INDUSTRIAL ESSENTIALS
Strengthening RSV prophylaxis: Expert guidelines for pediatric practice in Hong Kong
Acute lower respiratory tract infections caused by respiratory syncytial virus (RSV) are a leading cause of hospitalization in young children.1 In Hong Kong, RSV is the primary driver of hospital admissions for children under 5 years old with respiratory viral infections, accounting for 50% of deaths in this age group.1 Among hospitalized RSV-infected patients, 39.4% required mechanical ventilation, while 21.1% needed inotropic support.1 Additionally, limited local epidemiological data further complicates this challenge.1 A single-center study (1998-2012) reported an annual RSV hospitalization rate of 157.7 per 10,000 children under five years old, with the highest burden observed in infants under one year.1 More recently, a multicenter case-control study (2013-2015) involving 3,538 pediatric RSV hospitalizations found a mortality rate of 0.14%, with 44.6% of cases occurring in infants ≤12 months old.1
Despite ongoing advancements in RSV prevention and treatment, including vaccines, therapeutic antibodies, and antiviral drugs—palivizumab remains the only available prophylactic agent.1 In Hong Kong, the government reimburses palivizumab for preterm infants (<34 weeks gestational age) with chronic lung disease requiring home oxygen therapy or medication at discharge, up to 6 to 9 months of age (maximum five doses).1 This humanized immunoglobulin G1 monoclonal antibody, which targets the RSV fusion protein, has demonstrated effectiveness in reducing RSV-related hospitalizations (RSVH) in high-risk children.1 International guidelines recommend palivizumab prophylaxis for specific high-risk groups, including preterm infants, former preterm infants with chronic lung disease/bronchopulmonary dysplasia (BPD), and children under 2 years old with hemodynamically significant congenital heart disease (hsCHD).1 However, these recommendations are primarily based on studies from temperate regions and may not fully align with the epidemiological and healthcare landscape of Hong Kong, a subtropical area.1 Furthermore, perception and variability in palivizumab use across hospitals add to the challenges of standardizing clinical practice.1
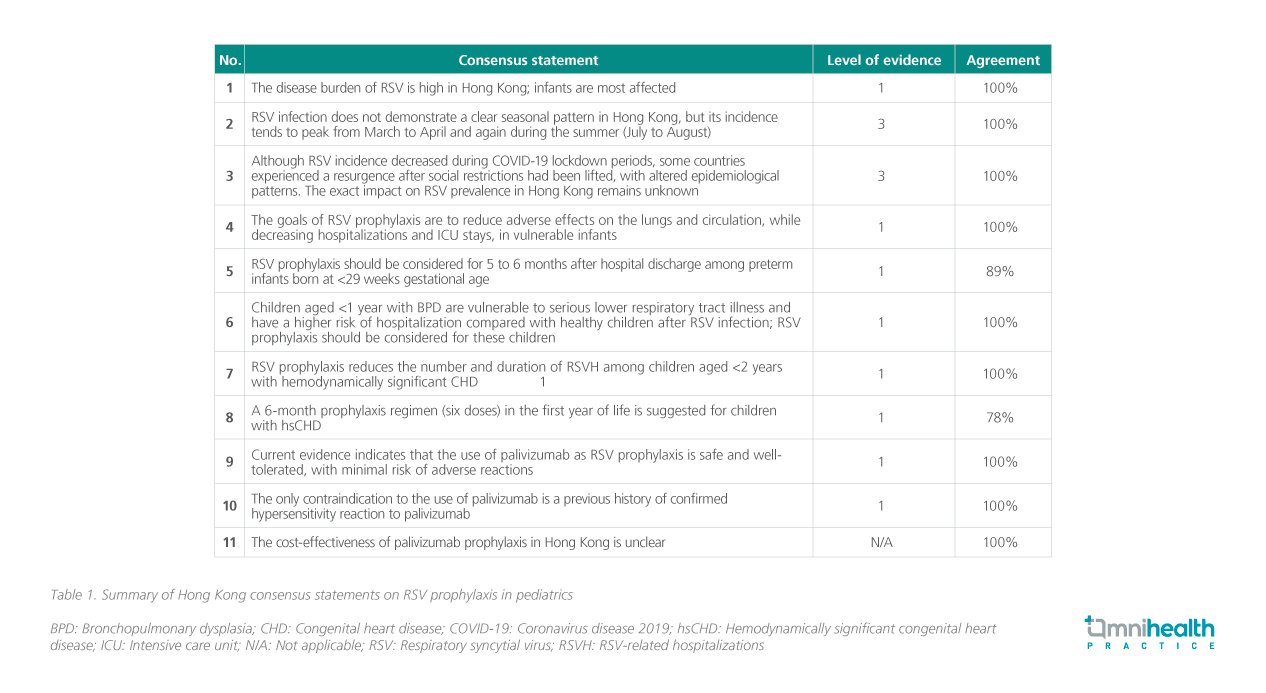
To address these gaps, a multidisciplinary panel of experts— including neonatologists, pediatric intensivists, pediatric respiratory specialists, and pediatric cardiologists from both the public and private healthcare sectors—convened to establish locally relevant consensus recommendations.1 Given the less distinct RSV seasonality in Hong Kong, the local recommendations emphasize identifying high-risk patient populations rather than seasonality-based prevention strategies.1 During the meeting, 11 statements were formulated and met consensus criteria.1 These statements, which consider the level of evidence, strength of recommendation, and agreement, were developed through literature review and expert discussion, with alignment to local reimbursement policies and the American Academy of Pediatrics (AAP) recommendations.1 The final consensus aims to provide practical guidance for RSV risk management in children, both locally and internally.1 A summary of the key consensus statements is presented in table 1.1