EXPERT INSIGHT
Emphasizing HAE diagnosis and management in the Asia-Pacific region with SHARP guidance
Hereditary angioedema (HAE) is a rare, yet potentially life-threatening, inheritable disease characterized by episodic attacks of cutaneous and submucosal swelling.1,2 Unfortunately, the adoption and implementation of international guidelines established in Asia-Pacific (AP) populations remains limited due to a lack of expertise, infrastructure, public awareness, and access.2,3 In an interview with Omnihealth Practice, Professor Philip Li, Board Director of the Asia Pacific Association of Allergy, Asthma and Clinical Immunology (APAAACI) and lead author of a recently published epidemiologic study of HAE in the AP region, outlined the regional epidemiologic characteristics of HAE, current challenges and priority areas that require attention to optimize HAE management in the AP region. He also shared insights regarding the most recent Hong Kong-Macau Severe Hives and Angioedema Referral Pathway (SHARP) which offers guidance on patient stratification and referral strategies in patients with urticaria.
Recognizing the cycle of burden in HAE
HAE is an autosomal dominant disease attributed to SERPING1 mutations. The gene codes for C1 inhibitor (C1-INH), a type of serine protease inhibitor, regulating bradykinin metabolism which mediates swelling in HAE.1,2 The 2 types of HAE are caused by C1-INH deficiency (type I, HAE-1) and dysfunction (type II, HAE-2) respectively.1,2 According to the 2021 WAO/EAACI HAE guideline, HAE-1/2 is estimated to affect around 1 in 10,000-50,000 individuals globally.2
Prof. Li shared that most HAE patients in Hong Kong experience their first swelling episode in their 20s and 30s, which are often triggered by hormonal fluctuations, infections, inappropriate use of medications, or physical or emotional stress. He added that laryngeal attacks are the most worrying and may result in asphyxiation in 1 of 5 HAE patients. In addition, over 50% of HAE patients will experience intestinal swelling, which leads to immense pain, impairing their quality of life (QoL) and elevating their risk of anxiety and depression.
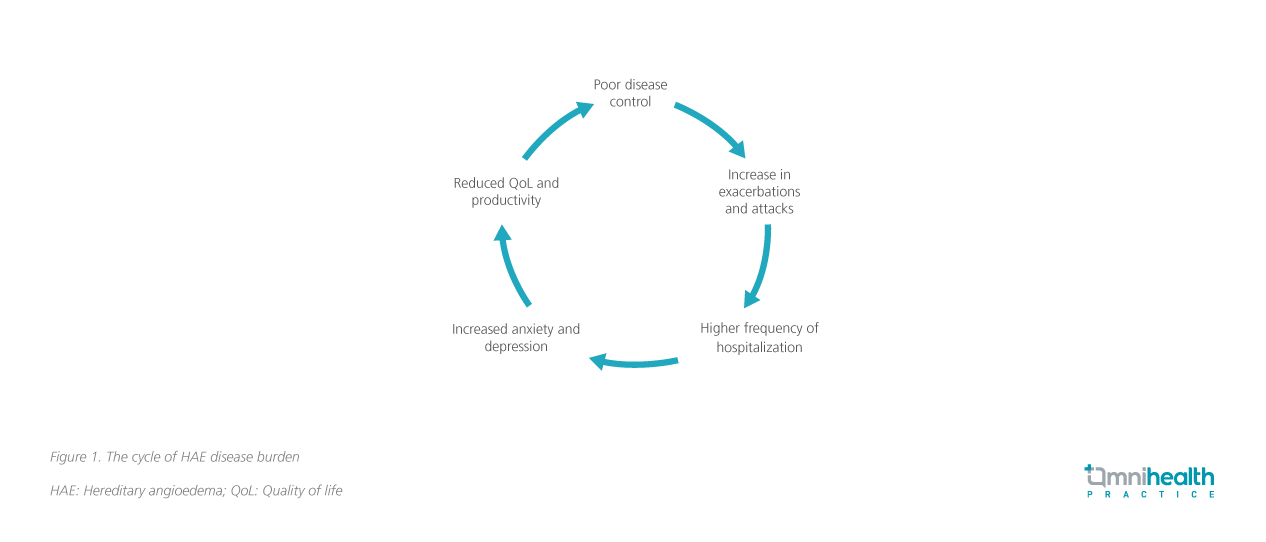
HAE attacks pose a significant burden on patients’ mental health and overall QoL.3-5 A multinational survey conducted in 2018 reported a considerable number of HAE patients had moderate-to-severe anxiety (38.0%) and depression (17.4%).3 Mental health impairments reinforce a vicious cycle of poor QoL which worsens HAE control, further increasing the frequency of attacks and hospitalization (figure 1).4 A US-based patient survey reported that up to 67.0% of HAE patients who experienced high attack rates (≥13 attacks in 6 months) believed that HAE had considerably hindered their ability to accomplish even basic daily activities.5
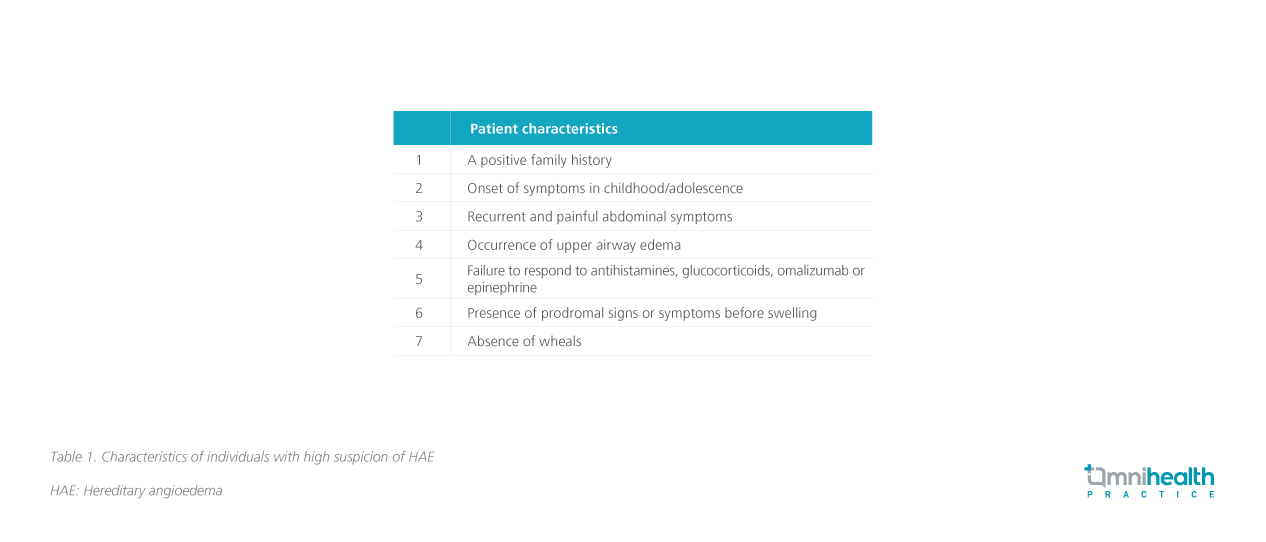
Timely diagnosis and intervention are critical factors in optimizing the clinical outcomes of HAE patients.2 According to the WAO/EAACI guideline, if a patient presents with a history of recurrent swelling of the skin (extremities, face and genitals), gastrointestinal attacks (abdominal cramps and/or laryngeal edema) and reports certain characteristics (table 1), laboratory assessments of serum/plasma levels of C1-INH function, C1-INH protein, and C4 should be performed to confirm the diagnosis of HAE-1/2.2
Reviewing HAE diagnosis and management in the AP region
Despite the significant burden of HAE, a lack of diagnostic infrastructure and limited access to HAE-specific medications has resulted in suboptimal management in the AP regions.6 To address this, Prof. Li led an international survey among experts from the AP region to explore the prevalence, needs and potential interventions for HAE management. The questionnaire consisted of 28 questions on HAE prevalence, patient profiles, and the presence of diagnostic facilities or tests, guidelines and patient support groups, and was completed by 14 expert panel members from 12 APAAACI member countries and territories with a combined population of 3.7 billion.6
The overall prevalence of HAE in the AP region was estimated to range from 0.02/100,000 to 0.33/100,000, which was vastly different from western cohorts (~1.6/100,000).6 All medical centers (n=14) had facilities for C4 level testing, but C1-INH level tests, C1-INH function tests and SERPING1 genotyping were only available in 10, 9 and 9 centers, respectively.6 The results of the study indicated that HAE-specific medications were only available in parts of the AP region.6 Amongst the 12 AP countries and territories represented, only 6 and 4 had registered on-demand (icatibant or C1-INH replacement) and prophylactic HAE-specific medications (berotralstat, lanadelumab, or long-term C1-INH replacement) for HAE respectively.6 Subsequent association analyses found that countries and territories with patient support groups were significantly more likely to have on-demand medications registered in their countries and territories, while those with regional HAE guidelines were more likely to have C1-INH replacement therapy and prophylactic medications registered.6
The diagnostic pitfalls of HAE
The international survey was the first epidemiologic study on HAE conducted in the AP region to date, which found a relatively lower HAE prevalence compared to the western population (1.6/100,000).6 Nevertheless, Prof. Li suggested that the disparity may be linked to disease detection rather than ethnic and biological variations alone.6 Misdiagnosing HAE as an allergic reaction is frequent due to similar clinical features and a lack of public awareness of HAE. He added that in Hong Kong, HAE is substantially underdiagnosed with some patients oblivious to their HAE status throughout their lifetimes.
Indeed, misdiagnosis is a persistent obstacle in HAE management.7,8 An observational study published in 2016 investigated the history of misdiagnosis among HAE patients across 11 countries.7 Among 418 patients, 44% had received ≥1 misdiagnoses before receiving a HAE diagnosis.7 These patients were significantly older at the time of correct diagnosis than those without a misdiagnosis and had a significantly longer delay from symptom onset to HAE diagnosis compared with patients who had not been misdiagnosed.7 Patients with a family history of HAE were significantly less likely to be misdiagnosed.7 Another Germany-based survey published in 2020 also found that HAE patients were most frequently misdiagnosed as having appendicitis, allergy or mental disorders.8
Prof. Li pointed out that the misdiagnosis of HAE has contributed significantly to the disease burden for patients. In most cases, antihistamines and glucocorticoids are administered to misdiagnosed HAE patients over extended periods, which are not only ineffective in relieving HAE symptoms, but also increase the risk of developing comorbidities such as diabetes, hypertension, osteoporosis, and immunosuppression.
A local framework for HAE management
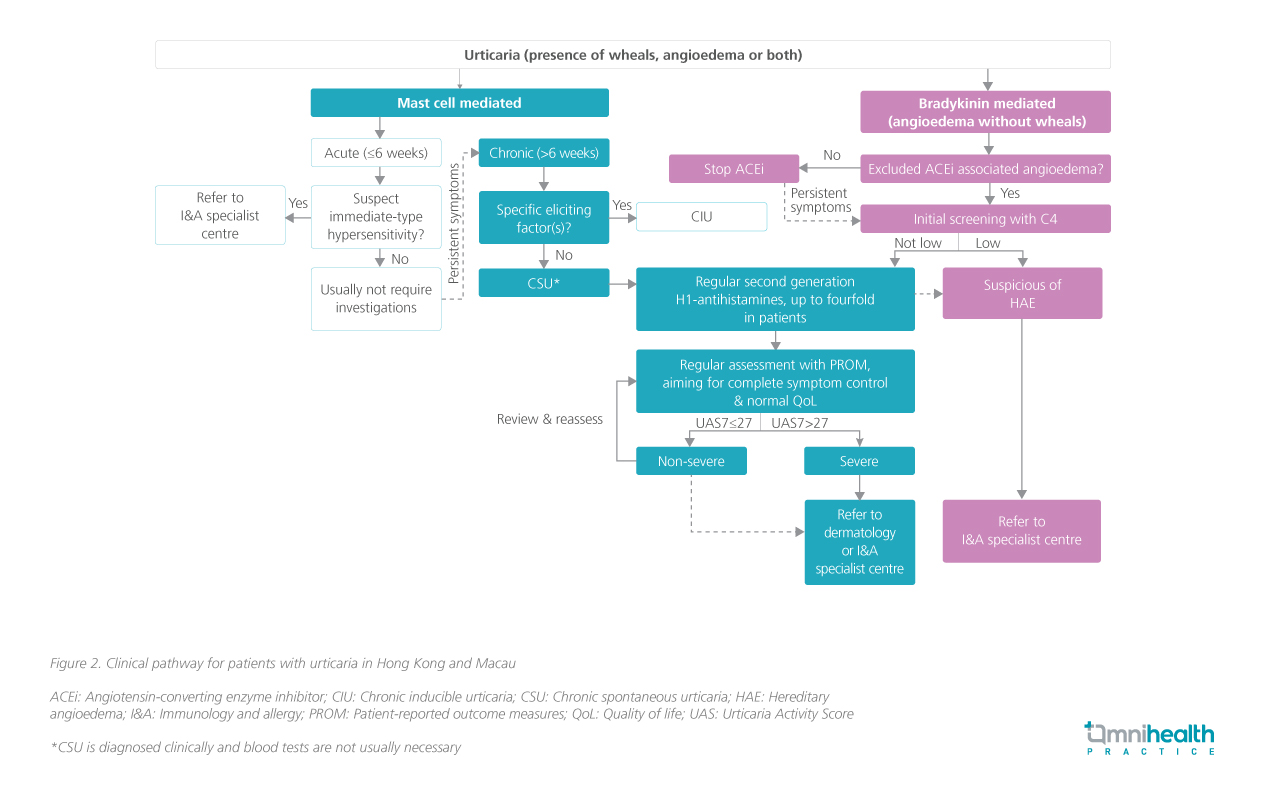
In addition, Prof. Li recognized that local physicians may hesitate to arrange referrals for patients suspected of HAE as only 1 public hospital currently has Specialists in Immunology & Allergy, which may result in delayed diagnosis and treatment. To minimize misdiagnosis and facilitate efficient screening of HAE, the Hong Kong Institute of Allergy and the Macau Society of Dermatology collaborated to develop a local referral pathway for patients with urticaria, SHARP. It serves as a guide for physicians in the diagnosis, management, and referral of patients with severe hives and angioedema, which may be caused by a range of underlying conditions including chronic spontaneous urticaria (CSU) and HAE (figure 2).9
Aside from proposing an integrated pathway, the consensus also advised physicians to refrain from administering non-HAE-specific medications (such as attenuated androgens, antifibrinolytics and fresh frozen plasma) for the treatment and prophylaxis of HAE, urging healthcare authorities to ensure the availability and accessibility of HAE-specific medications.9 As the lead author of this guideline, Prof. Li hoped that SHARP could assist physicians in differentiating and appropriately referring cases of either CSU or HAE, as well as promoting multidisciplinary collaboration in HAE management.
The fundamental role of patient advocacy and disease awareness
Aside from tailoring clinical guidelines to local settings, there is also an urgent need to improve patient advocacy.6 Prof. Li believed that increasing public awareness of HAE can drastically increase the accessibility of local HAE diagnostic facilities and HAE-specific medications. Hong Kong had no HAE-specific drugs until recently when advocacy and lobbying led by local patient support groups brought about the registration of C1-INH replacement therapy, icatibant and lanadelumab.6
Prof. Li remarked that local support for HAE patients in Hong Kong is still inadequate, citing the lack of diagnostic facilities and specialists, physician initiative and awareness, patient motivation, and financial support for HAE-specific medications under the current healthcare system. Therefore, raising awareness of HAE within the healthcare community is one of the key goals in improving local HAE management, which may be achieved via prioritizing educating primary care providers (e.g. emergency physicians and family doctors), increasing the dissemination of diagnostic algorithms, and the inclusion of HAE in medical training curricula.10
Conclusion
In summary, HAE is a rare yet debilitating and potentially life-threatening disease that is overlooked in the AP regions.6 The findings of the international survey published by APAAACI highlighted the underlying issues in HAE underdiagnosis among the AP regions, which reaffirms the necessity of establishing regional clinical guidelines and fostering patient advocacy to improve diagnosis and accessibility of HAE treatments.6 Raising awareness of HAE within the local healthcare community is also essential for reducing misdiagnosis and lobbying for additional HAE diagnostic facilities.

