EXPERT INSIGHT
Experience learning from the first MSC unit in HK
With the median age of women having their first child in Hong Kong (HK) rising from 28.1 years in 1991 to 32.3 years in 2020, the rates of comorbidities and obstetric complications are expected to increase.1-4 Thus, notably, there is an increasing need for maternal critical care, resulting in the first HK maternal special care (MSC) unit being piloted in the Prince of Wales Hospital in May 2018 which aims to reduce maternal morbidity and mortality. In an interview with Omnihealth Practice, Dr. Hui, Shuk-Yi Annie talked about her experience in founding the first MSC unit in HK and shared a clinical case of preeclampsia with postpartum hemorrhage which benefited from the MSC unit and resolved without developing complications
Noting the unmet need in maternity critical care
In HK, the age of first-time mothers has been rising.1 This is of great concern as advanced maternal age is associated with higher rates of coexisting medical diseases and obstetric complications.2-4 According to the World Health Organization (WHO), the top 3 causes of maternal deaths are obstetric hemorrhage, sepsis and hypertensive disorders, summing up to around 50% of all maternal mortalities.5 Based on data of the intensive care unit (ICU) admissions of obstetric patients and maternal mortalities from the Hospital Authority (HA), the composition of maternal deaths in HK is similar.6
The management of these deadly obstetric conditions often requires life-saving procedures and maternal intensive care.6 In fact, maternity critical care has been implemented in countries such as the United Kingdom (UK) and the United States (US) for years, but yet in HK.6 It is understandable that there exists an intrinsic difference in the healthcare systems between the western countries and HK. However, with the rising age of first-time mothers, maternal critical care is now well recognized as an indispensable service for reducing maternal morbidity and mortality.6
The journey of founding the first MSC unit in HK
Before setting up MSC, hospitals in HK handled high-risk mothers differently. Some admitted the patients to the ICU which often had limited beds, whereas others managed them at general maternity wards where high-risk patients may be treated insufficiently, increasing the odds of developing serious complications and death. In light of the service gap, the Hospital Authority adopted the idea of “maternal special care”, and the Prince of Wales Hospital was chosen as the first to establish an MSC unit, which was opened in May 2018.6 The MSC unit serves as an intermediary unit between the ICU and the general wards, on one hand it helps to reduce the number of admissions to the ICU and shorten the duration of ICU stay, on the other hand it provides higher level of care for mothers in need.6 Enhancing patient safety by ensuring intensive monitoring of high-risk cases, prompt recognition of deteriorating patients, early consultation to intensivists, and providing emergency care before transferring to the ICU are among the key objectives of the MSC unit.6 With a focus on providing optimal up-to-date management to a series of obstetrics conditions and complications, the MSC unit is managed by a multidisciplinary team of maternal and fetal medicine specialists, obstetricians, obstetric anesthetists, and midwives with critical care training.6 By situating the MSC unit within the delivery suite, mother-baby separation is also minimized.6
Vital features of the MSC unit enable high effectiveness
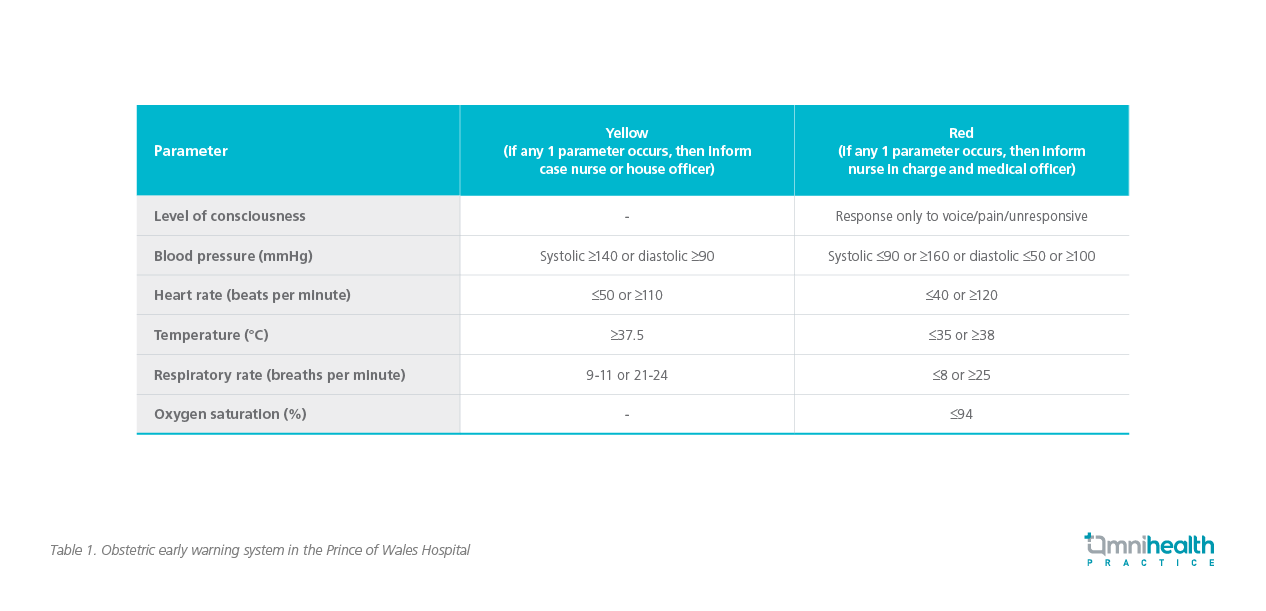
Obstetric early warning system
An early warning system to detect early symptoms and/or signs of maternal deterioration is an accurate tool to predict death among critically ill obstetric patients.6 The MSC unit took references from several different early warning systems and created its own for monitoring the altered physiological parameters of obstetric patients.6 A color-coded (yellow or red) observation chart is implemented to guide the escalation of care (table 1).6 The aim of the system is to raise clinical awareness of potential serious events and trigger urgent patient evaluation.6 This could ensure timely diagnosis and prompt intervention to reduce maternal morbidity and mortality.6
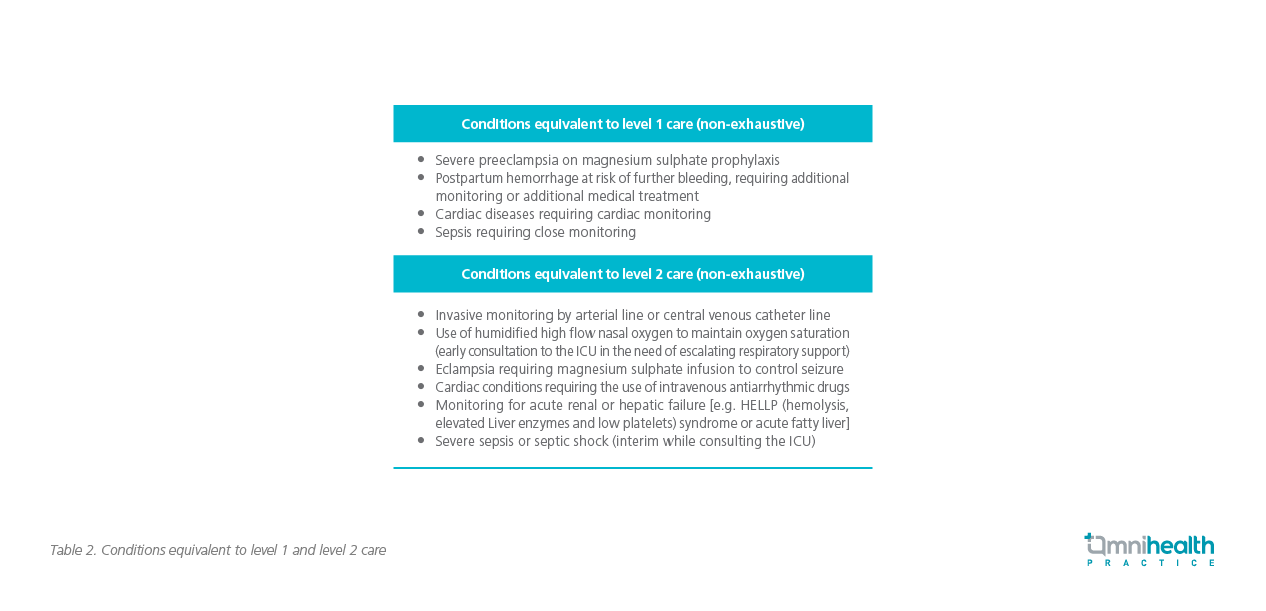
Two levels of care for critically ill obstetric patients
The MSC unit provides 2 levels of enhanced care, according to the patients’ conditions. Level 1 care is provided to patients at the risk of deterioration, who require enhanced monitoring or additional clinical interventions, clinical input or advice, and/or stepping down of care from a higher level, while level 2 care is given to patients with greater illness severity, at a higher risk of deterioration, or require closer monitoring (table 2).6 Certain patients, such as those requiring ≥2 organs support or advanced respiratory support, might necessitate an even higher level of care and would be transferred to the ICU.6 The MSC unit works closely with the ICU to ensure a smooth patient transferal if such need arises.6 The nurse to patient ratio in MSC unit is 1:1 or 1:2.
Equipment in the MSC unit
The humidified high-flow nasal cannula system, which is commonly used in the emergency department and the ICU, is available for respiratory support in the MSC unit (figure 1).6 To measure pH, partial pressure of oxygen, electrolytes and lactate, the MSC unit uses an in-house blood gas analyzer, which is particularly useful for cases such as severe sepsis since it has a short turnaround time.6 Another essential equipment is the thromboelastography (figure 2), which is used as the point-of-care coagulation test to identify any coagulopathy at an early stage of postpartum hemorrhage.6 Fibrinogen plays a major role in postpartum hemorrhage in obstetric patients and is an early predictor of coagulopathy, it is also an important factor in amniotic fluid embolism which is a life-threatening condition in pregnancy.6 This machine enables real-time assessment of fibrinogen and platelet functions, which could help alert the need of early intervention.6
Midwifery training in maternal critical care
As patients admitted to the MSC unit are taken care by midwives specialized in maternal critical care, a range of training is provided in order to enhance their competence.6 In-house training includes regular case reviews, drills, workshops and special equipment demonstrations.6 In addition, trainings organized by local institutions, such as the Institute of Advanced Nursing Studies and the Chinese University of Hong Kong, are also available.6 Overseas visits in 2018 and 2019 to hospitals in the UK and US were organized, with the aim of learning from their experiences in maternal critical care.6
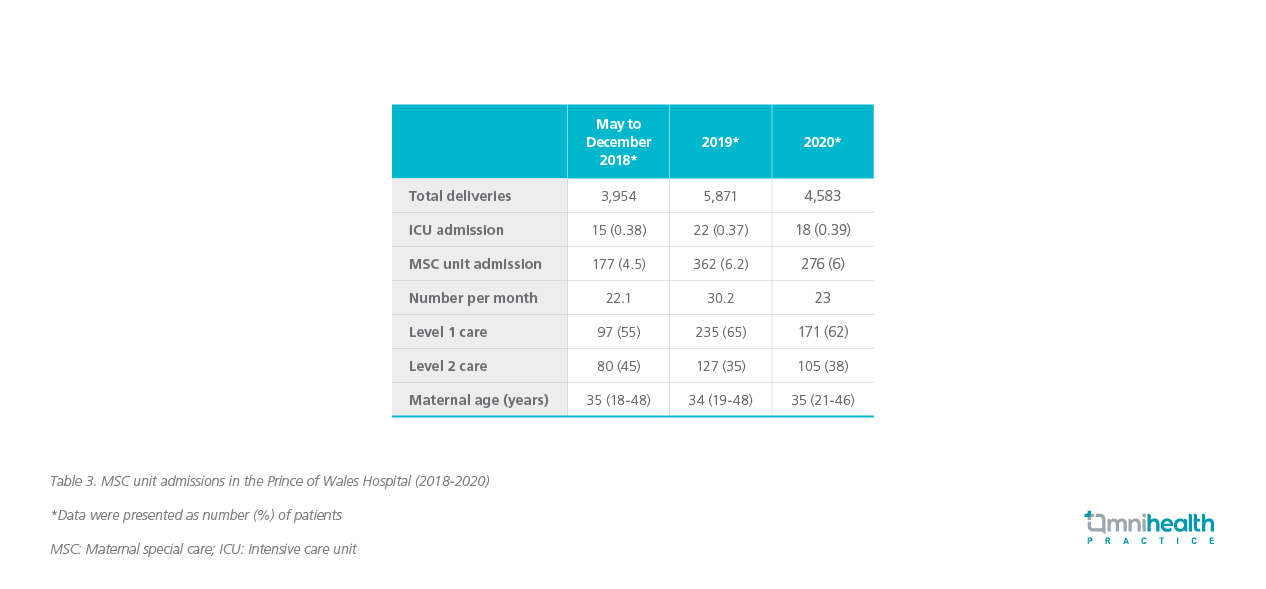
High utilization rate of the MSC unit showed high demand of maternal critical care
From May 2018 to December 2020, a total of 815 obstetric patients were admitted to the MSC unit (average 25 cases per month), accounting for 5.66% of the total deliveries (table 3).6 The mean length of stay in the MSC unit was 23.8 hours.6 Overall, 503 (61.7%) required level 1 care while 312 (38.3%) were given level 2 care.6 Of all patients admitted to the MSC unit, 55 women were transferred to the ICU or the cardiac care unit, accounting for 0.38% of the total deliveries.6 More than half of the patients (52.8%) were of advanced maternal age (≥35 years).6 The most common indications for MSC included preeclampsia/ eclampsia, massive hemorrhage and preterm labor before 32 weeks requiring magnesium sulphate infusion for neuroprotection.6
Operation of the MSC unit amid COVID-19
In 2020, the outbreak of coronavirus disease 2019 (COVID-19) had a striking impact on the operation of the MSC unit. Like many other hospitals, the obstetric team was divided into two teams: One to manage COVID-19-positive patients and the other for negative patients. The COVID pandemic spread the already limited manpower and resources even thinner, putting all public patients at risk.
Moreover, under the COVID-19 epidemic, more than half of the ICU beds were occupied by severely ill COVID-19-positive patients, resulting in even fewer beds available for high-risk obstetric patients. That arrangement left the MSC unit overwhelmed by the extra number of patients it needed to care for. More importantly, it highlighted the significance of the MSC unit since it could be served as a backup when the ICU was not available.
Dr. Hui stressed that one of key missions of the MSC unit was to reduce the risk of obstetric patients developing complications. Although the COVID-19 situation seems to have stabilized by now, she encouraged pregnant mothers to get vaccinated to protect themselves and their babies for possible future waves of epidemic.
Case sharing and discussion
With solid experience in operating the MSC unit, Dr. Hui shared a clinical case with obstetric complications to demonstrate the effectiveness of the MSC unit.
A female patient in her early 40s with no past medical problem had her first baby delivery at around 35 weeks of pregnancy. During her pregnancy, the patient was diagnosed with preeclampsia with severe features, and hence required emergency delivery by Caesarean section. She was admitted to the MSC unit to control her blood pressure before the operation. Unfortunately, during the Caesarean section, she also suffered from intraoperative massive hemorrhage that could not be controlled by medical means. As such, the massive transfusion protocol was activated. Thromboelastography was utilized to guide further clotting factors replacement. With the combined effort of the obstetricians and the anaesthetists, the bleeding was finally halted. In the era without MSC, this patient would need to be monitored in the ICU, for both her pre-eclampsia and postpartum hemorrhage would need very careful fluid management and chance of rebleeding is also very high. Our patient was transferred to the MSC unit after the operation, which provided her close monitoring via invasive lines, optimal blood pressure control and fluid management. After 24 hours of care by the MSC unit, the patient was finally stabilized and fit to be transferred to the postnatal ward. Overall, the management of this patient by the MSC unit was effective and satisfactory.
“The MSC unit allows healthcare professionals to monitor obstetric patients closely and provides early recognition and intervention, and thus prevents additional complications,” Dr. Hui commented.
Conclusion
The MSC unit serves as a good intermediary unit between the ICU and the general wards, effectively reducing maternal morbidity and preventing maternal mortality. Its high utilization rate unveiled the high demand of maternal critical care in HK and implied that a wider adoption of a similar service in other HK hospitals might be conducive to saving more lives of high-risk mothers.

