INDUSTRY ESSENTIALS
Unlocking the full potential of CAR T-cell therapy in R/R MM: A consensus from the IMWG Immunotherapy Committee
Chimeric Antigen Receptor T-cell (CAR T-cell) therapy has emerged as a transformative treatment for relapsed or refractory multiple myeloma (R/R MM), which remains challenging despite advances in conventional therapies.1 Targeting B-cell maturation antigen (BCMA), consistently expressed on malignant plasma cells, CAR T-cell therapies—such as ide-cel, cilta-cel, and eque-cel—have been approved for patients with refractory disease.1 These therapies, which differ in their binding domains but share common signaling mechanisms, have demonstrated high response rates and prolonged overall survival, offering new hope for patients resistant to multiple drug classes.1
Recent pivotal trials, including KarMMa-3 and CARTITUDE 4, have compared CAR T-cell therapy with standard triplet regimens in early R/R MM.1 Both studies showed superior overall response rates and progression-free survival with CAR T-cell therapy.1 However, the KarMMa-3 trial also revealed a higher rate of deaths due to adverse events in the CAR T-cell therapy group, underscoring the need for careful management of unique toxicities associated with this treatment.1
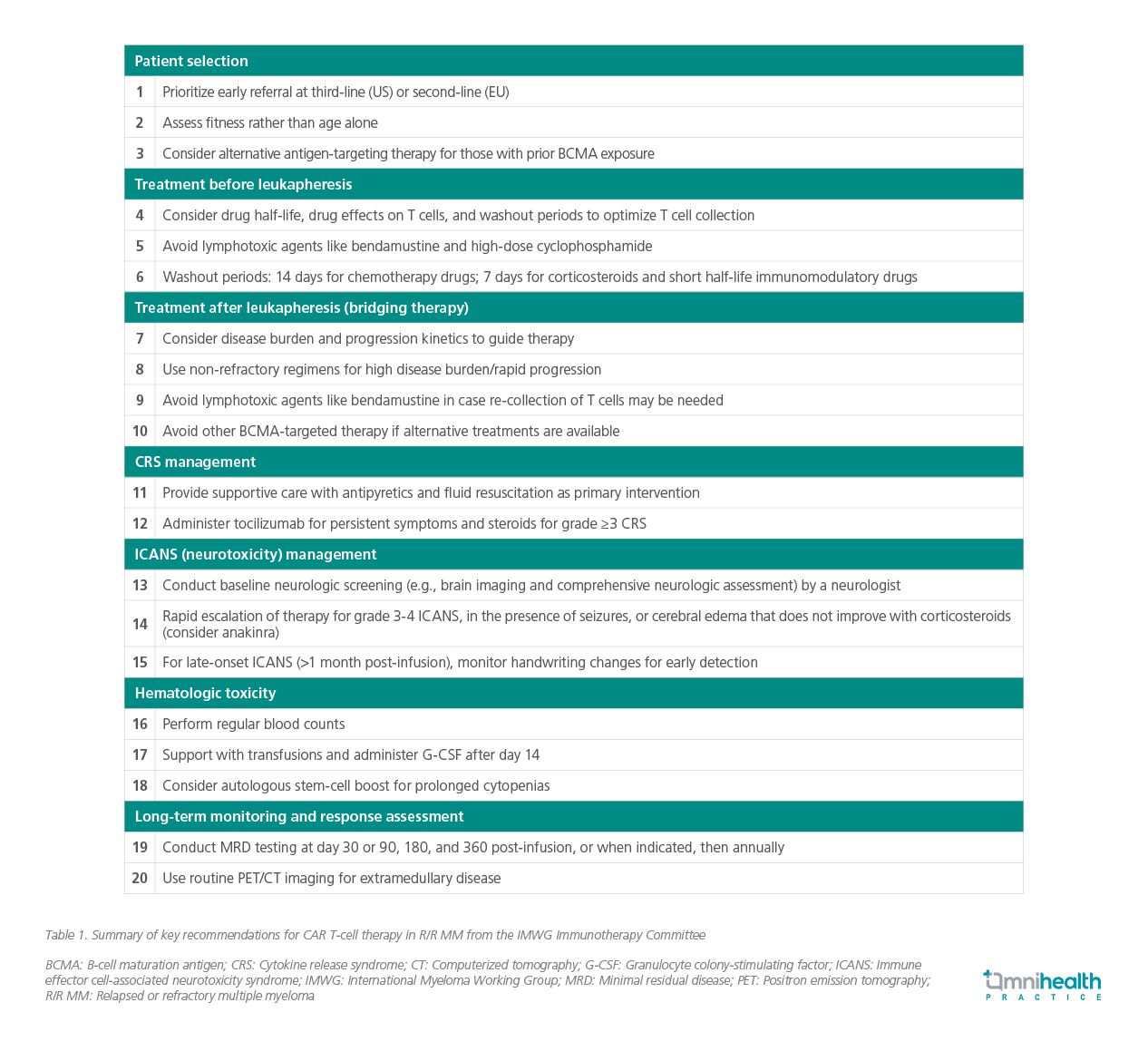
As CAR T-cell therapies continue to show promise, a panel of experts in the field of hematopoietic cell transplantation, cell therapy, and multiple myeloma therapeutics from the International Myeloma Working Group (IMWG) gathered to provide consensus guidelines to optimize the use of CAR T-cell therapy and ensure its safe and effective implementation in clinical practice.1 The consensus seeks to standardize management by offering comprehensive recommendations on patient selection, bridging therapy, lymphodepletion, response evaluations, and overall toxicity management.1 The key clinical considerations described are highlighted in table 1.1

In an interview with Omnihealth Practice, Dr. Sivakumar Palaniappan, a consultant hematologist from Malaysia, with a special interest in CAR T-cell therapy, shared his insights on the current landscape and future outlook of this innovative immunotherapy in the Asian context.

Q1: How feasible is it to integrate CAR-T therapy into the treatment landscape in Asia? What has been your experience so far, and what are the key challenges to implementation?
Dr. Palaniappan: CAR-T therapy has shown transformative potential in hematologic malignancies, particularly in refractory leukemia and lymphoma. However, its integration across Asia faces challenges such as high costs, logistical complexities, and the need for specialized centers to manage toxicities like cytokine release syndrome and neurotoxicity. Overcoming these barriers requires coordinated efforts from healthcare institutions, regulators, and industry stakeholders. Encouragingly, the region’s growing investment in cancer care infrastructure and precision medicine is paving the way for broader CAR-T adoption.
Q2: How do recent regulatory guidelines in Asia support CAR-T therapy adoption? Given the IMWG consensus on CAR-T therapy in multiple myeloma, what are the key considerations for clinical practice in this region?
Dr. Palaniappan: Regulatory frameworks, such as our local Malaysia’s Guidelines on Stem Cell and Cell-Based Research and Therapy (3rd Edition), provide ethical oversight and safety standards for CAR-T therapy, mirroring similar regional advancements. These guidelines are crucial in ensuring responsible implementation while expanding clinical access.
The IMWG consensus offers comprehensive recommendations on CAR-T therapy for R/R MM, covering patient selection, toxicity management, response assessment, and real-world applicability. In Asia, factors such as healthcare access, infrastructure, and cost constraints influence treatment decisions. While core principles of CAR-T therapy remain universal, adapting these guidelines to local settings is essential for optimizing patient outcomes. Collaborative initiatives, such as the Asian Myeloma Network (AMN) play a key role in advancing clinical research and regional treatment strategies.
Q3: Looking ahead, how do you see CAR-T therapy evolving in Asia, and what are the key priorities for ensuring its successful integration into clinical practice?
Dr. Palaniappan: CAR-T therapy is evolving rapidly, with emerging innovations such as off-the-shelf products and combination strategies (e.g., with bispecific antibodies or immune checkpoint inhibitors) expected to change the treatment landscape. However, financial and logistical challenges must be addressed to support a wider adoption. As regulatory frameworks mature and clinical data from Asian populations grow, I believe that CAR-T therapy will become increasingly integral to hematologic malignancy management across the region.

