EXPERT INSIGHT
CD management: advances and ongoing difficultiesin local practice
In 2016, a young woman in her 20s complained of sudden abdominal pain in the morning which then deteriorated rapidly, and was subsequently admitted to the intensive care unit (ICU) of Prince of Wales Hospital (PWH). The patient was diagnosed with Crohn’s disease (CD). During her ICU stay, the patient underwent 2 major surgical procedures and received massive blood transfusion due to her severe intestinal bleeding. The patient had been staying in the ICU for 3 months and was discharged from PWH only about 3 years later. This case reminds us of the considerable suffering of the CD patients and the immense challenges of overall disease management. Considering its rising prevalence in Hong Kong, CD is set to increase the medical needs of patients and the disease burden of the society.1 In an interview with Omnihealth Practice, Dr. Lam, Long-Yan Kelvin talked about the latest advances in CD management and the ongoing difficulties in local clinical practice.
Background
CD, a disease first described by Dr. Burrill B. Crohn and his colleagues early in 1932, belongs to the spectrum of idiopathic inflammatory bowel disease (IBD), and is characterized by discontinuous skin lesions and transmural inflammation, which may involve the entire gastrointestinal (GI) tract from the mouth to the anus.² CD patients can develop complications, such as intestinal fistula, perforation, obstruction, and ulcerative colitis with neoplasm of the colon, therefore resulting in elevated risks of morbidities and mortality.3
An observational study from a territory-wide, population-based registry found that the prevalence of CD in Hong Kong has been on the rise.¹ Over the past 3 decades, the incidence rate has increased tremendously from 0.05 per 100,000 individuals in 1985-1989 to 14.17 per 100,000 individuals in 2011-2014, pointing to the increasing medical needs of patients and the disease burden of the society.1
Multiple risk factors identified in CD
Despite the fact that the causes of CD remain unknown, several risk factors have been identified to be associated with increased risks of CD development, including gender and genetics, etc.4 In general, the incidence of CD among men is higher when compared with women.3 Patients who carry heterogenous Nucleotide-binding oligomerization domain-containing protein 2/ caspase recruitment domain-containing protein 15 (NOD2/CARD15) genes and homogenous alleles have 2-4 times and 20- to 40-fold increased risks of developing CD, respectively.4
Fortunately, some risk factors of CD are modifiable.4 Past history of smoking (including active and passive smoking), lack of long-term dietary fiber intake, consistent disruption of sleep, and insufficient exercise have been linked to higher risks of CD.4 Modifying these risk factors might, therefore, help lower the likelihood of CD occurrence/ recurrence.
Additional risk factors of CD include the time of disease onset and the presence of perianal fistulas at disease presentation.5,6 In general, CD mainly has 2 peaks of disease onset, with the first between 20 to 30 years of age and the second at around 50 years old.2 Several studies have revealed that CD patients with early disease onset tended to have a more severe disease and required more aggressive treatments.5 On the other hand, a study from the United States found that Asians had more perianal involvement than the Caucasian counterparts.7 Patients with perianal CD were more likely to receive abdominal surgeries.6
Current prognostic scoring system in CD and its limitations
The Crohn’s Disease Activity Index (CDAI) is a well-established prognostic system that defines the severity of disease activity among CD patients.8 First published in 1979, the CDAI was used to compare the results of patients treated with sulfasalazine, prednisone, or azathioprine with those of the placebo group.8 Although the CDAI first appeared to be relatively reliable, significant inter-observer differences were noted in the later studies.8 As such, in local clinical practice, disease prognosis is still determined via simple prognostic factors, especially gender, the time of disease onset, the presence of lesions and abscess under endoscopy.
The current principles for CD management
CD is a lifelong disease that still cannot be cured.4,9 The current management approach aims to achieve symptomatic relief, induce remission in the short term, as well as prevent relapses and complications in the long term.9 Since evidence has shown that patients with chronic and insufficiently treated underlying inflammation (even if the patients are asymptomatic) are more likely to develop CD-associated complications, it is nowadays recognized that early pharmacological intervention is critical.9 In local clinical practice, a “top-down” approach with timely and intensive treatment has been widely adopted to achieve rapid disease control in CD patients.
The current treatments for inducing remission
Corticosteroids are among the most efficacious drugs for inducing remission in the short term, while thiopurine monotherapy is not effective in inducing remission since it has a much slower onset of action of around 8-12 weeks.9 Among moderate-to-severe CD patients who fail to respond to the conventional therapies, or patients who present with fistula, more aggressive approach using monoclonal antibodies, including tissue necrosis factor (TNF) inhibitors (e.g., infliximab and adalimumab), interleukin-12/23 (IL-12/23) inhibitors (e.g., ustekinumab) and α4β7 integrin (LAMP-1) inhibitor (i.e., vedolizumab), should be adopted.9 All these biological agents are equally effective in inducing remission for CD patients, regardless of their prior biological exposures.9 In general, TNF inhibitors are the first-choice treatment options.9 Of note, the addition of thiopurines to infliximab induction therapy has been shown to be more effective among treatment-naïve patients vs. infliximab alone; no such additional clinical benefit was observed for adalimumab in the clinical trial.9
Therapies for the prevention of relapses
Thus far, immunosuppressants (e.g., thiopurines and methotrexate) and biological agents are the most effective therapies in maintaining medically induced remission among patients with moderate-tosevere CD.9 In particular, thiopurines or methotrexate is often utilized to maintain remission in steroid-dependent patients; while for patients where remission has been achieved by a biological agent, the same biological agent is usually used for preventing future relapses.9
Mucosal healing for preventing complications
Prevention of CD-associated complications remains a major treatment goal for CD patients, since they are often associated with significantly increased morbidities and mortality.10 In the past, there was no evidence showing the efficacy of conventional drugs in these regards.11 More recently, mucosal healing (i.e., endoscopic remission) has been shown to be associated with higher rate of sustained clinical remission, as well as lower rates of hospitalization and disease-related surgeries (i.e., better disease control and fewer complications).11 Since then, the clinical trials of newer biological agents have focused on mucosal healing as a vital treatment target for CD patients.10
Study of Biologic and Immunomodulator Naive Patients in Crohn’s Disease (SONIC) was the first trial to adopt mucosal healing as a key study endpoint.10 Results showed that about 44% of patients with active CD who were naïve to TNF inhibitors achieved endoscopic remission with the combination of infliximab and azathioprine after the 26-week treatment.11 Subsequently, some other biological agents were also shown to attain similarly remarkable outcomes in mucosal healing among CD patients.11
Novel potential agents in CD management
Despite the use of biological agents, many patients still have refractory diseases, and surgery remains frequent among CD patients, probably due to the development of neutralizing antibodies over time.12 The high surgery rates indicate an urgent need for further expanding the armamentarium in CD management. Since cytokine signaling plays a crucial role in the CD pathogenesis, Janus kinase (JAK) inhibitors were therefore considered in the CD-related clinical trials.12,13 JAK inhibitors are small molecule drugs that can be conveniently administered orally.13 Also, JAK inhibitors have a rapid onset of action and do not elicit antidrug antibodies, rendering them an ideal candidate as an alternative for patients whose diseases remain refractory to biological agents, or in whom biological agents are contraindicated.13
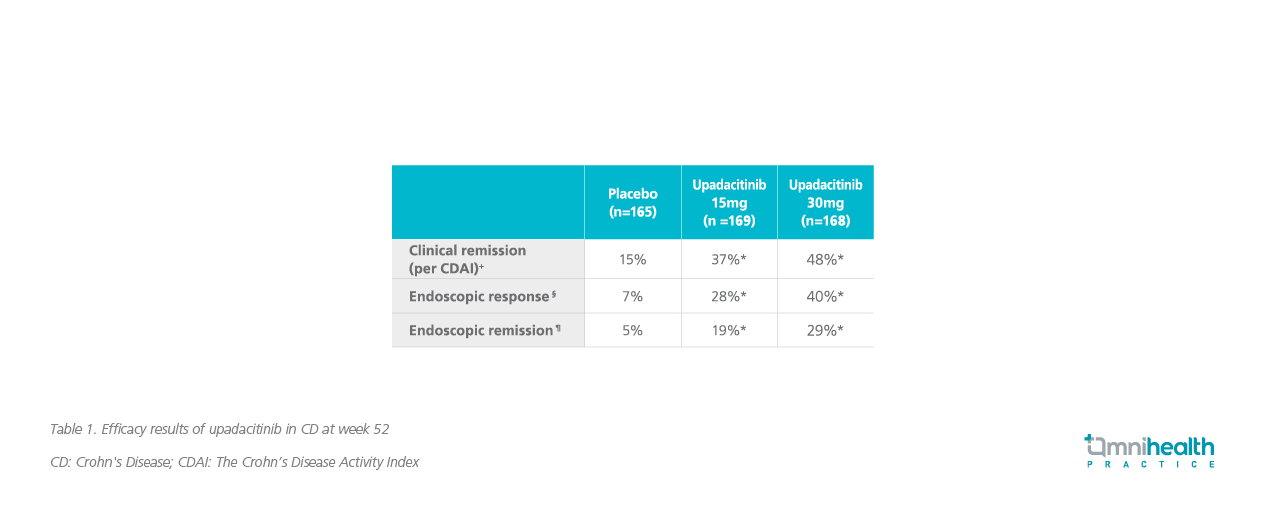
Encouragingly, upadacitinib, one of the three JAK inhibitors available in Hong Kong, demonstrated promising results in a phase 2 trial in moderate-to-severe CD, and therefore, a phase 3 study was initiated.12 The positive findings of the phase 3 study were announced in May 2022. Results found that a significantly higher proportion of patients treated with upadacitinib 30mg achieved clinical remission at week 52 vs. placebo (48% vs. 15%; p<0.0001) (table 1).14 Moreover, about 29% of patients in the upadacitinib 30mg group achieved endoscopic remission (i.e., mucosal healing) vs. 5% in the placebo group (p<0.0001).14 The safety results of upadacitinib in CD patients were consistent with the established safety profile of upadacitinib, and no new safety signals or deaths were reported.14
The promising findings could be particularly important for CD patients whose medical needs remain unmet with the conventional treatments or biological agents. Yet, further regular review is needed before upadacitinib can be fully used in local clinical practice.
Treatment monitoring and ongoing challenges in local practice
In CD, underlying inflammation of the bowel and disease progression, which are associated with increased risks of complications and the need for surgical procedures, often precede the reporting of clinical symptoms by patients. Hence, the international guidelines strongly recommend regular monitoring of the disease and treatments based on the objective and measurable markers, e.g., endoscopy, C-reactive protein (CRP), calprotectin, etc.9 This approach could allow physicians to achieve stringent control of CD and prevent the development of complications.14
“However, our disease surveillance is far from enough and cannot keep up with the recommendations of the international guidelines,” Dr. Lam said reluctantly. After all, endoscopy is a costly procedure for many patients, rendering it not feasible to perform too often. “Sadly, if we wait until patients present with symptoms, it is already too late. In fact, these are the ongoing dilemma and difficulties facing us and our patients,” Dr. Lam added.
Conclusion
All in all, the prevalence of CD in Hong Kong has been increasing over the past 3 decades, and it is imperative to increase the disease awareness among healthcare professionals and to stay vigilant. The management of CD could be very challenging, and the disease, if not well controlled, would bring considerable suffering to patients. Since 2016, there have been some advances in the CD management in terms of additional treatment options. Still, stringent treatment monitoring is needed to achieve optimal disease control (e.g., mucosal healing) and prevent complications. While this remains an unaddressed issue in local practice, more efforts are required to improve the CD management in Hong Kong and help patients resume their normal lives.

