CKM medications, increasing public-private partnerships service capacity, and leveraging digital health tools and integrated electronic health records may help streamline care coordination, enable data sharing, and support personalized patient management. Given the rising prevalence of CKM syndrome, driven by demographic and lifestyle shifts, these innovative strategies are vital to improving health outcomes and reducing the societal burden of this complex, multi-system condition.
Conclusion
The way forward for effectively managing CKM syndrome in Hong Kong relies heavily on ongoing education, research, and collaboration among stakeholders.2 Prof. Tan added that “Future research will be essential to confirm the broad, multi-system benefits of CKM medications and to evaluate the long-term impact of preventive measures, which may take years to become evident.” Ultimately, a collaborative effort among government agencies, healthcare providers, researchers, and patient groups is vital to building a sustainable, patient-centered CKM care model that effectively addresses the rising burden of this syndrome in Hong Kong.

