CONFERENCE UPDATE: EULAR 2023
SEC and SDZ-ADL show similarly low radiographic progression in axSpA patients
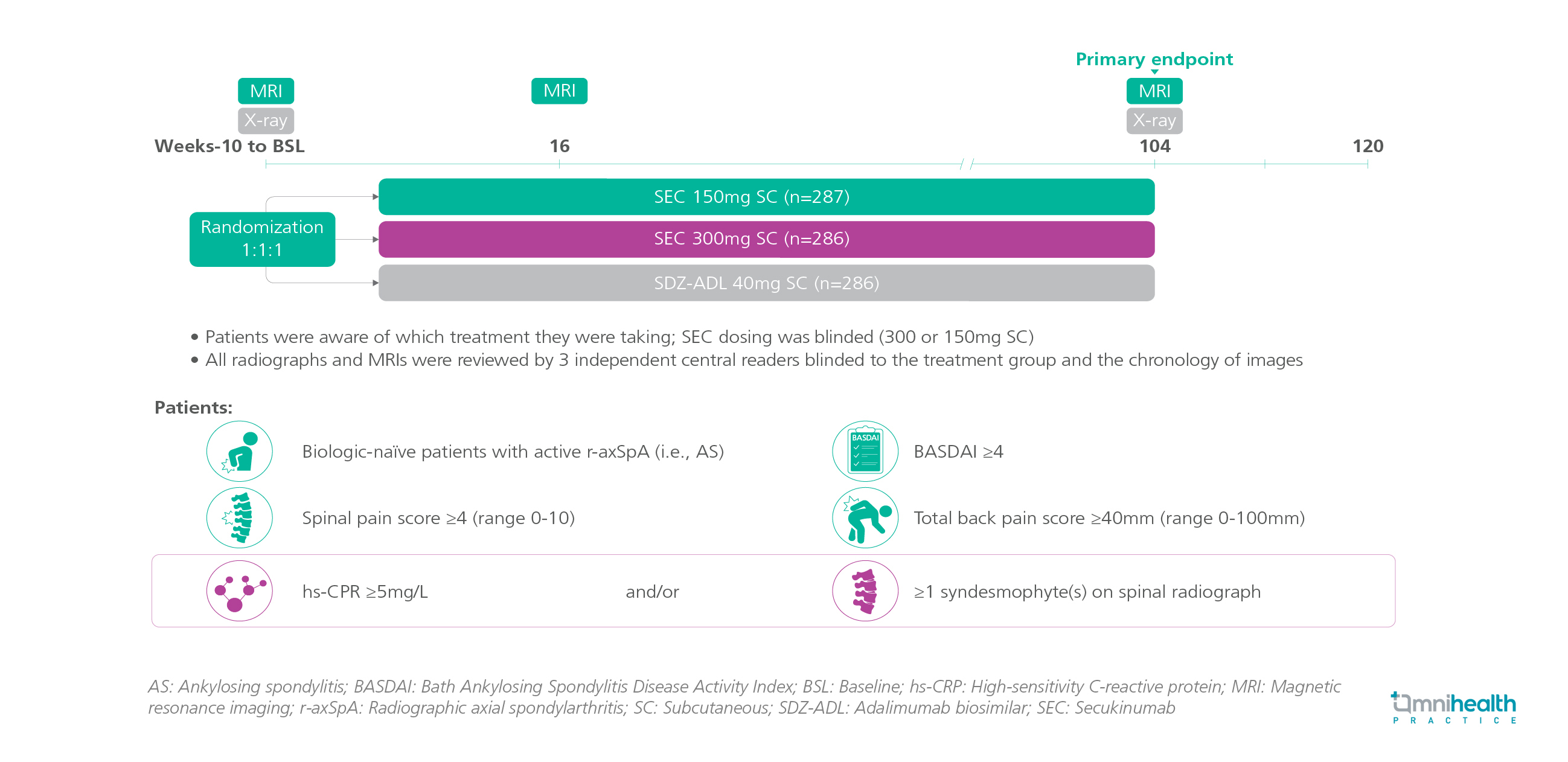
STUDY DESIGN
The prevention of potentially irreversible structural damage is an important goal in the management of axial spondylarthritis (axSpA).1 Currently, there are limited data regarding the effects of biologic disease-modifying anti-rheumatic drugs (bDMARDs) on slowing radiographic progression in patients with radiographic axSpA (r-axSpA).1 The MEASURE 1 trial showed low rates of radiographic progression after 2 years in r-axSpA patients being treated with secukinumab (SEC).1 A head-to-head study, SURPASS, was carried out to compare the effects of SEC and adalimumab biosimilar (SDZ-ADL) on radiographic progression.1
SURPASS was a 2-year, partially blinded, randomized, active-controlled, phase 3b trial that involved 859 biologic-naïve patients with active r-axSpA who had a Bath Ankylosing Spondylitis Disease Activity Index (BASDAI) spinal pain score ≥4, total back pain score ≥40mm, high-sensitivity C-reactive protein (hs-CPR) ≥5mg/L and/or ≥1 syndesmophyte(s).1 In this trial, patients were aware of the treatment, while physicians were blinded to it.1 Patients were randomized 1:1:1 to receive SEC 150mg, SEC 300mg, or SDZ-ADL 40mg subcutaneously (SC).1
The findings showed that the proportion of patients with no radiographic progression, as defined by the modified Stoke Ankylosing Spondylitis Spinal Score (mSASSS) ≤0.5, was similar across all groups.1 The change from baseline (CFB)-mSASSS at week 104 was consistently low across all groups.1 Also, consistencies across all groups were the cumulative distribution of CFB-mSASSS, the proportion of patients without new syndesmophytes at week 104, as well as the reduction and distribution in the sacroiliac joint oedema score and the spine oedema score.1 The frequency of most adverse events (AEs) was similar and no new safety signals were observed.
FINDINGS
|
Primary endpoint: |
|
|
|
Secondary endpoints: |
|
|
|
|
|
|
|
Safety: |
|
|
|
"Spinal radiographic progression over 2 years was low with no significant difference between SEC and SDZ-ADL."
Dr. Xenofon Baraliakos
Ruhr-Universität Bochum, Bochum,
Rheumazentrum Ruhrgebiet, Herne,
Germany

