EXPERT INSIGHT
Redefining the management of non-muscle-invasive bladder cancer in one swoop with en bloc resection over standard transurethral resection
Bladder cancer is one of the most prevalent cancers worldwide, with non-muscle-invasive bladder cancer (NMIBC) accounting for 75% of bladder cancer cases.1-3 While the standard piecemeal transurethral resection of bladder tumor (SR) has been the conventional surgical procedure for NMIBC, oncological control remains subpar, prompting the development of alternative techniques such as en bloc transurethral resection of bladder tumor (ERBT).4,5 To examine the impact of ERBT on the prognosis of NMIBC, Professor Teoh, Yuen-Chun Jeremy and his team conducted a local phase 3 randomized controlled trial, EB-StaR, that compared the 1-year recurrence rate of NMIBC with ERBT to SR.4 In an interview with Omnihealth Practice, Prof. Teoh discussed the implications of the results and the future of ERBT implementation.
Limitations of standard piecemeal resection in NMIBC
Bladder cancer is a significant global health issue, with nearly 600,000 individuals, predominantly men over 55 years of age, diagnosed with the malignancy in 2020.2 Approximately 75% of bladder cancer cases can be classified as NMIBC, where bladder tumors are confined to the mucosa of the bladder wall (stage Ta) or demonstrate invasion to the subepithelial connective tissue (stage T1).1,3
Conventional SR, where bladder tumors are removed in a piecemeal manner from the bladder, has been the mainstay treatment in the management of NMIBC.2 As the tumor specimens obtained are fragmented, it is not possible to properly assess the resection margin.2 As such, the success rate of complete resection with this technique highly depends on the surgeon's skills and experience.4 Prof. Teoh added that residual disease may be detected in roughly 20%-30% of patients with stage T1 NMIBC upon second-look transurethral resection which is concerning.
Prof. Teoh also pointed out that floating tumor cells resulting from the SR process may reimplant onto the bladder wall, leading to disease recurrence. Indeed, the 1-year and 5-year disease recurrence rates range from 15%-61% and 31%-78% respectively among patients with stage Ta or T1 bladder cancer who underwent SR.6 As such, alternative approaches are needed to overcome the challenges of tumor fragmentation and reimplantation.
Single-piece resection ERBT as an alternative approach
In an effort to enhance the quality of the resection, the ERBT technique, where the tumor is removed in a single piece, has been introduced as an alternative approach for selected bladder tumors.4,5 With this technique, a higher-quality specimen can be obtained, which may in turn improve the accuracy of pathological staging and the completeness of the resection, and reduce the risk of tumor reimplantation.5 Currently, ERBT is available in a variety of energy modalities, including electrocautery ERBT, laser ERBT and waterjet hydrodissection.7
In 2023, a prospective, open-label, phase 3 randomized controlled trial was conducted to compare the specimen quality retrieved from ERBT and SR, which involved 384 patients with up to 3 stages Ta or T1 NMIBC tumors of 1cm-3cm in size.5 At the end of the study, the quality of tumor specimens from the ERBT group (n=192) was considered to be superior to those from the SR group (n=192), indicated by a significantly higher detrusor muscle prevalence (50.7% vs. 71.1%; mixed model p=0.01).5 Compared to SR, ERBT was associated with a lower incidence of bladder perforation (5.6% vs. 12%) and obturator reflex (8.4% vs. 16%), highlighting its more favorable safety profile.5 However, no statistical significance was observed between the disease recurrence rates of the treatment groups, leaving the long-term oncologic value of ERBT undetermined.5
ERBT demonstrated notable efficacy in reducing 1-year recurrence of NMIBC
To investigate whether ERBT offers improved oncological outcomes for patients with NMIBC, Prof. Teoh and his colleagues conducted a local randomized multicentre phase 3 trial, EB-StaR, which aimed to evaluate the effectiveness of ERBT in reducing the 1-year recurrence rate in patients with NMIBC, as compared with SR.4
Between 2017 and 2020, a total of 350 adult patients with bladder tumors ≤3cm in size were recruited from 13 hospitals in Hong Kong and randomized 1:1 to undergo either SR (n=175) or ERBT (n=175).4 74 patients were excluded due to benign histology or muscle-invasive bladder cancer (MIBC), leaving 143 patients in the ERBT group and 133 in the SR group in the analysis.4 All patients were followed up for up to 1 year after the initial surgery.4 During this period, second-look transurethral resection and intravesical bacillus Calmette-Guerin (BCG) therapy were provided as needed.4
Apart from the 1-year recurrence rate, other outcomes such as detrusor muscle sampling rate, operative time, hospital stay, 30-day complications, any residual or upstaging of disease upon second-look transurethral resection, and 1-year progression rate were also assessed.
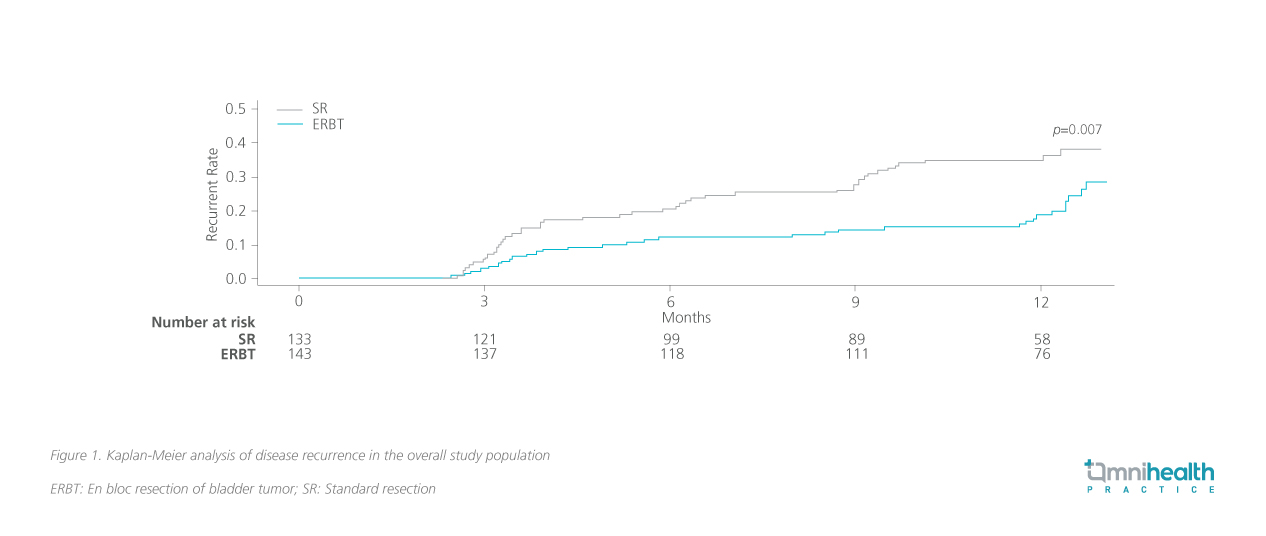
At 1 year, 31 patients in the ERBT group and 46 patients in the SR group experienced tumor recurrence.4 The ERBT group had a significantly lower 1-year recurrence rate compared to the SR group (29% vs. 39%; p=0.007) (figure 1).4 After adjusting for age and the European Association of Urology (EAU) risk group in the multivariable analysis, ERBT was found to be associated with a 43% reduced risk of tumor recurrence (HR=0.57; 95% CI: 0.36-0.91; p=0.017).4 Prof. Teoh described this finding as particularly noteworthy, given surgeons’ greater familiarity and experience with SR.
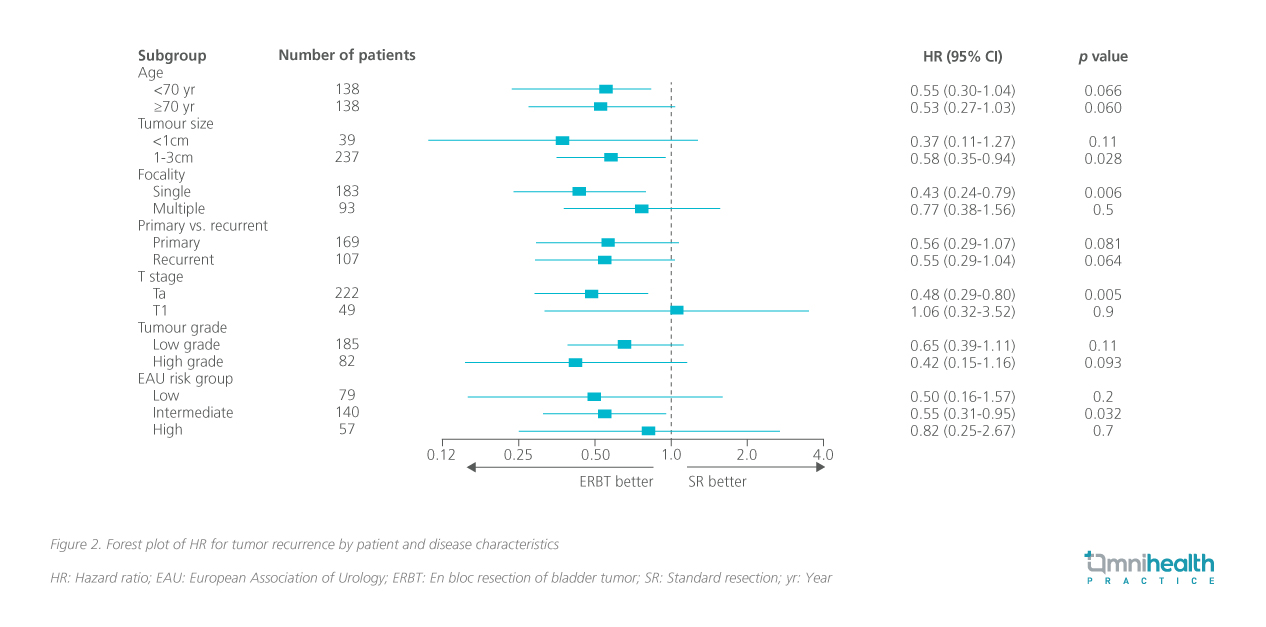
A subgroup analysis was also performed and found that in particular, patients with 1cm-3cm tumors, a single tumor, Ta disease, or intermediate-risk NMIBC as classified by EAU had a significant benefit from ERBT and that no significant difference was detected for the other subgroups (figure 2).4
In terms of secondary outcomes, no patients in the ERBT group progressed to muscle-invasive disease, compared to 3 patients in the SR group.4 The estimated 1-year progression rates were comparable between the ERBT and SR groups (p=0.065).4 The median operative time was longer for ERBT than SR (28mins vs. 22mins; p<0.001).4 Other secondary outcomes were similar between the 2 groups.4
Regarding safety, the incidence of overall complications was similar between the ERBT and SR groups (15% vs. 13%; p=0.6).4 One patient in the ERBT group developed acute coronary syndrome, and another developed pulmonary embolism.4 Importantly, no bladder perforations or mortality were observed in either group.4 As such, Prof. Teoh and his team concluded that compared to SR, ERBT offered superior efficacy in reducing disease recurrence with a manageable safety profile, further supporting its role as the standard surgical technique for the resection of NMIBC tumors ≤3cm.
The impact of ERBT in patients with high-risk NMIBC
In reviewing the 1-year recurrence data, Prof. Teoh noted that ERBT was effective in minimizing short-term tumor recurrence, with the recurrence rate remaining steadily below 20% between months 3 and 9.4 However, Prof. Teoh highlighted that there was a sudden surge in recurrence around month 12, suggesting that ERBT alone may be insufficient for longer-term prevention of recurrence, particularly among patients with high-risk NMIBC, as suggested in the subgroup analysis (p=0.7).4 Prof. Teoh highlighted that high-risk NMIBC patients are often more susceptible to tumor development due to poorer bladder health from factors such as tobacco consumption. He therefore believes that adjuvant therapies, such as intravesical BCG therapy, might need to be used in combination with ERBT to enhance its benefits in this high-risk patient subgroup.
To explore this further, Prof. Teoh and his team conducted an exploratory analysis within the phase 3 study. In this analysis, 20 patients from the ERBT group and 23 patients from the SR group received intravesical BCG therapy. During the interview, Prof. Teoh shared that while the difference was not statistically significant, the ERBT group exhibited a lower 1-year recurrence rate compared to the SR group (5.0% vs. 26.3%; p=0.059) (figure 3).
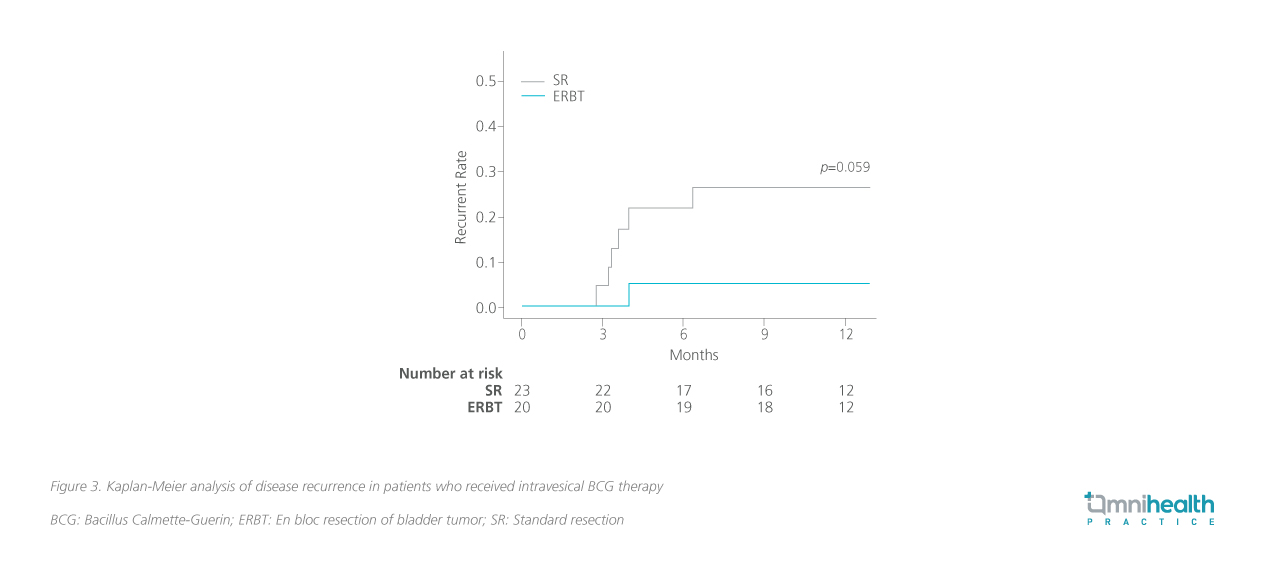
Based on these results, Prof. Teoh believes that the addition of intravesical BCG therapy could further minimize the risk of recurrence in high-risk NMIBC patients treated with ERBT. This hints at the potential research value of investigating the combination of ERBT and adjuvant therapies in future clinical trials targeting this patient population.
Future directions for enhancing the efficacy and applicability of ERBT
Aside from investigating ERBT + adjuvant therapy combinations, Prof. Teoh also emphasized that there is a plethora of unanswered questions regarding the technical aspects of ERBT and follow-up management, such as the decision to undergo second-look resection, ERBT’s compatibility with adjuvant therapies, and the frequency of post-operative cystoscopy monitoring.8 Thus, Prof. Teoh and his team have initiated the ongoing Global ERBT Registry (ClinicalTrials.gov number: NCT04934540), which aims to gather large amounts of real-world data and provide insight into the unresolved questions regarding ERBT.8 Prof. Teoh mentioned that more than 1,000 patients from 120 hospitals have already enrolled in the registry, which would be beneficial for identifying investigational topics for future randomized trials.
Prof. Teoh emphasized the importance of collaborative efforts in promoting ERBT and ensuring its effective dissemination within the healthcare community. To further support the adoption of ERBT, an upcoming meeting with local urologists has been organized to review the results of this phase 3 trial and discuss the implementation of ERBT training programs for novice physicians and surgeons. He remarked that ERBT is not significantly more difficult to learn compared to the conventional SR procedure, and can often be conducted with the same facilities and equipment.
Conclusion
In summary, ERBT demonstrated remarkable efficacy in reducing the 1-year recurrence rate in patients with NMIBC and tumor sizes of ≤3cm compared to SR.4 Additionally, the safety profile of ERBT in this phase 3 study was comparable to that of SR, indicating its potential as a viable standard treatment option for this patient group.4 Building on these positive findings, Prof. Teoh and his team will be exploring the use of ERBT in combination with adjuvant therapies, as well as collecting more real-world clinical data on ERBT outcomes globally. Importantly, Teoh emphasized that future collaborative efforts and proper surgical training programs will be crucial for the widespread dissemination and adoption of ERBT in clinical practice.4,8

