EXPERT INSIGHT
From conventional to leadless pacemaker: Real-world experience, challenges and future prospects
In recent years, leadless pacemaker has been introduced into clinical practice to overcome the lead- and pocket-related complications associated with conventional pacemakers, including infections and lead failure.1-4 In the absence of subcutaneous pocket and leads, leadless pacemaker is a promising technology that could potentially change the approach of arrhythmia management, particularly for patients with increased risks of infections.5,6 In an interview with Omnihealth Practice, Dr. Lee, Lai-Fun Kathy discussed the emerging role of leadless pacemakers in local practice and the ongoing challenges with the leadless pacing. She also shared a local clinical case to demonstrate the benefits of leadless pacemakers in a 95-year-old arrhythmia patient.
Safety concerns of conventional pacemaker
In Hong Kong, 1 in 100 people is affected by arrhythmia, with the risk of disease increasing with age.7 While atrial fibrillation (AF) is the most common type of arrhythmia, it is generally not immediately life-threatening. However, the risks of stroke, heart failure and mortality in arrhythmia patients are about 5, 3 and 2 times higher than people without arrhythmia, respectively.7 Hence, pacemaker implant is an effective option for symptomatic arrhythmia patients and has been widely adopted in clinical practice for the AF management with a current rate of 1 million devices per year, globally.7,8
In general, conventional pacemakers carry a subcutaneous pocket and leads (e.g., permanent transvenous pacemakers). Studies have shown that these pacemakers were associated with an approximately 7%-12% increased risk of major complications at 3 months after implantation, with nearly half of them attributed to lead dislodgement, lead fractures and infections.1,8 In particular, infections relating to pulse-generator pocket have aroused much concern about the long-term safety of conventional pacemakers, since it has been shown to be associated with significantly increased morbidity and mortality in patients who have received the implants.1,5
Leadless cardiac pacing for the arrhythmia management
Leadless cardiac pacing is a new form of pacing technology, which aims to eliminate pocket- and lead-related complications.5 Without the leads, the leadless pacemaker has an unique feature of being fully contained in the right ventricle, providing right ventricular sensing or pacing.8,9 To date, there is 1 leadless pacemaker that has obtained the United States (US) Food and Drug Administration (FDA) approval for treating arrhythmia.2 The approval was based on the positive trial results, in which 98% of eligible patients had achieved adequate pacing capture thresholds at 6-month post-implant, along with significantly fewer major complications than those with transvenous pacemakers.2,9
To further evaluate the safety and efficacy of leadless pacemakers, a systematic review and a meta-analysis have been recently conducted, covering 36 high-quality studies of leadless pacemakers published as of June 6, 2020.1 The primary safety endpoint was the incidence of any major complications, while the primary efficacy endpoint was good electrical performance as indicated by an acceptable pacing capture threshold of ≤2V.1 For patients with leadless pacemaker implanted, the incidence of complications at 90 days (n=1,608) was 0.46% (95% CI: 0.08-1.05), and at 1 year (n=3,194) was 1.77% (95% CI: 0.76-3.07) after implantation.1 In those studies of up to 1-year follow-up, much lower odds of complications were found with leadless pacemaker vs. conventional transvenous pacemaker (OR=0.49; 95% CI: 0.34-0.70).1 Of note, the common complications with transvenous pacemakers, including device dislodgement, tamponade/cardiac perforation, and infections, were not found in patients with leadless pacemakers (n=2,376).1 Regarding the pacing capture thresholds in the first year, 98.96% (95% CI: 97.26-99.94) of patients (n=1,376) implanted with leadless pacemaker had adequate threshold values.1
Based on the compelling evidence, Dr. Lee adopted leadless pacemakers for treating her arrhythmia patients. She also shared a local clinical case to demonstrate the clinical benefits of leadless pacemaker implantation in an older patient with bradycardia and discussed the importance of rate adaptive algorithm adjustment in leadless pacemaker, as well as the unsolved issues with leadless pacing.
Clinical experience of using leadless pacemaker
A 95-year-old female dementia patient was diagnosed with symptomatic bradycardia. After a thorough assessment, cardiac pacemaker implantation was deemed an appropriate option to restore her normal heart rhythm. Since the patient’s family was concerned about the infection risk of conventional pacemakers and the post-implant wound care, Dr. Lee considered leadless pacemaker as a better option for this patient.
The leadless pacemaker implantation was performed successfully via the femoral vein transcatheter approach, where a very small incision of only approximately 1cm was made on the patient’s groin. The leadless pacemaker functioned properly after implantation and successfully restored the patient’s heartbeat from less than 40 beats/min to a normal rhythm. The patient was then followed up a week after the surgery, and no procedure- or pacemaker-related adverse events (AEs) and complications were observed. During the follow-up at 1 month and 3 months, the patient maintained a stable heart rate and blood pressure and no longer complained of any bradycardia-associated symptoms. As such, calibration or program adjustment of the leadless pacemaker was considered unnecessary. Subsequent follow-up was arranged every 6 months until the patient died at 99 years of natural causes, unrelated to the pacemaker. During the 4 years of implantation, no AE associated with the leadless pacemaker was reported.
Dr. Lee mentioned an additional benefit of the leadless pacemakers, “Usually, when patients implanted with conventional pacemakers pass away, their family members need to rush to the hospitals for removing the implanted pacemaker as pacemakers with leads can cause explosion during cremation. With leadless pacemakers, they no longer need to bother.”
Optimizing rate response in sedentary patients
For leadless pacemakers, 3-axis intracardiac accelerometer is deployed for rate adaptation, and 3 sensor setpoints [i.e., lower rate (LR), activity of daily living rate (ADLR) and upper rate (UR)] are used to convert detected acceleration to a desired rate response.10 With the adoption of more sensitive accelerometer counts (AC) setting for the 3 setpoints and the automatic rate profile optimization (RPO) algorithm in leadless pacemakers, the same AC that occurs at rest or exercise may give rise to a higher rate response in patients with sedentary activity daily living (ADL).10 This phenomenon occurred in one of Dr. Lee's sedentary ADL patients during follow-up, with the patient’s pacing rate fluctuating even when she made small movements, such as turning the body around (figure 1).10 Dr. Lee explained that this fluctuation phenomenon was due to the increasingly sensitive rate adaptive settings in the leadless pacemaker, thus producing a more aggressive rate response by the automatic RPO.10
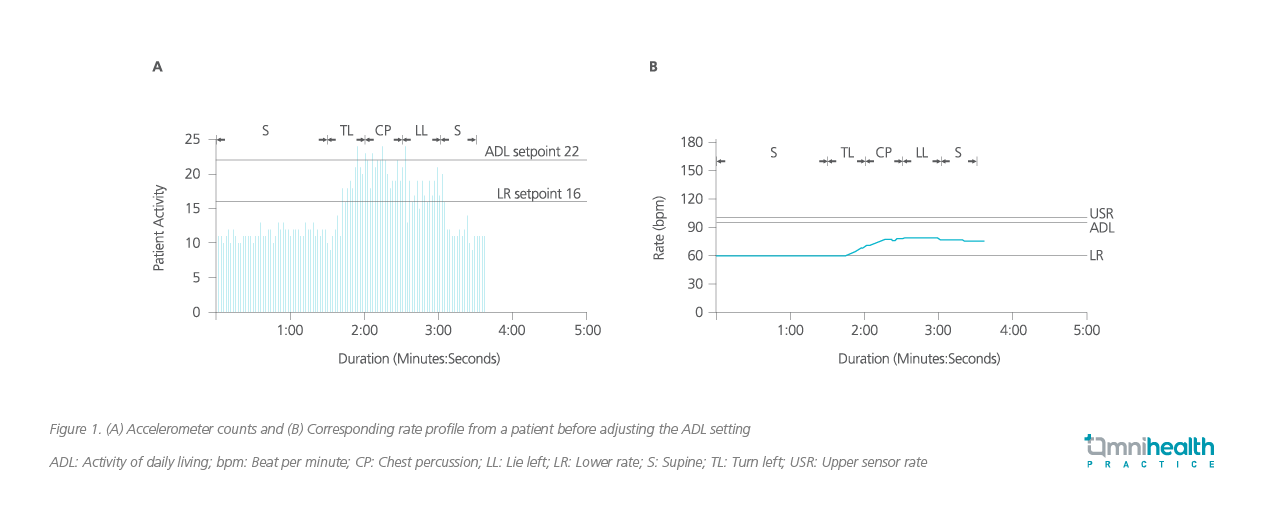
Dr. Lee was among the first to recognize this phenomenon which could occur in patients who resume exercise after a long period of sedentary life.10 To address this issue, Dr. Lee suggested choosing a sensor vector axis that is less sensitive to body turning, deactivating the RPO algorithm, and reprogramming the ADLR appropriately.10
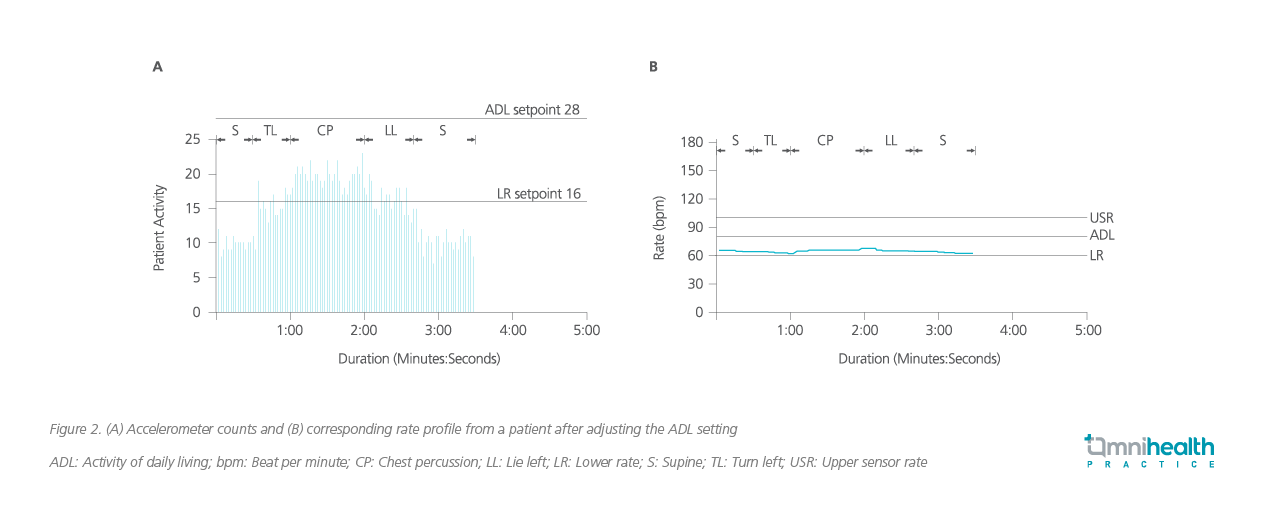
In that patient, Dr. Lee increased the ADLR setting from 22 to 28.10 This adjustment allowed only minor rate changes during turning and chest percussion, while permitting rate adaption during assisted walking (figure 2).10 “In sedentary patients, it is essential to make appropriate changes of LR, ADLR and UR setpoints in leadless pacemakers, thus providing an optimized rate response from the RPO algorithm,” Dr. Lee stressed.
Future prospect of leadless pacemakers
Despite the advantages of reducing the risks of complications associated with the conventional pacemakers, a wider adoption of leadless pacing therapy is limited by its single-chamber pacing indication, i.e., leadless pacemakers are not indicated for other clinical conditions that require dual-chamber pacing.8 To address this issue, a multicenter, international, single-arm, pivotal investigational study has been initiated in early 2022.11 This ongoing trial evaluates the clinical safety and effectiveness of a leadless dual-chamber pacemaker system in a patient population of 550 indicated for dual-chamber bradycardia pacing.11 This novel system is designed for atrial sensing and pacing, atrioventricular (AV)-synchrony, and ventricular sensing and pacing.8 If the trial is successful, the novel dual leadless pacing system would benefit an even broader range of patients with arrhythmia.8
Besides, battery longevity is another considerable limitation of leadless pacemaker. Extensive studies on battery longevity are also indispensable to support the wider adoption of leadless pacing technology in clinical practice.8
Conclusion
Leadless pacemaker is a ground-breaking technology that has started a new era of cardiac pacing by mitigating the risks of pocket- and lead-related complications of conventional pacemakers. Dr. Lee adopted leadless pacemakers to treat her arrhythmia patients and emphasized the importance of optimized rate response with leadless pacemakers. While the wider adoption of leadless pacing is limited by single-chamber ventricular pacing and battery longevity, researchers have been endeavoring to evaluate the feasibility of leadless dual-chamber pacemaker system among patients in need of dual-chamber pacing, as well as expanding the battery longevity of leadless pacemakers.

