CONFERENCE UPDATE: AHA 2022
Diagnosis and management of aortic disease: The 2022 ACC/AHA clinical pactice guideline
A team of specialists has recently organized an education session at the American Heart Association (AHA) Scientific Sessions held in November 2022, reviewing the highlights of the new American College of Cardiology (ACC)/AHA Aortic Disease Guideline.1,2 The members of the writing committee presented a new evidence base for aortic disease patients, also sharing the importance of decision-making, the necessity of a team approach, and developing genetic discoveries.1,2 The experts presented 2 subsections under the topic of “Aortic Disease Team Management”- the first was on “Imaging”; and the second was on “Multiple Disciplinary Care and High-Volume Centers”.1,2
All recommendations are assigned a Level of Evidence (LOE) and Classification of Recommendation (COR) developed previously by an expert task force.3 The COR reflects the strength of the recommendation, which includes the expected scale and certainty of benefit to risk.3 The quality of scientific evidence supporting the intervention is indicated by the LOE, which grades this evidence based on the nature, volume, and consistency of data from clinical trials and other reliable sources.3
LOE
- Level A: High-quality evidence from ≥1 randomized controlled trial (RCT); meta-analysis of high-quality RCTs; or ≥1 RCT corroborated by high-quality registry studies
- Level B-randomized (B-R): Moderate-quality evidence from ≥1 RCT; or meta-analysis of moderate-quality RCTs
- Level B-nonrandomized (B-NR): Moderate-quality evidence from ≥1 well designed, well executed nonrandomized studies, observational studies, or registry studies; or meta-analysis of such studies
- Level C-limited data (C-LD): Randomized or nonrandomized observational or registry studies with limitations of design or execution; meta-analysis of such studies; or physiological or mechanistic studies in human subjects
- Level C-expert opinion (C-EO): Consensus of expert opinion based on clinical trial
COR
- Class 1: Strong; Benefit>>>Risk
- Class 2a: Moderate; Benefit>>Risk
- Class 2b: Weak; Benefit≥Risk
- Class 3: No benefit (moderate); Benefit=Risk
- Class 3: Harm (strong); Risk>Benefit
Imaging:
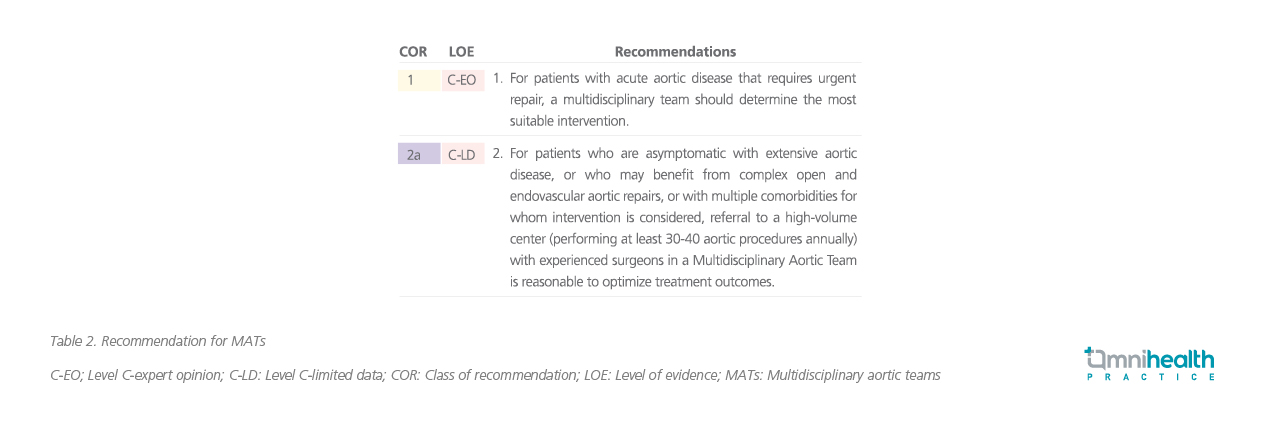
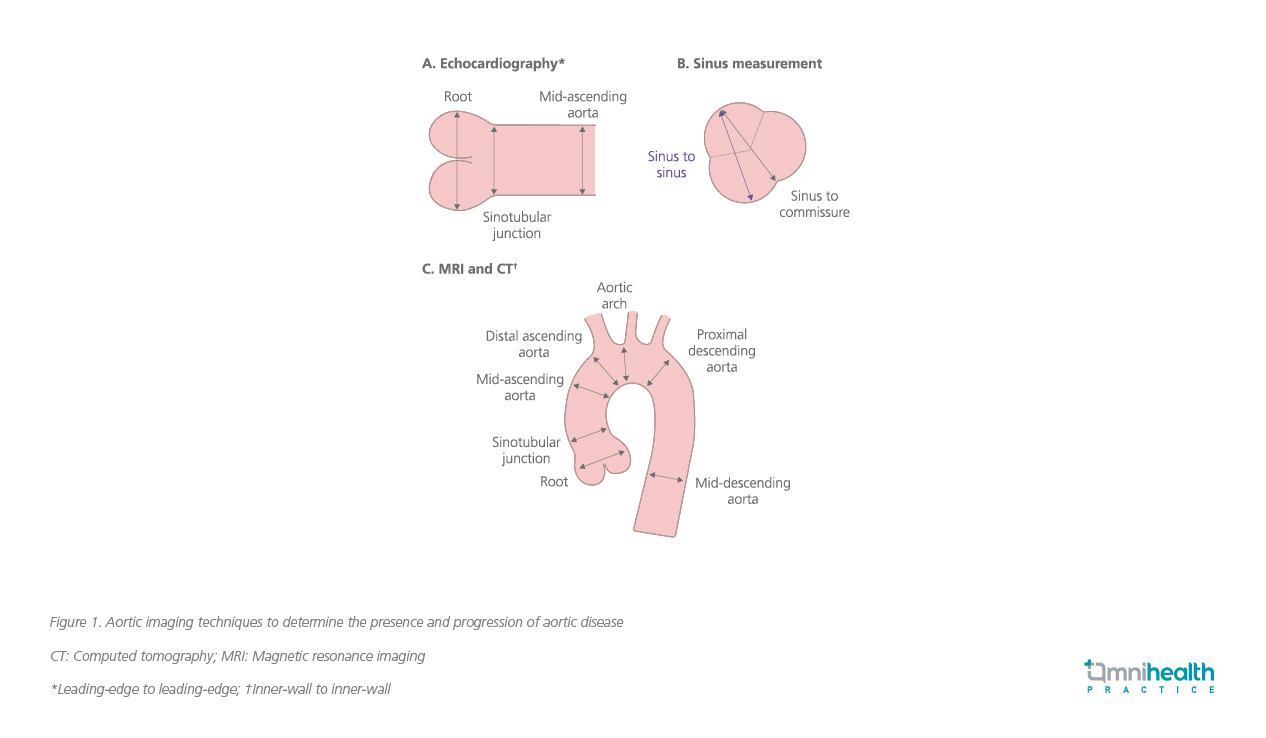
Measurement techniques preferred for different imaging modalities were presented.1 The 3 most common modalities used to assess the aorta are echocardiography, cardiac computed tomography (CT), and magnetic resonance imaging (MRI).1 Standard measurement locations and preferred measuring techniques for each of these 3 modalities, and recommendations for aorta imaging techniques to identify the presence and progression of aortic disease (figure 1 and table 1).1,3
Measurement techniques
- The guideline still proposes the leading-edge to leading-edge technique for measuring the aortic root and the ascending aorta via echocardiography
- Inner-edge to inner-edge measurement is preferred in MRI and CT
- The importance of reporting the largest diameter, particularly in asymmetric aortas such as the bicuspid valve is emphasized
- It is important to utilize a consistent method when using MRI and CT to measure all 3 sinuses
- Both the largest measurement and a cross-sectional area should be reported if possible
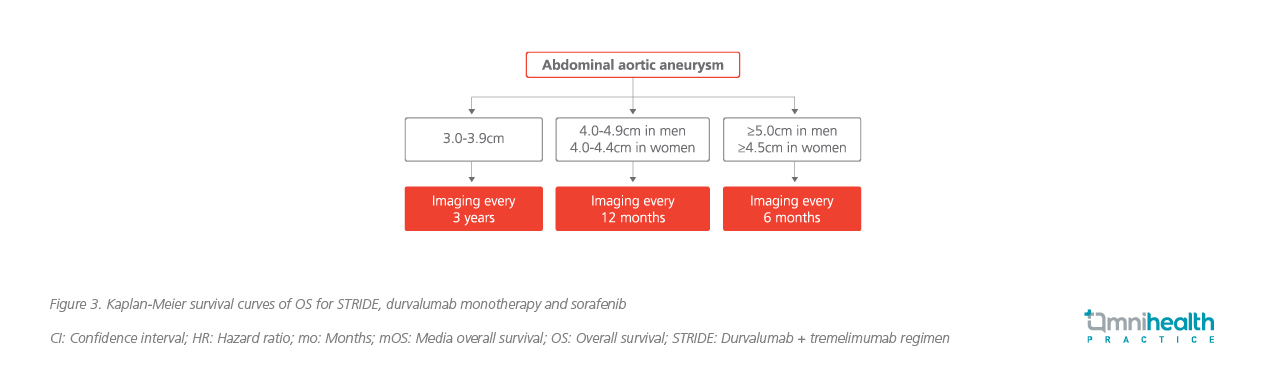
Based on the current aortic diameter, a Class 1 algorithm recommendations for the frequency of surveillance imaging of abdominal aortic aneurysms in men and women using ultrasound is given below (figure 2).3
Multiple disciplinary care and high-volume centers:
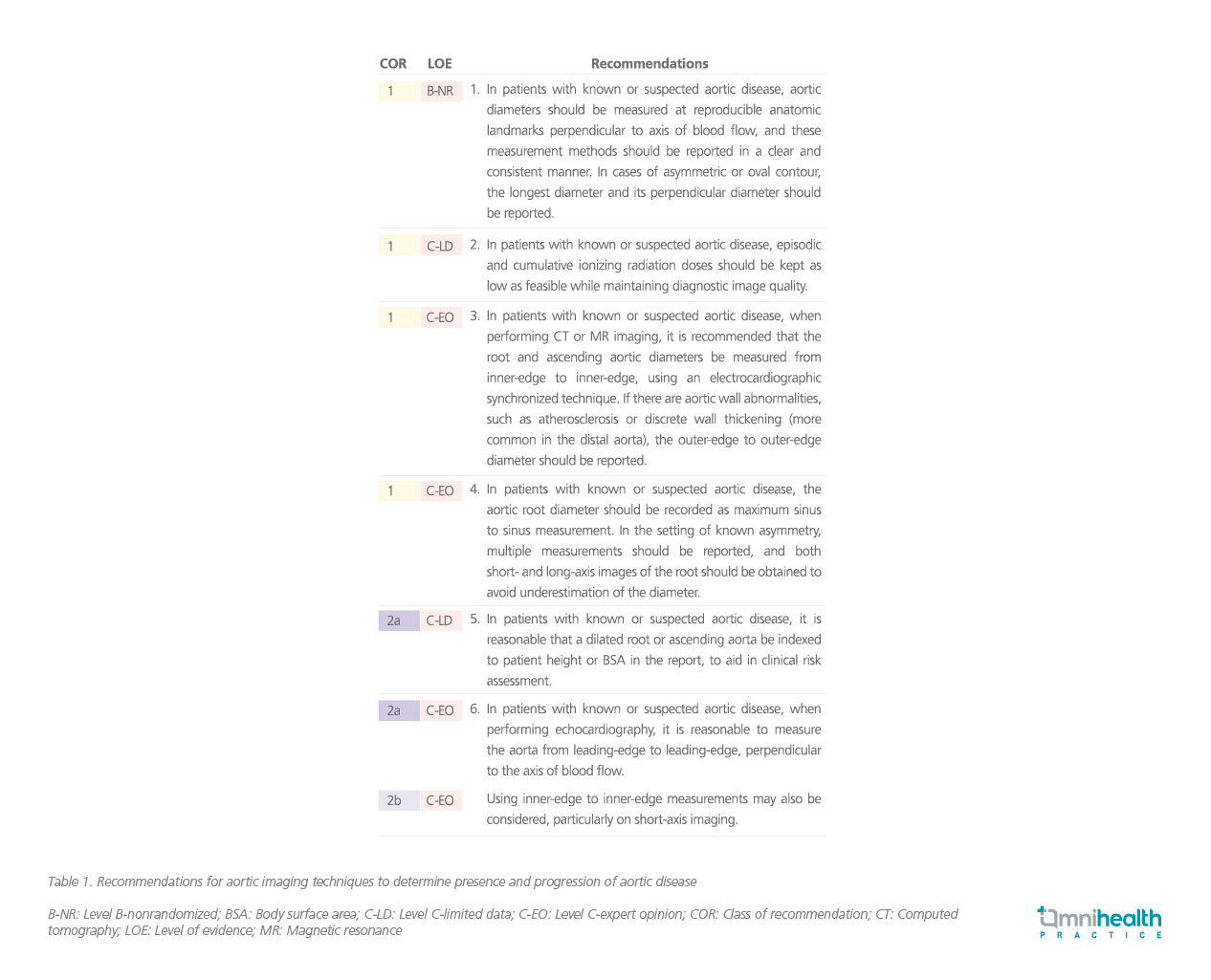
There were both single-center and multi-center studies comparing the outcomes of surgical aortic repair with or without a multidisciplinary aortic team (MAT), which have shown significantly lower mortality and better outcomes when surgeries were carried out by a sizeable multidisciplinary thoracic aortic surgery team.4,5
Relevant studies investigating the relationship between case volume and operative mortality were then presented. One study showed an inverse relationship between the volume of the aortic root and the ascending aortic surgeries performed in hospitals and surgical mortality.6 The expert writing committee noted that they were observing improved short- and long-term outcomes and mortality with the use of MATs, high-experience surgeons at high-volume centers.2 This led to the development of recommendations for the MAT management of aortic disorders (table 2).3