INDUSTRY ESSENTIALS
Overseeing local ocular health with a watchful gaze: Consensus on managing center-involving DME in Hong Kong
Diabetic macular edema (DME) is a prevalent cause of vision loss among individuals in the working-age population, characterized by the disruption of the blood-retinal barrier and the accumulation of fluid and serum macromolecules in the intercellular space.1 As the incidence of diabetes mellitus (DM) is projected to rise among Asian populations, a corresponding increase in the prevalence of DME is expected.1 In addition, real-world data of novel DME treatment options such as brolucizumab and faricimab have recently been published.1 To adequately address the potential increase in DME cases and incorporate the latest clinical evidence on DME medications, the development of comprehensive clinical guidelines for DME management is essential.1
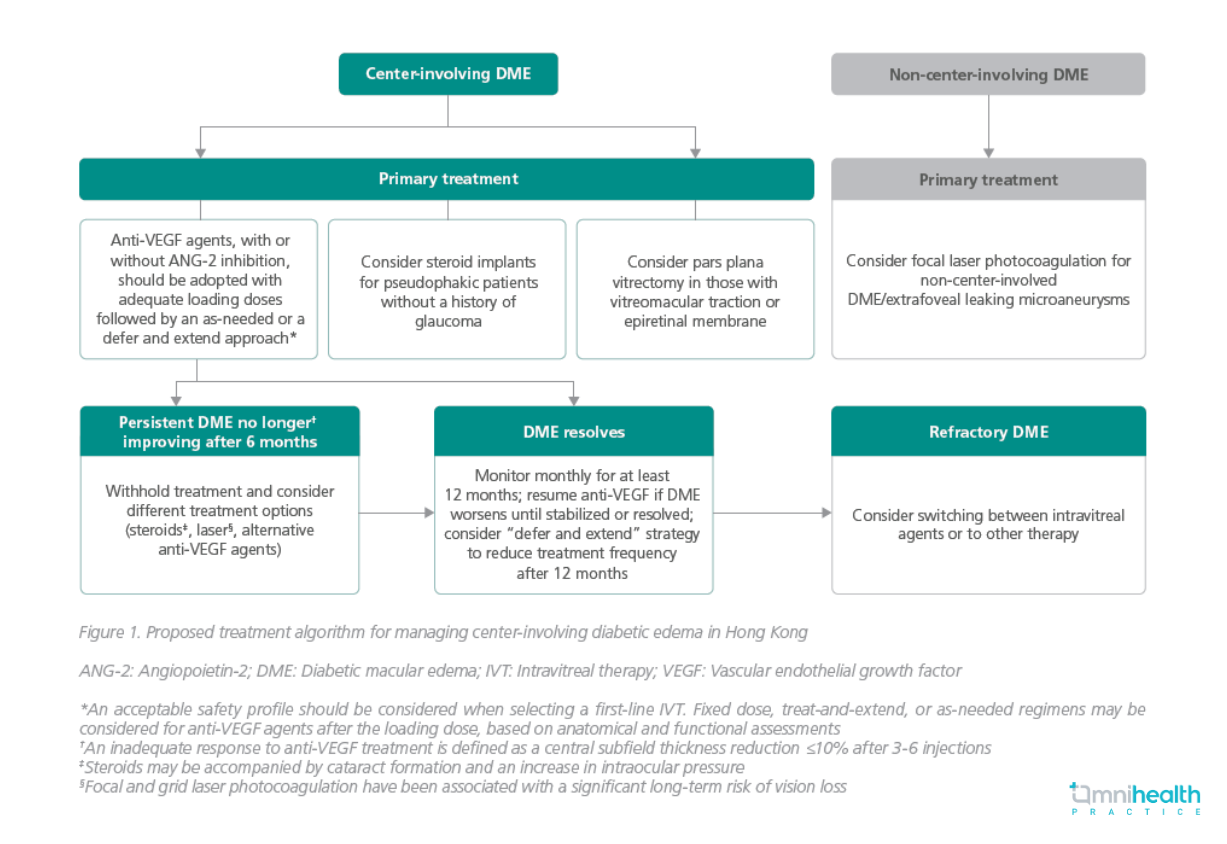
In September 2022, 8 local ophthalmologists and 1 ophthalmologist from Singapore convened to establish a set of consensus recommendations for managing DME in Hong Kong.1 A total of 15 statements regarding DME treatment goals, assessment, and options including anti-vascular endothelial growth factor (anti-VEGF) agents and intravitreal therapy (IVT), were drafted based on published evidence and the panel’s clinical experience, which were then voted on and discussed.1 After some adjustments, the finalized recommendations were of ≥80% acceptance (table 1).1 Furthermore, a treatment algorithm tailored to the specific population of Hong Kong was proposed (figure 1).1
|
DME definition and treatment goals |
|
|
Treatment options |
|

 |
In a subsequent interview with Omnihealth Practice, Professor Fung, Siu-Kay Nicholas, an ophthalmology specialist and the first author of the consensus, shared his insights on the current local practices and challenges in managing patients with DME. |
Question 1: What was the rationale behind the development of this consensus?
Prof. Fung: In Hong Kong, roughly 1 in 10 persons suffer from DM, with 10%-20% of these patients developing diabetic retinopathy (DR), a precursor to DME. Although DME only affects around 10% of DM patients with DR, it is important to recognize that the local population of DME patients is expected to continue to grow due to the rising incidence of DM. Moreover, there have been recent advancements in novel DME treatment approaches with specific protocols. It was therefore crucial to update management recommendations to incorporate the latest available options.
Question 2: What are the respective roles of anti-VEGF agents and laser treatments in local DME management?
Prof. Fung: Despite their limited durability, anti-VEGF treatments have demonstrated remarkable efficacy in the management of DME. In the initial year of treatment, patients typically receive up to 7-8 injections, with the frequency gradually decreasing in subsequent years. In clinical practice, switching therapy is uncommon and is usually considered in cases of refractory DME or when a longer-acting anti-VEGF agent is available.
On the other hand, laser treatments such as grid and subthreshold lasers have become less commonly used despite their lower cost. This shift can be attributed to the potential risk of post-operative complications associated with laser treatment. With the availability of anti-VEGF treatments, the utilization of laser treatments has gradually declined and is now primarily used as a second-line option for those with no access to or with poor response to anti-VEGF.
Question 3: What are the key challenges in the local management of DME?
Prof. Fung: Anti-VEGF agents are recommended as the first-line treatment option for patients with DME. However, the need for multiple injections to sustain ongoing management of the condition can create financial burdens for patients and contribute to challenges with treatment adherence. Moreover, since anti-VEGF treatments are commonly employed for various macular diseases beyond DME, there is a significant local demand for these injections. Compounding the issue, there is a shortage of trained personnel available to administer anti-VEGF treatments, resulting in prolonged waiting times for DME patients. As such, the development and use of longer-acting agents that offer similar efficacies with a less frequent dosing schedule are encouraged.

