EXPERT INSIGHT
Reforming penicillin allergy testing: A path to better antibiotic stewardship
Penicillin antibiotics are celebrated for their extensive bactericidal activity and overall safety, making them the most commonly prescribed antibiotics worldwide.1,2 However, the mislabeling of penicillin allergies poses a significant public health issue, especially in Mainland China.3-5 Current penicillin skin testing (PST) practices in the region have resulted in a concerning number of falsely labeled penicillin “allergies”.3-5 In an interview with Omnihealth Practice, Professor Philip H Li discussed a recent study from his team that critically examined the differences in PST practices between local and national settings. The study highlighted how non-evidence-based testing methods contribute to the high prevalence of incorrect penicillin allergy labels.5 Prof. Li also detailed the variations in testing practices, their public health implications, and potential strategies for reforming penicillin allergy management in China.
The complexities of penicillin hypersensitivity
Penicillins are the most widely prescribed antibiotics globally but face significant public health challenges due to high rates of mislabelling.1,2 The global prevalence of unverified penicillin allergy labels ranges from 2%-13%.1,2 In Hong Kong, about 1 in 50 individuals are inaccurately recorded as having β-lactam allergies, with nearly 90% of these labels later deemed incorrect.5 This mislabeling limits access to effective treatments and is associated with increased hospitalization rates and higher mortality, as patients are often prescribed less effective second-line antibiotics.5 In 2018, China’s consumption of ‘access’ antibiotics was only 15.1%, well below the WHO's goal of at least 60% by 2023, whereas Hong Kong’s consumption reached 62%.5 Additionally, penicillin usage among hospitalized patients in Mainland China was just 3%, compared to 57% in Hong Kong.5 The high rate of false positives in penicillin allergy testing—exacerbated by mandatory pre-emptive skin testing in Mainland China—compounds this issue.5 Misdiagnoses can result in unnecessary prescriptions of second-line antibiotics, contributing to antimicrobial resistance and preventing patients from cheap and effective treatments.5
A comparative analysis of local and national practices
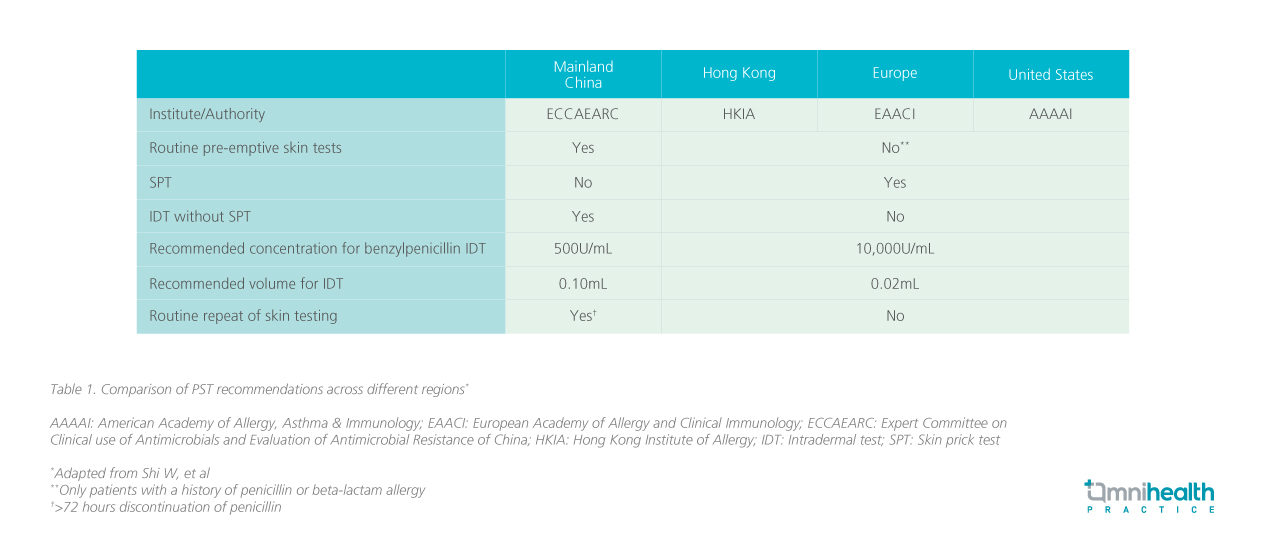
In the review article, it was highlighted that a critical difference in PST practices between Hong Kong and Mainland China lies in their timing and methodology (table 1).5
In Hong Kong, the approach generally aligns with international standards, treating penicillin allergy primarily as a clinical diagnosis that emphasizes the importance of taking a comprehensive history prior to choosing appropriate allergy tests.5 Physicians assess patients’ clinical histories, and if an allergy is suspected, they initiate PST, typically starting with a skin prick test (SPT) before intradermal tests (IDT) to confirm the diagnosis.5 While PST is a valuable diagnostic tool, it is essential to recognize that it does not replace clinical judgment, as it can yield both false positives and false negatives that may lead to misinterpretation.5
In contrast, Mainland China employs a pre-emptive approach to skin testing, with regulatory guidelines mandating that a PST be conducted before administering penicillin, regardless of the patient's medical history.5 This policy-driven requirement significantly limits physicians' discretion and flexibility. Moreover, national recommendations in Mainland China endorse conducting IDT without prior SPT.5
Prof. Li noted that while starting with IDT may be convenient for clinicians due to its greater sensitivity, it can complicate the diagnostic process, especially since it is prone to high rates of false positives depending on the methodology used.5 In Hong Kong, adherence to international protocols by starting with SPT enhances diagnostic accuracy and reduces the risk of false positives, reserving IDT for cases where SPT results are negative.5 The methodologies for conducting PST also differ significantly.5 In Hong Kong, both positive and negative controls are generally implemented using histamine and saline to mitigate the risk of false positives, particularly for individuals with sensitive skin.5 In contrast, these controls are not typically recommended in Mainland China.5 Additionally, the recommended injected volume for IDT in Mainland China is 0.1mL, which can lead to discomfort and increase the likelihood of false-positive results.5 Prof. Li highlighted that even with smaller volumes used in Hong Kong (0.02mL), challenges can still arise in administering IDT, especially for patients with a history of severe reactions.5
Pathways to improving penicillin allergy mislabeling in China
Given the significant variations in allergy epidemiology, cultural actors, and medical practices across different geographies, there will unlikely be a ‘one size fits all’ solution to drug allergy services.5 Nevertheless, while some clinicians recognize the problems associated with the overuse and misuse of IDT, less experienced clinicians, as well as those outside the allergy specialty, may operate under misconceptions and contribute to false labeling.5
Prof. Li mentioned he has encountered many practitioners from Mainland China who believe the prevalence of penicillin allergy is significantly higher in China than elsewhere, reflecting a lack of understanding of the differences in PST practices. To address this, it is essential to educate healthcare professionals about PST best practices and the limitations of preemptive IDT. Prof. Li advised doctors against automatically diagnosing patients as allergic based solely on skin test results, emphasizing it should assist – not replace–clinical judgment, and that their accuracy is heavily influenced by the methodology used. Moreover, he emphasized the importance of educating patients about the implications of a positive PST result. Once patients are labeled as penicillin-allergic, they tend to remember this diagnosis and may be reluctant to undergo retesting which has life-long implications.
Responsibility lies not just with allergists
Prof. Li remarked there is a common misconception that drug allergy issues must be addressed solely by specialists. However, this is not the only approach; non-specialists can be effectively trained to assist in managing these concerns, thereby increasing access to care. The following initiatives were highlighted to exemplify successful models that may be adopted to achieve this goal.
Hong Kong Drug Allergy Delabelling Initiative (HK-DADI)
Traditionally, evaluations of suspected penicillin allergies have required allergist involvement, limiting public access to necessary testing and treatment.7 HK-DADI, a nurse-led penicillin allergy testing strategy, serves as a successful model pioneered by Prof. Li and his team that addresses the significant shortage of allergists in Hong Kong, where the allergist-to-population ratio is among one of the lowest globally.6,7
An assessment of over 310 patients revealed that 90% of penicillin allergy labels were incorrect and subsequently removed.7 The rate of delabelling using the HK-DADI method was comparable to that of the traditional approach conducted by allergists.7 Throughout the evaluation, no patients experienced severe or systemic reactions.7 Furthermore, nurse-led evaluations resulted in a higher rate of penicillin use after delabelling compared to the traditional method (19% vs. 32% after an average of 10 months), while also reducing the need for unnecessary allergy skin tests.7
Hong Kong Penicillin Allergy Pharmacist Initiative (HK-PAPI)
In addition to HK-DADI, the HK-PAPI has been established to further address the need for specialist allergy services.8 This pilot program started in 2023 within the Hospital Authority Hong Kong West Cluster, operating alongside existing allergist evaluations.8 Pharmacists participating in HK-PAPI underwent allergy training and were certified to conduct penicillin evaluations, including performing skin testing, under the guidance of accredited specialists in immunology and allergy.8
The HK-PAPI assessed the effectiveness and safety of pharmacist-led evaluations compared to allergist-led evaluations for patients with low-risk penicillin allergies.8 In a study of 323 patients, 93.6% were successfully delabeled, with no severe or systemic reactions reported in either cohort.8 Notably, patients evaluated by pharmacists reported greater improvements in health-related quality of life (HR-QoL), with a significant change in their Drug Hypersensitivity Quality of Life Questionnaire (DrHy-Q) scores compared to those evaluated by allergists.8
Advancing Drug Allergy & Penicillin Testing (ADAPT)
In parallel, the ADAPT trial—a two-arm randomized crossover study—compared the drug allergy knowledge and self-reported confidence of practicing non-allergist physicians (general practitioners or non-allergy specialists) and nurses in Hong Kong before and after a dedicated educational intervention.9 All participants were actively practicing in Hong Kong, either in hospitals or in the community. This trial aimed to address the gaps in knowledge and confidence that many non-specialists face in managing drug allergies.9 Participants in the ADAPT trial exhibited unsatisfactory baseline knowledge (58.0) and self-reported practices (36.9).9 However, after completing the intensive course, their knowledge scores significantly improved to 77.7, and self-reported practices rose to 71.0.9 This demonstrates that with targeted training, non-specialists can effectively enhance their skills in drug allergy management, aligning with recommendations from Asia Pacific countries.9 Given the successes of HK-DADI, HK-PAPI, and the ADAPT trial, Prof. Li believes there is great potential for Mainland China to adopt similar strategies. By training non-specialists to conduct evaluations and testing, China could significantly improve the management of drug allergies, ultimately enhancing patient care and access to vital services.
Conclusion
Prof. Li concluded that “People often say, ‘Better safe than sorry.’ Many worry that failing to preemptively label patients as allergic does more harm than labeling. However, I want to emphasize the opposite–we must not overlook the lifelong implications of an allergy label.” Accurate allergy labels are crucial for effective treatment and combating antibiotic resistance. By adopting evidence-based testing methods, enhancing healthcare professional training, and fostering international collaboration, we can significantly reduce the mislabeling of penicillin allergies. Accurate allergy assessments will not only ensure patients receive the most effective treatments but also help combat the growing threat of antimicrobial resistance. Implementing these changes will pave the way for better healthcare practices and ultimately contribute to a healthier society.
"Many worry that failing to preemptively label patients as allergic does more harm than labeling. However, we must not overlook the lifelong implications of an allergy label"
Professor Philip H Li
Specialist in Immunology & Allergy,
Division Chief of Rheumatology & Clinical Immunology,
Clinical Assistant Professor,
Department of Medicine,
The University of Hong Kong, Hong Kong SAR, China
Assistant Chair of Department,
Department of Medicine,
University of Hong Kong–Shenzhen Hospital, Guangdong, China

