Case Review
A case sharing of early brexpiprazole augmentation to preserve QoL among MDD patients with inadequate response to prior ADT
Approximately 3% of the Hong Kong populace experience an episode of major depressive disorder (MDD) in their lifetime.1 Some of these patients may have an inadequate or partial response to initial antidepressant therapy (ADT).2 Many atypical antipsychotics (AAPs) are used as augmentation for these patients, however, they often come with a myriad of adverse effects (AEs).2 Newer generation AAPs like brexpiprazole are prime candidates for augmentation, particularly among young and high-functioning patients who are concerned with AEs like hyperprolactinemia, sedation, weight gain, and extrapyramidal symptoms (EPS).2 In an interview with Omnihealth Practice, Dr. Li, Ching-Kwok Rico shared a clinical case of a high-functioning 29-year-old woman who had inadequate response to multiple lines of ADT treatment. He had addressed her reservations about augmentation therapy after repeated failure on different lines of ADT, and provided comprehensive counselling to help her achieve functional recovery instead of simply focusing on symptomatic control. The timely introduction of brexpiprazole had helped her attain rapid mood improvement as well as restore functions across her social, family, and work life.
Background
Guiding MDD patients through partial or inadequate response with AAP augmentation
Selective serotonin reuptake inhibitors (SSRI) remain the current first-line standard of care (SoC) option for MDD patients, followed by a switch to serotonin and norepinephrine reuptake inhibitors (SNRI).3 Augmentation with antipsychotics would be used after this line of therapy if results are unsatisfactory.3 In the interview, Dr. Li recommended that comprehensive psychoeducation should be offered to patients early. “Different lines of treatment and the evidence-based treatment algorithm stated in guidelines should be introduced early during counselling as well”. Such discussion helps patients approach treatment with a foundational understanding such that they are “aware of the expected choices and timeline of response.” Despite having unsatisfactory response to ≥2 different classes of antidepressants, patients who had received comprehensive counselling may remain hopeful and motivated. They may be better prepared psychologically and be more receptive to consider augmentation therapy or a relatively longer-term treatment.
Laying the groundwork of augmentation with a solid therapeutic alliance
Dr. Li reflected that many patients, particularly in the private sector, are motivated to learn more about their conditions. Most of them would access internet resources on their own, but the information might be incomplete, leading to a misunderstanding of their condition and available treatment options. He noted that misinformation is particularly apparent among young and working patients, where occupational function and sexual AEs are concerning aspects of both the disease and treatment. Doctors should approach the needs of their patients from their point of view and explore how to address functional impairments on top of their MDD symptoms.
He put a strong emphasis on the importance of effective communication and a robust therapeutic alliance, referring to the collaborative and affective bond between therapists and their patients.4 Studies have correlated a strong therapeutic alliance with improved treatment outcomes.4 Treatment providers should establish rapport by being non-judgmental and avoiding excessive use of medical jargons.5 Using open-ended questions and communicating the rationales behind treatments are also useful in establishing trust and rapport.5 Through a shared decision-making process and thorough discussion of life engagement goals, doctors can gain a more comprehensive understanding of the concerns and preferences of their patients. Ultimately, this helps resolve issues that negatively impact patients’ vocational function and contribute to their chronic fatigue like anhedonia, low energy levels, reduced occupational function, and concentration loss.
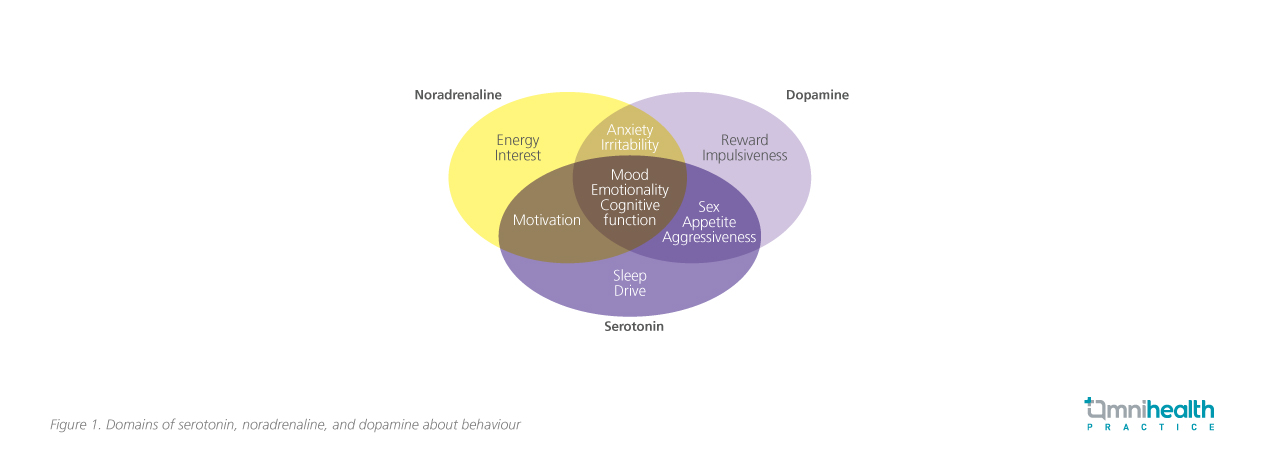
Dr. Li stated, “provided that in the early phases of treatment, patients are educated on the mechanisms of ADT and an evidence-based algorithm, there would not be much difficulty in convincing them the addition of AAP is the right move for treatment-resistant depression (TRD).” “Simple illustrative diagrams can help patients to better understand the rationale and enhance their acceptance and drug adherence.” To illustrate his point, he provided us with a live demonstration where we assumed the role of his patient. With the succinct diagram (figure 1), Dr. Li provided a comprehensive overview of his counselling approach, which covers the neurotransmitters and mechanisms involved behind different ADTs, as well as the indications of different lines of treatment, which helped manage patient’s expectations on when later-line treatment would be needed.5
Dr. Li further explained that better understanding of potential AEs of specific medication classes can help patients be more aware and willing to articulate their concerns with their healthcare provider in a more precise and accurate manner. Psychiatrists, in turn, can better adjust the treatment according to the needs of the patient. In the following case sharing, Dr. Li demonstrated how effective communication and early introduction of brexpiprazole augmentation helped a high-achieving patient suffering from TRD.
Case sharing
Miss Y is a 29-year-old lady with good past health and no history of psychological conditions. She was born into a prominent family in Beijing and came to Hong Kong as an expatriate in 2020 to work in a middle management role at an international asset management corporation. She is a smart and diligent young lady who can be summarised as a perfectionist with a strong sense of duty. She has always been one of the top performing staffs at her previous employments. However, she has been facing multiple stressors since she took up a new position in Hong Kong. The unexpectedly prolonged economic downturn related to the coronavirus (COVID-19) pandemic complicated by a relationship crisis with her boyfriend triggered her depressive episode.
She began to suffer from insomnia with early morning wakening and crying spells. At work, she was tired and had lost her focus and concentration. She reported losing motivation and passion in her work, which was new to her. This compiled into negative cognitions of self-doubt and feelings of worthlessness with fleeting suicidal ideation. Additionally, she suffered from uncontrolled binge eating episodes prior to important work meetings or after a long stressful day at work. As a result, she suffered from on-and-off stomachache and heartburn which progressed to gastritis and oesophagitis, subsequently requiring an oesophago-gastro-duodenoscopy (OGD), after which she was referred for psychiatric assessment.
Miss Y was diagnosed with MDD after consultation. After discussion, she agreed to start with an SSRI as a short-term, low dose anxiolytic and a hypnotic for her insomnia. She was prescribed with citalopram and was gradually titrated up to 40mg once daily (QD). However, she suffered from gastrointestinal (GI) symptoms at a higher dose, which may be attributed to a combination of limited symptom control, the AEs of SSRI, and persistent binge eating episodes. The control on her mood symptoms was also inadequate, so she was switched to desvenlafaxine. However, after an adequately long observation period, there was only marginal improvement in symptom control. She became concerned with the limited response which worsened her negative cognitions of worthlessness, leading to a vicious cycle of guilt and binge eating. Subsequently, desvenlafaxine was switched to vortioxetine 5mg QD, which was titrated up to 10mg QD. There were partial mood improvements but due to the mounting work stress and relationship issues, her binge eating episodes and negative cognitions were not under satisfactory control.
Noting that she was very eager to improve, Dr. Li proposed the addition of a dopamine control component to her treatment plan. Brexpiprazole 0.5mg QD was started early in June 2023 and the response was prompt and prominent. Though there were reports suggesting brexpiprazole may worsen compulsive symptoms and affect eating disorder symptoms, it was not observed presently. Since Miss Y’s binge eating was closely related to her anxiety and mood symptoms, tackling the depression helped alleviate the binge eating episodes. She reported no more binge eating after the first week of brexpiprazole augmentation. Noting the positive response, the dose was further up titrated to 1mg QD. Counseling on a healthy and balanced diet was also provided. With brexpiprazole augmentation, her condition showed remarkable improvement by September. No akathisia or other EPS was reported. There was no impact on her menstrual cycle. Alongside the improvement in her mental condition, Miss Y was offered a promotion opportunity to be transferred to the company headquarters in Beijing in October 2023 and she is on track to maintain the current regimen with a longer follow-up period.
Discussion
Managing expectations with lower dose range and AE profile in augmentation
Dr. Li shared that a low dose of brexpiprazole is often effective in providing a “kickoff effect” for mood improvement. He highlighted that patients may be more comfortable with adding a “little add-on intervention” to their pre-existing regimen given the small pill size and dose of brexpiprazole. Dr. Li mentioned that young and working patients may not tolerate some of the AEs associated with augmentation that some atypical antipsychotics and mood-stabilizing agents bring. Brexpiprazole was chosen for its superior AE profile, leading to minimal impact on appetite, body weight, menstrual cycles, and sedation. Such low incidences of AEs may also help convince patients to consider treatment augmentation for a prompt response.
The unique profile of brexpiprazole as a selective serotonin dopamine activity modulator (SDAM) gives it a distinctive receptor affinity profile, which contributes to achieving a balance in major depressive disorder (MDD) treatment, offering calming effects without inducing sedation and allowing them to reengage without overactivation.7 In a 26-week study of patients pooled from 3 randomized double-blinded, placebo-controlled trials, adjunctive brexpiprazole of up to 0.5-3mg* has demonstrated good tolerability of up to 52 weeks with most treatment-emergent AEs (TEAEs) being mild to moderate in severity.2 The mean increase in body weight was 2.7kg at week 26 and 3.2kg at week 52.2 No clinically relevant findings of EPS, prolactin, lipids, or glucose were reported.2
Assessing efficacy endpoints from the perspective of young and high-functioning patients
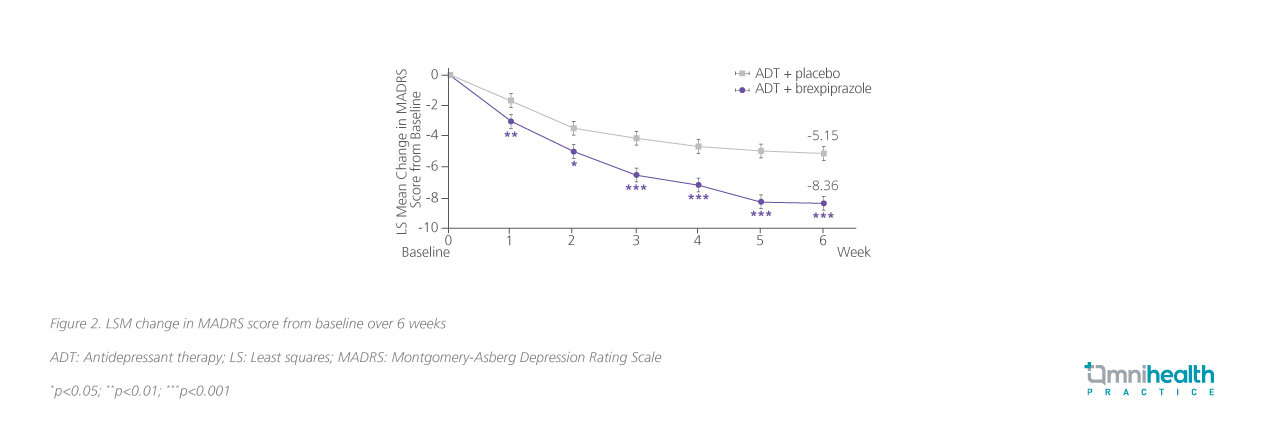
After an in-depth discussion with the patient, Dr. Li recognizes that she has a strong desire to resume her vocational functions. Thase ME, et al conducted a study in 2015 in which patients with inadequate response to 1-3 previous lines of ADT were randomized to receive brexpiprazole 2mg QD or a matching placebo on top of their ADT.8 They found a significant (p=0.0002) reduction in least squares (LS) mean change in Montgomery-Asberg Depression Rating Scale (MADRS) score by an additional 3.21 points at 6 weeks of treatment (figure 2).8
When assessing MDD recovery outcomes, Dr. Li remarked that life function comes first. MDD patients typically experience dysfunction across multiple domains including social, work, and family functioning.9 Life engagement provides a holistic view of treatment outcomes through assessing positive impact on different health aspects relating to cognition, which most clinical assessment scales could not adequately reflect.7
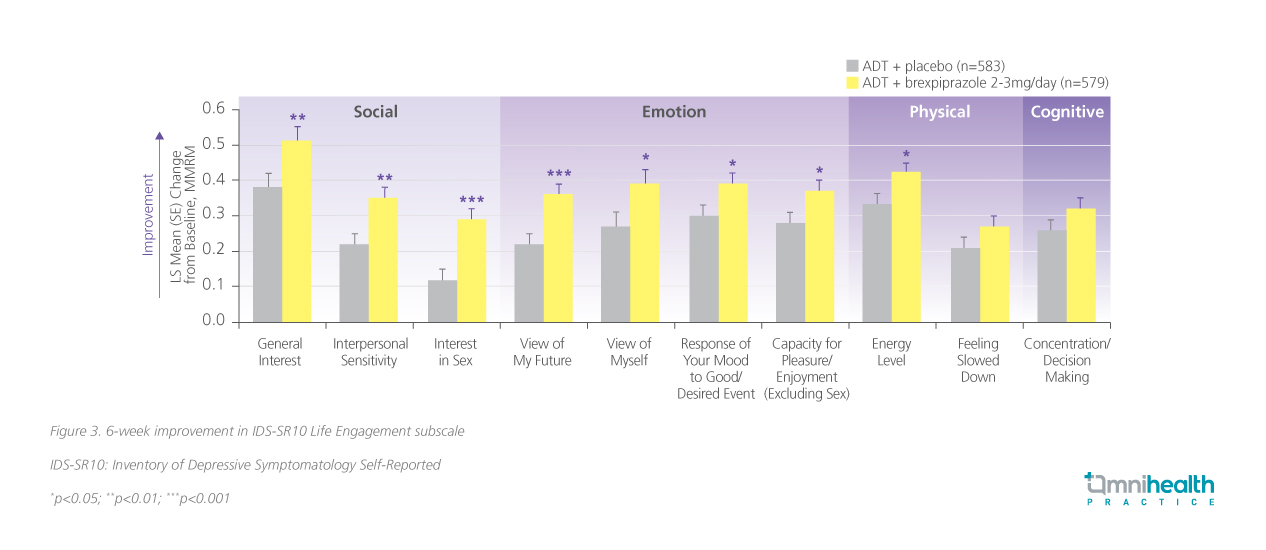
In another study conducted by McIntyre RS, et al where the effects of adjunctive brexpiprazole on life engagement in MDD patients showed that brexpiprazole augmentation offered significantly greater improvement over placebo in terms of the Inventory of Depressive Symptomatology Self-Report (IDS-SR10) Life Engagement subscale over 6 weeks (LS mean = -1.19; 95% CI: -1.78 to -0.59; p<0.0001) (figure 3).10 The Life Engagement subscale consisted of 10 items including the response of mood to good or desired events, concentration and decision making, view of oneself, view of one’s future, general interest, energy level, capacity for enjoyment or pleasure, interest in sex, feeling slowed down, and interpersonal sensitivity.10 Short-term results of the pooled analysis from 3 randomized double-blinded trials of ADT + brexpiprazole 2-3mg* QD (n=579) and ADT only (n=583), were recorded at 6 weeks post-treatment initiation, and long-term results were reported in an open-label extension of up to 52 weeks.10 Notably, at each weekly follow-up visit, statistically significant improvement in the placebo group were maintained consistently (p<0.01).10 In the extended study period, the mean improvement persisted in across all 10 Life Engagement items, with a 2.4 points improvement at week 26 and a 3.7 points improvement at week 52 respectively.10
Conclusion
In conclusion, Dr. Li reminded us that laying the groundwork for a strong therapeutic alliance with patients and informing them about the treatment protocol in early phases of treatment may facilitate better treatment adherence and improve the acceptance of augmentation therapy. Brexpiprazole, a drug with a unique mechanism of SDAM and a desirable AE profile, is a suitable option for augmentation therapy in MDD.7 It also helps patients achieve better life functioning over 6 weeks with lasting improvements over long-term follow-ups.10 Moreover, brexpiprazole has minimal impact on body weight, sedation, movement side effects, prolactin level, and metabolic syndromes, making it a good choice for young, high-functioning patients.2 Therefore, Dr. Li recommends early consideration of augmentation therapy in TRD in this particular patient population with brexpiprazole and other similar AAPs.
*Note that in Hong Kong, brexpiprazole is only indicated as an adjunctive therapy to ADT in adult patients with MDD at a starting dose of 0.5-1mg QD, up to a maximum of 2mg QD. 3mg dose has not been approved currently in Hong Kong.