EXPERT INSIGHT
Differences in hospital bed-day rates among T2D patients offer insights on management improvement
Type 2 diabetes (T2D) is a chronic disorder that can lead to a high disease burden and repeated hospital admissions due to its ability to facilitate a multitude of subsequent morbidities.1 Conventional studies often focus on investigating the risk of time-to-first events in T2D patients, giving limited insight into an individual’s disease burden.1 In an interview with Omnihealth Practice, Professor Luk, On-Yan Andrea and Professor Wu, Hong-Jiang, the co-authors of a recently published Hong Kong T2D population-based cohort study, discussed the incidence patterns of specific T2D-related medical conditions among the various subgroups of hospitalized T2D patients, as well as their implications towards the future of T2D management.
The elevated risk of hospitalization associated with T2D patients in Hong Kong
Patients with T2D often have an elevated risk of hospitalization due to comorbidities.2,3 A Taiwanese population cohort study published in 2019 found that T2D patients had significantly higher odds of hospitalization due to heart diseases, cerebrovascular diseases, malignancies, respiratory diseases, and sepsis/infection compared to healthy controls.2 Similarly, a Swedish cohort study published in 2018 reported that compared to healthy controls, T2D patients had a consistently higher risk of hospitalization for heart failure, and those who were <55 years of age with elevated glycated hemoglobin levels, low-density lipoprotein cholesterol levels, and blood pressure, albuminuria, smoking, had the highest excess risk of hospitalization for heart failure.3 Nevertheless, conventional clinical studies can only offer a restricted perception of an individual’s disease burden as they often negate nonfatal recurrent medical conditions associated with T2D.1
To investigate the correlation between T2D and hospital bed-day rate that encompasses not just conventional T2D complications, a territory-wide observational cohort study was conducted in Hong Kong which included a total of 758,254 adults with incident T2D and 758,254 matched healthy controls in the Hospital Authority (HA) database between 2002 and 2018.1 The all-cause and cause-specific hospital bed-day rates, defined as the total number of inpatient bed-days divided by follow-up time in person-years, were recorded as the study outcomes.1
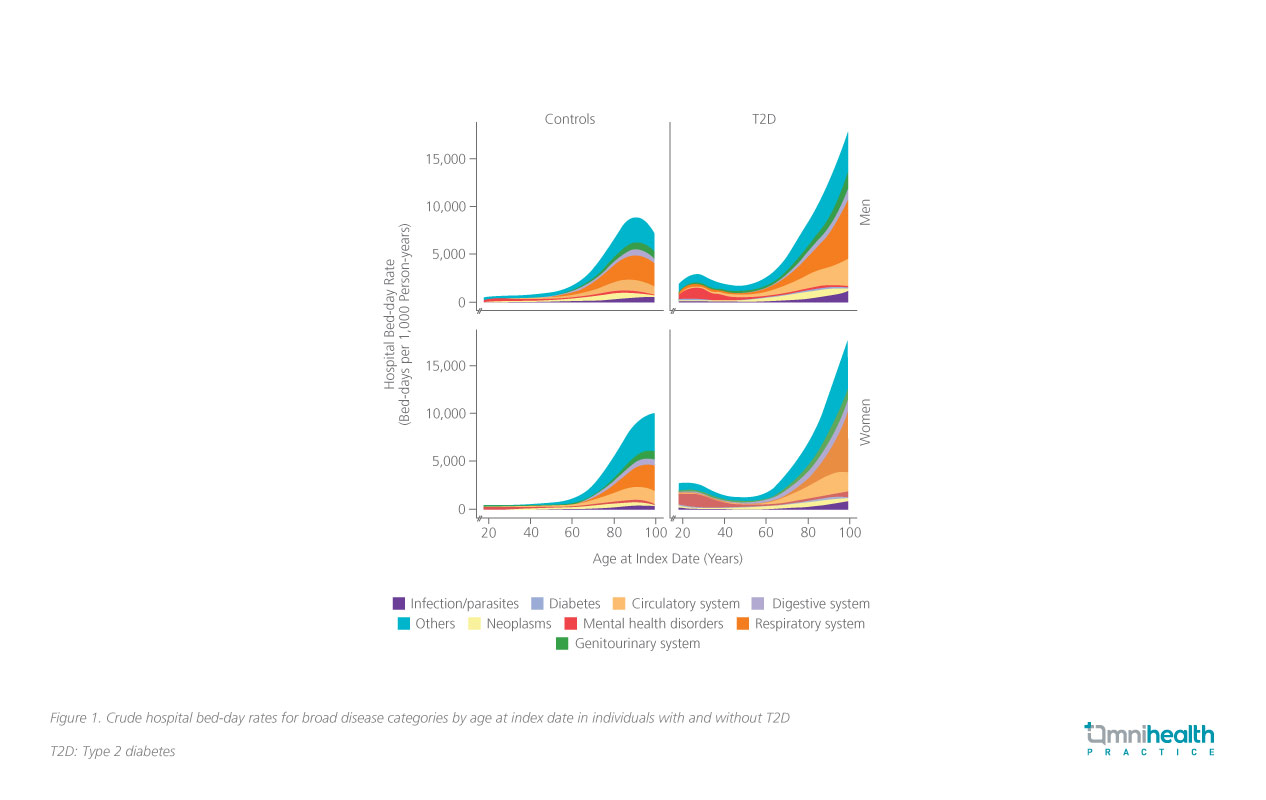
Compared to their healthy counterparts, men and women with T2D had a 1.75-fold (95% CI: 1.73-1.76; p<0.001) and 1.87-fold (95% CI: 1.85-1.89; p<0.001) increased risk of all-cause hospital bed-day rate, respectively.1 T2D was associated with the greatest risk of hospital bed-days rate due to genitourinary system diagnoses in both male and female T2D patients when compared to the healthy controls (rate ratio [RR] in men=2.94; 95% CI: 2.86-3.01, RR in women=2.64; 95% CI: 2.57-2.71) (figure 1).1 Similarly, both male and female T2D patients were also twice as likely to have an increased hospital bed-day rate due to infections (RR in men=2.11; 95% CI: 2.04-2.18, RR in women=2.30; 95% CI: 2.23-2.38) and complications in the circulatory system (RR in men=2.27; 95% CI: 2.23-2.32, RR in women=2.25; 95% CI: 2.20-2.30) compared to their healthy counterparts.1
Higher hospital bed-day rates observed in patients with young-onset T2D
The results of this Hong Kong cohort study also highlighted ageand sex-specific hospital bed-day patterns among T2D patients.1 For instance, a J-shaped relationship between the age at T2D diagnosis and the rate of all-cause hospital bed-days can be observed regardless of patients’ sex, where the hospital bed-day rates were elevated in those diagnosed at <40 years and ≥60 years compared to those diagnosed at 40-59 years (figure 1).1
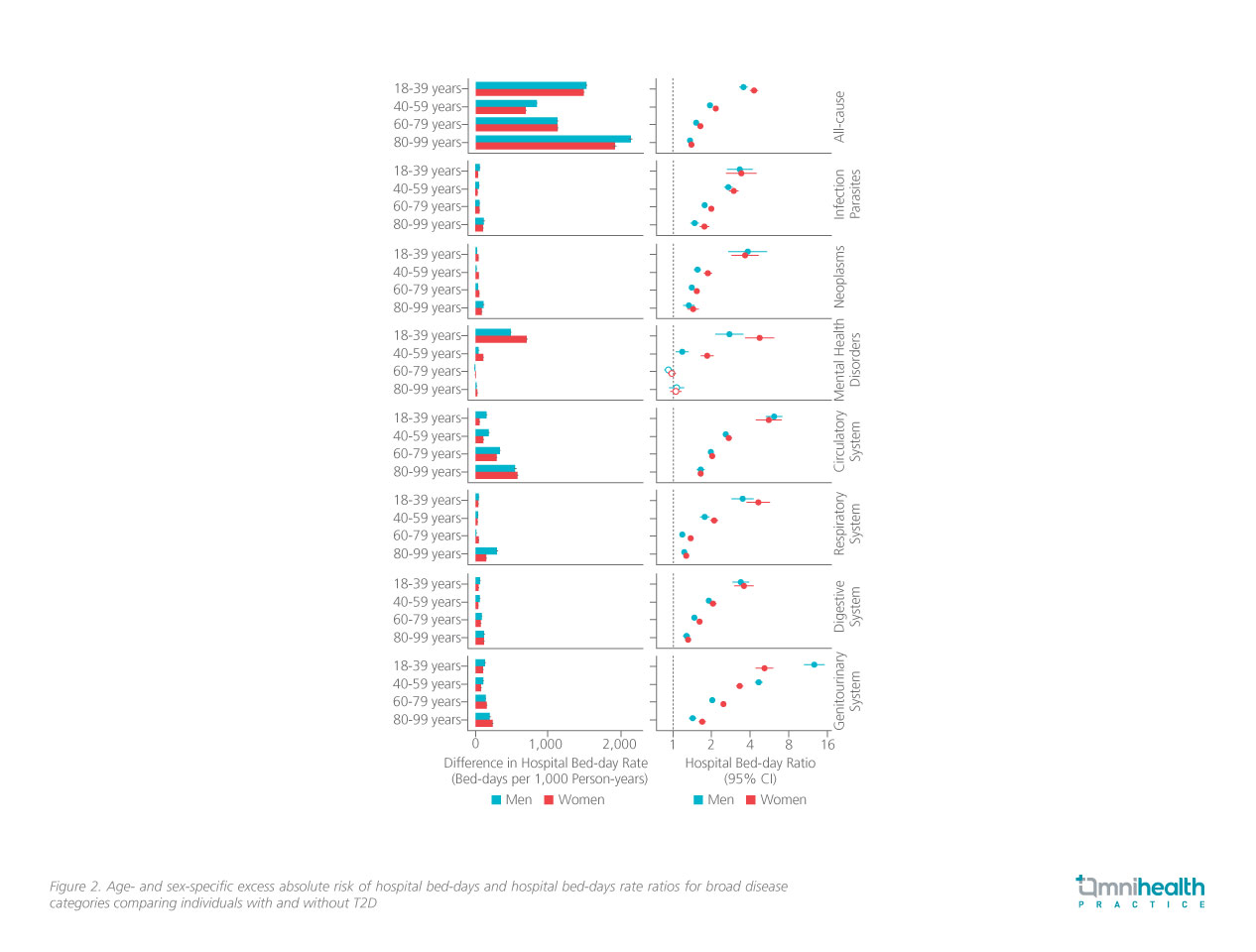
Further analysis suggested that the RRs for the association between T2D and hospital bed-day rates were significantly higher in people with young-onset T2D (figure 2).1 Patients who were diagnosed with T2D at 18 to 39 years of age were associated with an increased risk ranging from 3.54-fold (95% CI: 3.33-3.76; p<0.001) in men to 4.29-fold (95% CI: 4.00-4.60; p<0.001) in women compared to healthy controls.1,4 On the contrary, T2D patients who were diagnosed at 80-99 years of age maintain a relatively lower yet statistically significant risk of increased hospital bed-day (RR for men=1.36; 95% CI: 1.33-1.40; p<0.001, RR for women=1.40; 95% CI: 1.37-1.42; p<0.001).1,4
Prof. Wu elucidated that the emergence of prolonged hospital stays among young-onset T2D patients may be attributed to the rapid deterioration of ß-cell function, leading to a high potential of developing complications.1 He added that young T2D patients tend to have low treatment adherence, partially due to clinical inertia and patients’ personal decisions, which contributes to undesirable responses towards glucose-lowering treatments and unfavorable metabolic risk profiles, ultimately increasing their risk of hospitalization.1
Female T2D patients demonstrated a slightly higher risk ratio of increased hospital bed-day rate
Aside from age-related patterns, the risk of increased hospital bed-day rates among T2D patients exhibited sex-specific patterns as well.1 Across all 7 broad disease categories and age groups, female T2D patients demonstrated a slightly higher risk ratio of increased hospital bed-day rate compared to their male counterparts, except for genitourinary system complications in patients aged 40-59 years (men vs. women: 4.68 vs. 3.32), aged 18-39 years (men vs. women: 12.7 vs. 5.21), and circulatory system complications in patients aged 18-39 years (men vs. women: 6.15 vs. 5.63).1,4
Prof. Luk mentioned that female T2D patients are highly associated with suboptimal glycemic control performance, which can be attributed to their higher prevalence of central obesity, an indicator of reduced insulin function, compared to their male counterparts. This phenomenon is more evident among postmenopausal women. As for premenopausal women, Prof. Luk explained that maintaining glycemic control in this patient subgroup can be challenging since a majority of oral glucose-lowering drugs (OGLDs) may affect reproductive functions. With limited glycemic control options, premenopausal women with T2D are also susceptible to developing subsequent T2D-related morbidities.
Mental health disorders as a looming threat for young-onset female T2D patients
Multiple studies have demonstrated the bidirectional relationship between T2D and mental health disorders.1,5,6 Results from a meta-analysis involving 57,109 T2D patients have suggested that T2D patients possess a 3-fold and 11-fold increased risk of developing depression when evaluated by the Diabetes-Specific Quality of Life (DSQL) scale and the 36-Item Short Form Survey (SF-36), respectively.5 Similarly, another review has established that individuals with depression, schizophrenia, or traumatic life experiences have an elevated risk of developing T2D.6
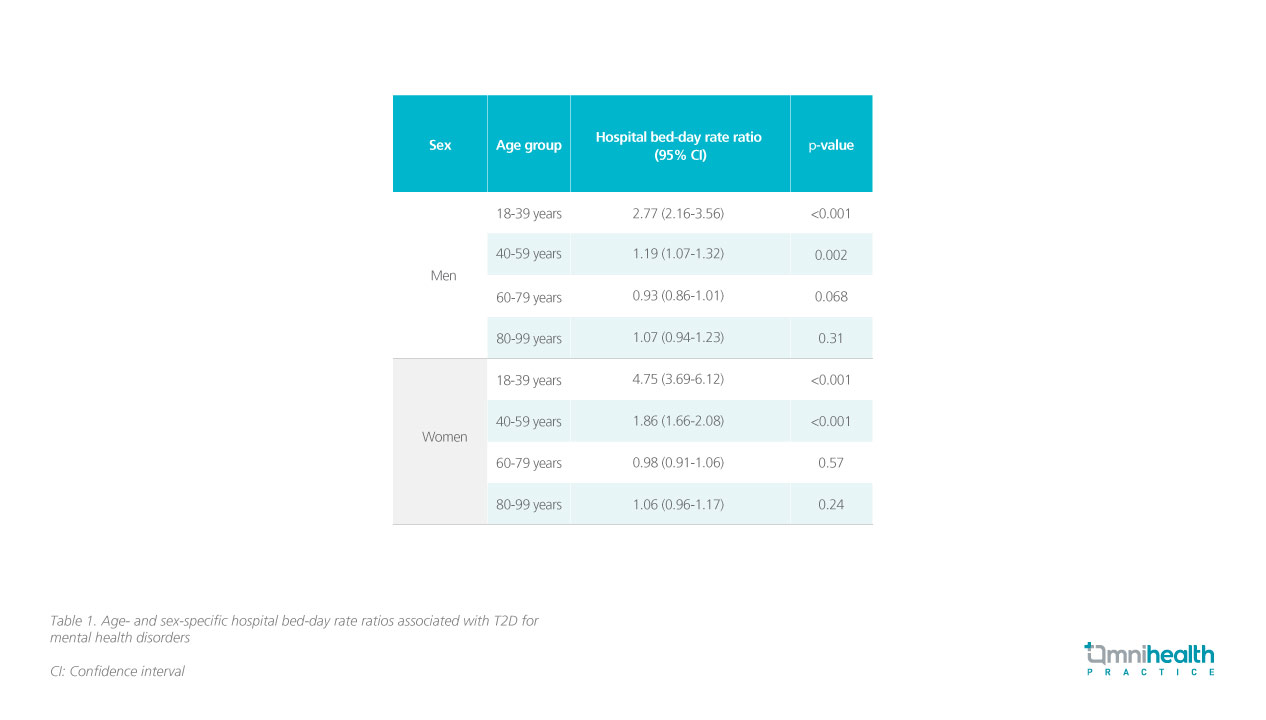
In this Hong Kong cohort study, mental health disorders constituted an overall 38.4% of hospital bed-days in young-onset T2D patients (age 18-39).1 Male young-onset T2D patients had a 2.77-fold increased risk of hospital bed-day due to mental health disorders compared to healthy controls (RR=2.77; 95% CI: 2.16-3.56; p<0.001), whereas female young-onset T2D patients experienced roughly a 4.75-fold increased risk of hospital bed-day for mental health disorders compared to their healthy counterparts (RR=4.75; 95% CI: 3.69-6.12; p<0.001) (figure 1 & table 1).1,4 Conversely, mental health disorders did not significantly impact the hospital bed-day rates of T2D patients in the “60-79 years” and “80-99 years” age groups (table 1).4
“Despite the incidence of T2D being relatively lower among young people, its development would still occur under the presence of mental health disorders such as schizophrenia and bipolar disorder, in which 60% of them occur in individuals under the age of 25. The presence of mental health disorders also contributes to an extended hospital stay for T2D patients due to their nature of disease progression and subsequent treatments,” Prof. Wu explained.1 Prof. Luk also supplemented that similar to T2D, mental health disorders such as depression and schizophrenia exhibit familial properties, suggesting that the co-existence of T2D and mental health disorders among younger patients can be attributed to genetic and lifestyle factors from their families.
Early detection and intervention for female and young-onset T2D patients
In light of the findings from this Hong Kong population cohort study, both experts urged for the implementation of more comprehensive T2D management strategies. Prof. Luk highlighted that late diagnosis age is commonly observed among female T2D patients, indicating that most women with T2D are untreated during the early disease stages. She explained that these patients may be burdened with work and family roles, resulting in them trivializing their health. Therefore, Prof. Luk emphasize d the need for public education and social /psychological support for women to raise awareness of T2D and to implement early detection and initiation of treatment for women with suspected T2D.
In the meantime, Prof. Wu emphasized that young-onset T2D patients are at a higher risk of developing mental disorders and that these disorders are often overlooked in the current standard of care, with approximately 40% of depression cases in young-onset T2D patients being undetected. He recommended that T2D care providers and mental health professionals should work together to implement integrated care for young-onset T2D patients, with psychiatric screening tests incorporated. As also suggested by Prof. Luk, these screening tests can be incorporated into the Risk Assessment and Management Programme (R AM P) launched by the Hospital Authority (HA). By doing so, early identification and intervention for common mental health disorders such as depression can be facilitated, thus effectively minimizing the hospital admission rates of young-onset T2D patients and helping provide them with timely care and support.
Conclusion
This cohort study has identified a correlation between increased hospital bed-days and certain T2D -related medical conditions among young-onset T2D patients, particularly females. Mental health disorders were found to be a significant morbidity factor for increased hospital bed-day rates among young-onset T2D patients. Therefore, future T2D preventive and management approaches should take age and sex differences into account, with a strong emphasis on early screening for mental health disorders.

