RESEARCH SPOTLIGHT
Overcome the flat dose-response of ssri with venlafaxine
In brief
This study provided evidence of the possible existence of a dose-response relationship with venlafaxine.
Background
Depression is a major contributor to disability, affecting 322 million people or 4.4% of the world’s population.1 Its prevalence has been increasing over the years by an estimated 18% between 2005 and 2015.1 The management of depression includes non-pharmacological options such as psychotherapy or pharmacological options, mainly the second-generation antidepressants such as first-line serotonin reuptake inhibitors (SSRIs).2 Since the current guidelines have conflicting recommendations, the dose dependency and optimal target dose of the second-generation agents remain controversial.2 While dose dependency among SSRIs is not found in the National Institute for Health and Care Excellence (NICE) guidelines, the American Psychiatric Association (APA) guidelines recommend gradual dose escalation as tolerated to reach the therapeutic dose.3,4 Systematic and comprehensive reviews addressing this issue are lacking or limited with disagreeing conclusions and little emphasis on the balance of efficacy, tolerability and the overall treatment acceptability.5-7
This meta-analysis was conducted to assess the dose-response of commonly prescribed antidepressants for the treatment of adults with major depression in terms of efficacy, tolerability and acceptability to provide summative evidence for future recommendations.2
Methodology
This study included double-blind, multinational, randomized controlled trials (RCTs), comparing the most frequently prescribed new-generation antidepressants in the United Kingdom (UK), involving 5 SSRIs (i.e., citalopram, escitalopram, fluoxetine, paroxetine, sertraline), venlafaxine and mirtazapine, with each other or with placebo in the management of major depression among adults.2,8 Trials were collected from different databases, national drug licensing agencies, the European Medicines Agency (EMA), trial registries, pharmaceutical companies, and other relevant organizations, including the NICE from the UK and Institut für Qualität und Wirtschaftlichkeit im Gesundheitswesen (IQWiG) from Germany.2 Trials comparing ≥2 fixed-dose treatment groups, including placebo with low risk of bias, were included.2 The outcomes assessed were treatment response (≥50% reduction on an observer-rated scale) for depression, preferably the Hamilton Depression Rating Scale (HAM-D) or the Montgomery-Åsberg Depression Rating Scale (MADRS), dropouts due to adverse events (AEs) to examine treatment tolerability, in addition to all-cause dropouts to examine the overall index of treatment acceptability.2
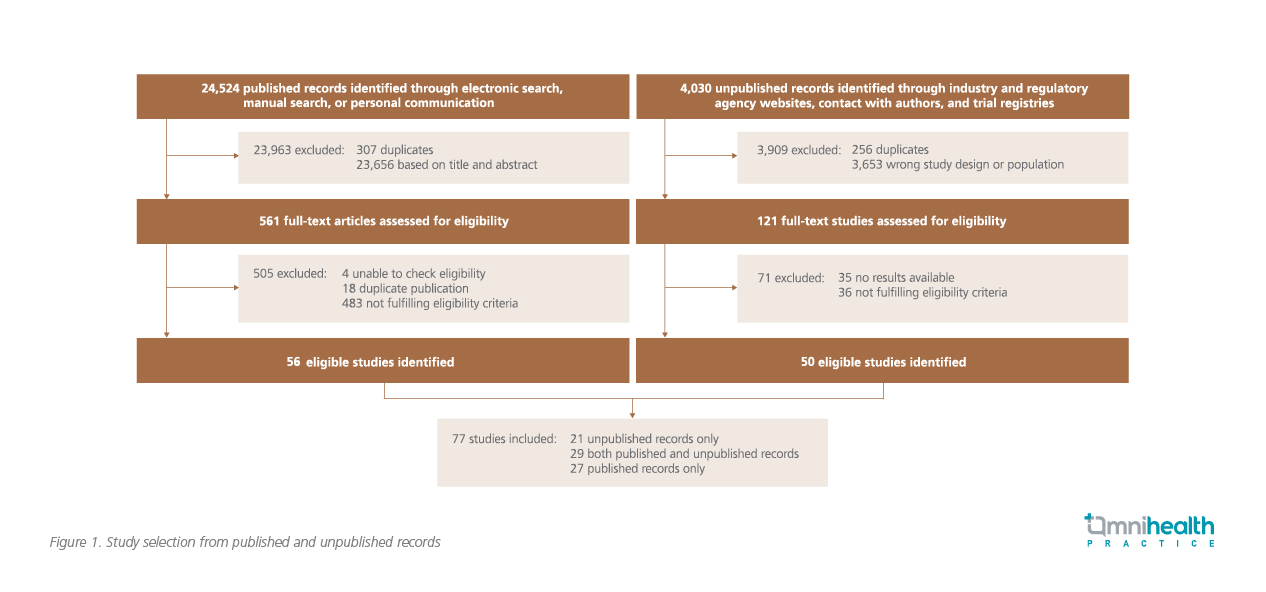
A total of 24,524 publications and 4,030 unpublished records were identified, of which 56 eligible publications and 121 eligible unpublished records were assessed for eligibility.2 After excluding studies that failed to meet the inclusion criteria, 77 studies including 21 unpublished records, 29 both published and unpublished records, and 27 publications were adopted in this meta-analysis (figure 1).2
Results and discussion
Treatment groups (n=201) in all the studies included placebo (n=75), citalopram (n=17), escitalopram (n=16), fluoxetine (n=27), mirtazapine (n=11), paroxetine (n=28), sertraline (n=11), and venlafaxine (n=16).2 Of the 19,364 patients included in all trials, 6,881 patients were allocated to placebo and 12,483 patients to the active drug.3 The mean age was 42.5 years, and 60.9% of patients were women.2
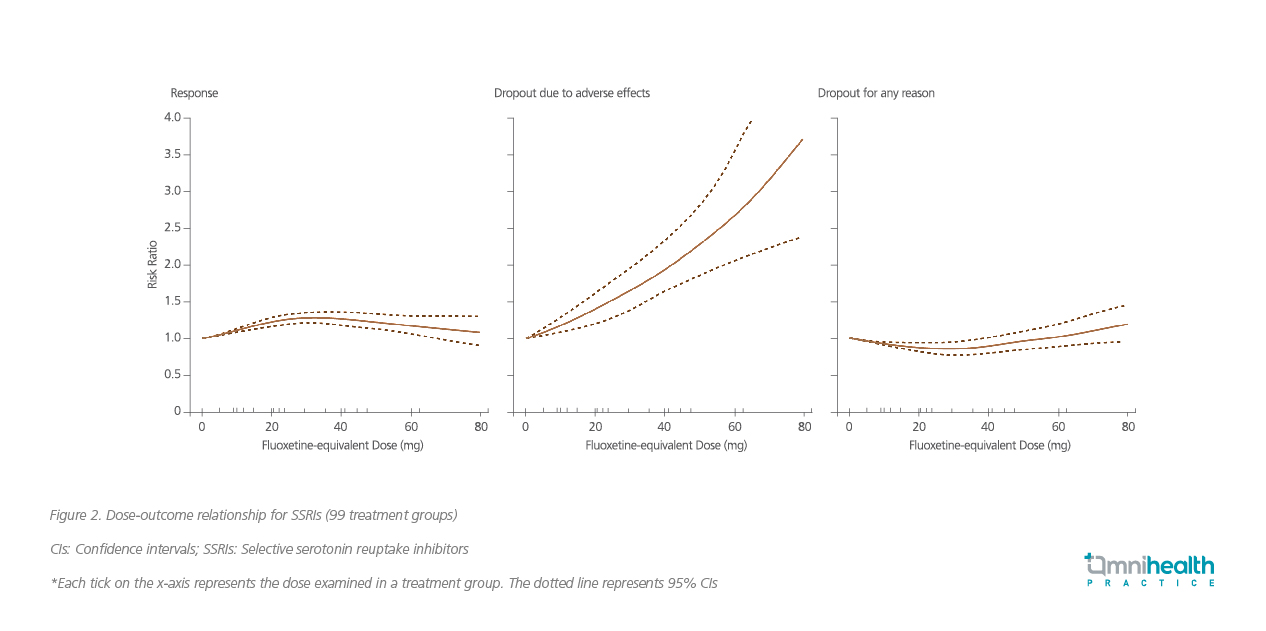
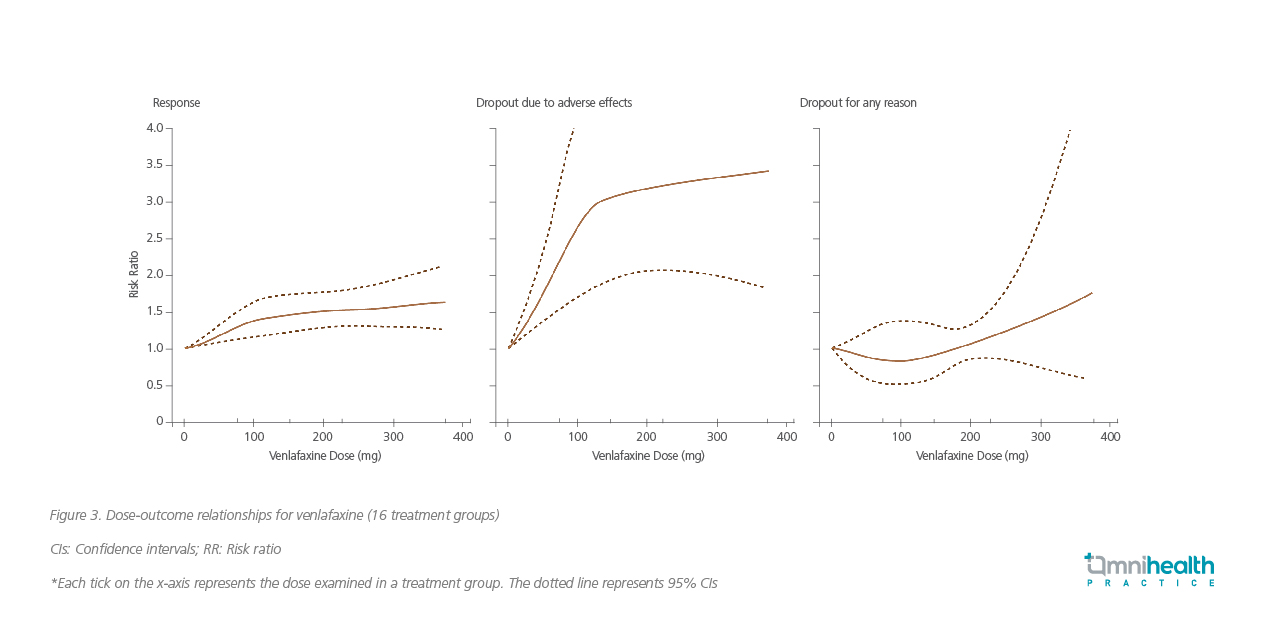
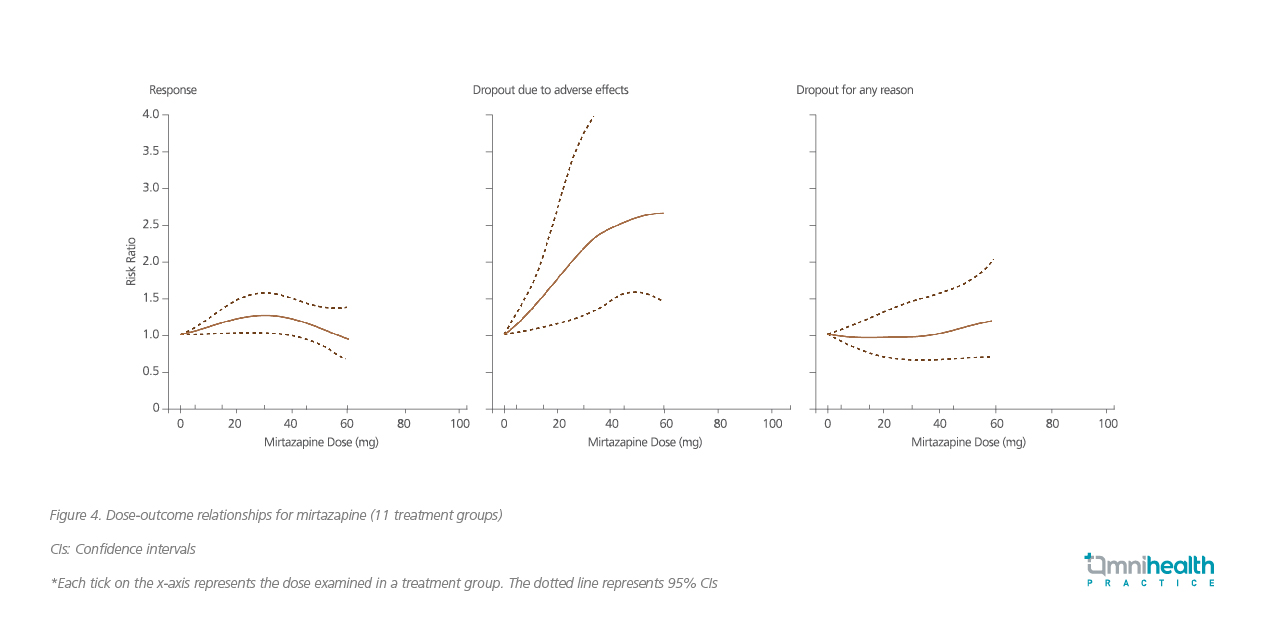
The response to SSRIs improved as the fluoxetine dose or the equivalent SSRI dose gradually increased from 10-30mg, after which it started to decrease (figure 2).2 However, the efficacy and response of venlafaxine increased sharply with higher doses up to 75-150mg, followed by a modest increase beyond this dose up to 375mg.2 Similarly, titration of venlafaxine to higher doses improved remission rates but also led to a proportional increase in dropouts due to AEs (figure 3).2 On the other hand, a higher efficacy was observed with increasing doses of mirtazapine up to a dose of 30mg, after which it decreased (figure 4).2
Professor Toshiaki A. Furukawa, Professor of the Department of Health Promotion and Human Behavior, Kyoto University Graduate School of Medicine and School of Public Health, Kyoto, Japan, the lead author of the study, concluded that for most patients receiving an SSRI, venlafaxine, or mirtazapine for the acute-phase treatment of their major depressive episode, the lower range of the licensed dose will probably achieve the optimal balance between efficacy, tolerability and acceptability.2
Significant interpretation
Prof. Furukawa mentioned that this study examined the dose dependency not only for efficacy but also for tolerability and acceptability, and was based on the largest and most comprehensive dataset of RCTs, analyzing not only SSRIs but 2 widely prescribed non-SSRI antidepressants as well.2 This analysis demonstrated a dose dependency in efficacy up to around 20-40mg fluoxetine equivalents, beyond which there was no further increase in efficacy for SSRIs or mirtazapine, but a possible increase for venlafaxine.2
These results showed that increasing serotonin transporter occupancy above 80% did not result in greater treatment efficacy, which supported the findings of another study stating that SSRI dose increase beyond this occupancy resulted in only small increases in transporter occupancy.9
Although high doses of SSRIs appeared to be slightly more effective in depression, they reached a plateau at an equivalent fluoxetine dose of 50mg.7 This slight benefit, however was offset by decreased tolerability.7 By using lower doses of SSRIs in clinical practice, clinicians would spare the patient of AEs by trading off a slightly reduced chance of improvement.5
On the other hand, venlafaxine, the serotonin and noradrenaline reuptake inhibitor (SNRI), might become apparent only at higher doses such as 225mg and 375mg.10 A study examining the dose-response relationship of venlafaxine demonstrated greater improvements in the total HAM-D and MADRS scores with the intermediate (225mg/day) and high doses (300-375mg/day) of venlafaxine.11
Generally, patients who do not achieve a response to SSRI after 8 weeks of treatment are switched to a non-SSRI drug.12 A 2005 review on the dose-response relationship of antidepressants showed that a flat dose-response curve may be seen within the SSRI class, but for SNRI, a dose increase strategy may be effective with venlafaxine due to sequential engagement of serotonin and noradrenaline reuptake inhibition according to the dose.12
In conclusion, SSRIs tend to have a flat dose-response relationship compared with mirtazapine (which shows a moderate dose-response relationship) and venlafaxine (which is associated with a significant dose-response relationship up to a dose of 375mg). Although doses at the lower approved range appear to have better effectiveness, venlafaxine may have better efficacy with increasing doses. These findings will have significant clinical implications, especially in the countries where practitioners often prescribe fluoxetine at doses of ≥40mg.2

