EXPERT INSIGHT
Ambulatory management of spontaneous pneumothorax: recent evidence and a case study
Spontaneous pneumothorax (SP) is defined as the existence of air in the pleural space without a precipitating external event.1 It can be further classified into either primary or secondary based on the presence or absence of pre-existing lung diseases.1 SP accounts for at least 1,000 hospital admissions per year in Hong Kong.2 Many patients with SP present to the emergency departments.2 Traditionally, considerations for intervention rest primarily on the size of pneumothorax and presence of dyspnea.1 There has been hardly any high-powered clinical studies on SP as the recruitment processes are remarkably difficult, given the emergency nature and acute presentation of many SP.3 Recently, the results of several practice-changing clinical trials on SP have been published, including new data on the ambulatory devices supporting its selective utilization in clinical practice.3,4 In an interview with Omnihealth Practice, Dr. Lui, Mei-Sze Macy presented some new data on the management of SP including the use of ambulatory devices and shared a case of secondary SP which resolved well without any complications after using one of such devices.
Starting with a simple, conservative approach
Chest tube drainage is the most common treatment for primary SP (PSP) in the real-life clinical setting.5 Despite its high efficacy in achieving radiological resolution, chest tube insertions were associated with complications such as pain, organ injury, bleeding and infection.5 Due to the potentially serious consequences of these invasive procedures, the British Thoracic Society (BTS) 2010 guidelines recommend that they should be reserved for patients with significant breathlessness associated with at least modest size of pneumothorax (≥2cm).1 For small PSP patients without significant breathlessness, a conservative approach should be adopted.1
More recently, a multicenter, randomized study has demonstrated that among patients with moderate-to-large PSP, conservative approach with observation was non-inferior to chest drainage in terms of lung re-expansion at the 8th week, with possible benefits in many secondary outcomes, including a lower risk of adverse events (AEs) and a shorter hospital stay.5 In this randomized trial, up to 85% of patients were spared from an invasive pleural intervention.5 The data provided a solid ground in support of conservative treatment for asymptomatic or minimally dyspnoeic patients with PSP, as long as close outpatient reassessment was feasible and adequate support was available when their symptoms deteriorated.5
Dr. Lui commented that “We have to determine when and how to intervene, and think about which approach (observation, simple aspiration, chest drain, or newer devices) provides the best outcome for our patients.”
Management of SP in Hong Kong
Local clinical practice continues to consider chest drain insertion as the mainstay of treatment for SP.2 Despite the recommendation by BTS guidelines, only 11% of patients with pneumothorax admitted to public hospitals were treated with conservative approach, i.e. simple aspiration.1,2 Apart from the increased risk of complications, invasive chest tube drainage can be associated with a longer hospital stay, reduced mobilization and jeopardized quality of life of patients with SP.5 Simple aspiration should worth more consideration as the initial intervention for evacuating pneumothorax, principally when the size of PSP is small and is not associated with significant breathlessness.1 A meta-analysis by the European Respiratory Society (ERS) taskforce on the management of SP in 2015 showed that although simple aspiration had a varying success rate of 50%-80%, it was associated with a much shorter hospitalization time and a similar recurrence rate at 3 months when compared with chest drain.6 For those whose SP persists or recurs on conservative management or post-aspiration, chest tube drainage can then be considered, in particular when dyspnea is also present.
Ambulatory devices: An alternative that allows ambulatory care and early mobilization
In the recent decade, ambulatory devices like Pleural Vent and Atrium Pneumostat have been explored as an alternative management for SP, aiming to shorten hospitalization, facilitate ambulatory care and improve quality of life.3,4 Pleural Vent consists of an 8-French pigtail catheter and a small plastic device with one-way valves attaching to skin that allow connection to wall suction, if required.4 Atrium Pneumostat is also a portable device that functions as an one-way valve and can be connected to chest tubes of a range of sizes for ambulatory drainage of pneumothorax.4
Efficacy of ambulatory devices demonstrated in patients with primary spontaneous pneumothorax
Chest drainage connected to traditional underwater seal system is associated with median length of hospital stay (LoS) of at least 6-8 days.3 According to an open-label, randomized controlled trial published in 2020, the use of ambulatory devices (i.e. Pleural Vent) greatly reduced the LoS.3 In this study, 236 adults with symptomatic primary SP were randomized 1:1 into standard of care (SoC) treatment or Pleural Vent management.3 The SoC arm had adhered to the BTS guidelines where aspiration was employed with optional smallbore chest drainage at the discretion of the physicians.3 Patients in the Pleural Vent arm were discharged soon after placement of the ambulatory device if they were clinically stable and mobile.3 The primary outcome of the study was to evaluate the total LoS, including readmissions within the first 30 days.3 Patients who had been discharged on the same day were recorded as having 0 day.3 It was shown that the use of ambulatory devices significantly reduced the median LoS from 4 days to 0 day (p<0.0001).3 In the meantime, the rate of AEs was reported to be higher with the ambulatory treatment group on account of home management.3 Below is a summary of the safety data from the trial (table 1):3
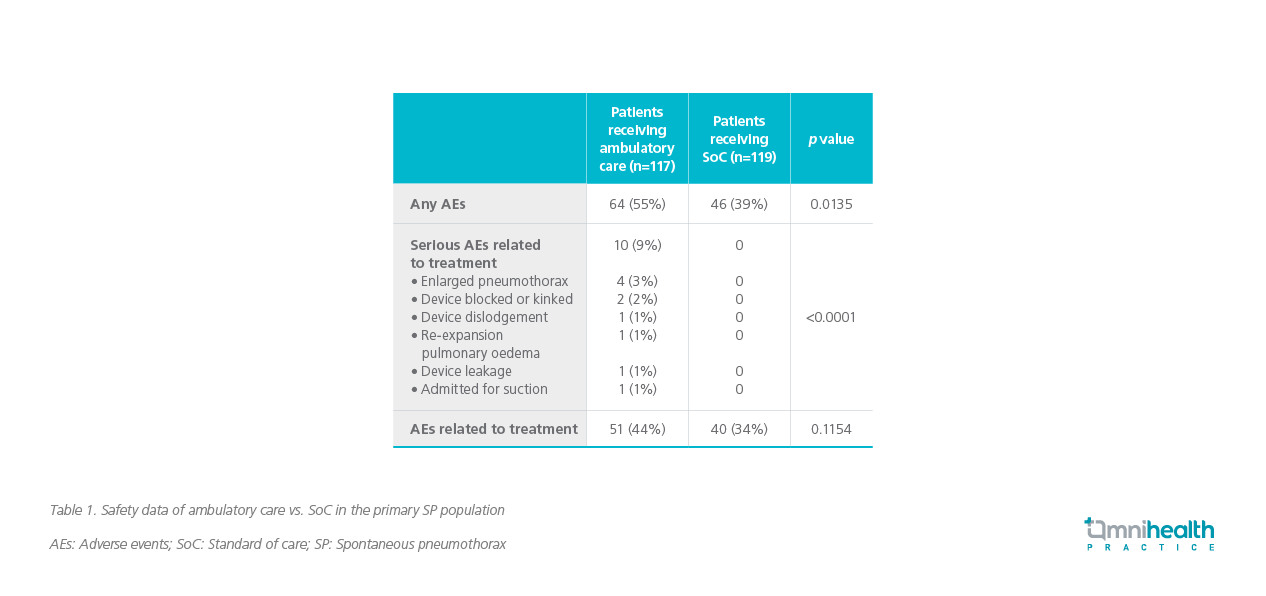
The role of ambulatory devices in secondary SP requires further investigations
The results in the population with secondary SP brought up uncertainties, which could be partially attributed to the poorer functional status and more significant air leak in patients with secondary SP.4 A recent multicenter, open-label, randomized controlled trial had assessed the use of 2 different ambulatory devices, Pleural Vent and Atrium Pneumostat, in the setting of secondary SP.4 The study was terminated early due to slower than expected recruitment.4 The data on the 41 recruited patients were analyzed.4 The median LoS did not show statistically significant difference in the ambulatory treatment arm compared with the SoC arm (figure 1).4
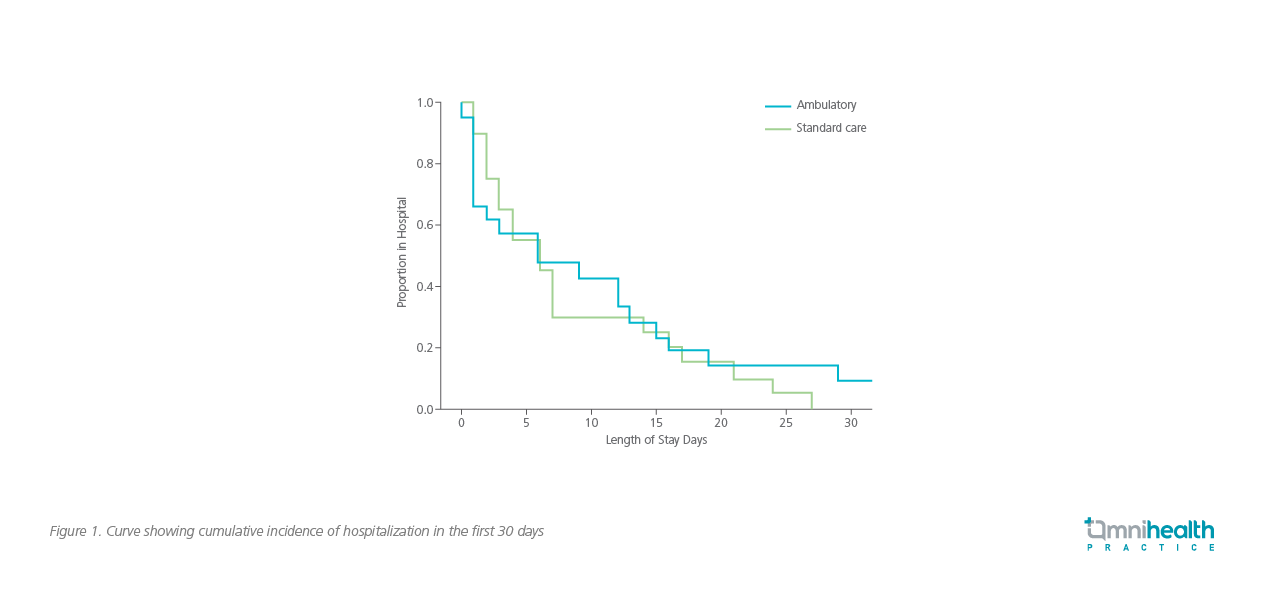
In this underpowered study, the use of ambulatory devices (n=21) was shown to have a median LoS of 6.0 days which was similar to that of the SoC arm (p=0.77).4 In a subgroup analysis of the ambulatory arm, the use of Atrium Pneumostat (n=8) was associated with a much shorter median LoS of 1.5 days compared with a median LoS of 9.0 days in the Pleural Vent subgroup (n=13).4 Given the smaller sample size in the subgroups, the difference was not statistically significant (p=0.37).4 There were no treatment failures associated with the use of Atrium Pneumostat, but there were 6 out of 13 failures in the subgroup treated with small-bore Pleural Vent.4
In this study, the small-bore (8 French) diameter of Pleural Vent was one possible reason that accounted for the high, early failure rate and failure to shorten hospital stay.4 The amount of air-leak, or in other words, the size and number of the visceral pleural hole(s), is often more sizable in secondary SP compared with primary SP.4 A chest tube of larger bore may be required in the context of secondary SP.4 On the other hand, Atrium Pneumostat allows connection to chest tubes of a range of sizes.4 Whether the use of Atrium Pneumostat is beneficial in stable secondary SP should be investigated further in clinical trials.4
Case sharing and discussion
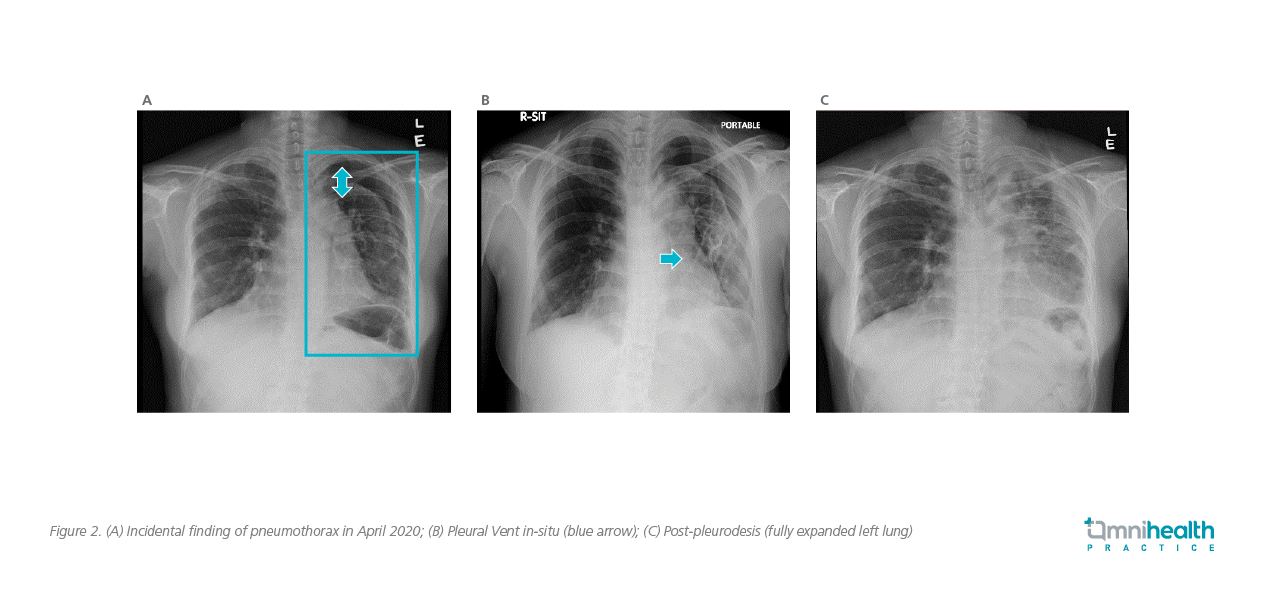
Dr. Lui shared a case to demonstrate the clinical effectiveness of ambulatory device in the management of selected patients with SP. A non-smoking female patient in her thirties had a past medical history of haematological malignancy and autologous stem cell transplant 10 years ago. She was diagnosed with pleuroparenchymal fibroelastosis 5 years after the transplant. In a follow-up visit, she was found to have a left sided apical pneumothorax (3cm from apex, figure 2A). Due to her underlying lung disease, a diagnosis of secondary SP was made. The patient did not experience any significant worsening in breathlessness and had a peripheral arterial oxygen saturation (SpO2) of 97% on room air. However, in view of her underlying chronic lung disease with fair lung function reserve, she was admitted to hospital for further monitoring.
Since the patient was minimally symptomatic, conservative management was adopted initially with supplementary oxygen. However, there was no radiological improvement after 3 days of conservative treatment. After thorough discussion, she was reluctant for placement of traditional larger-bore chest tubes. An 8-French Pleural Vent was then installed with a 5mm skin incision (figure 2B). She was kept in hospital for monitoring after the Pleural Vent was placed, which was connected intermittently to wall suction via the side port on the device. She was ambulatory in the ward with the Pleural Vent in-situ. The lung gradually re-expanded over the subsequent 5 days. Talc slurry pleurodesis was administered through the Pleural Vent upon full lung re-expansion, and the patient was discharged 12 days after installing the Pleural Vent (figure 2C).
Conclusion
The latest evidence from randomized clinical trials has advocated symptom-driven approach for primary SP, irrespective of the size of the pneumothorax.5 Invasive procedures, especially chest drainage, should be reserved for patients with persistent or recurring pneumothorax with breathlessness.5 Novel ambulatory devices, which have demonstrated efficacy in patients with primary SP, can be a viable alternative for reducing the need of more invasive interventions and shortening the duration of hospital stay.3 Although the use of ambulatory devices in patients with secondary SP requires further study, the treatment outcome of the case shared by Dr. Lui was promising, suggesting that it may be considered for highly selected subjects under close monitoring. The use of ambulatory device allows earlier ambulation and rehabilitation, which could be of paramount importance in improving the outcomes and preventing complications in patients hospitalized with secondary SP.4 All in all, with the wider adoption of evidence-based clinical practice, it is anticipated that the overall clinical outcomes of SP patients can be enhanced, thus significantly reducing the treatment complications and maintaining patients’ quality of life.

