MEETING HIGHLIGHT
Optimizing heavy menstrual bleeding treatment and management with LNG-IUS
The high prevalence of heavy menstrual bleeding (HMB) has affected 1 in 3 women of their lives. It can cause negative impacts on women’s physical, emotional, social, and health-related quality-of-life (QoL), thus becoming an economic burden.1,2,3 Furthermore, 50% of patients prefer to wait and seek treatments, leading to delayed treatment that may affect the medical outcomes.4 In Hong Kong, HMB patients are mainly offered stepwise, nonspecific conventional medical regimens, which may not be optimal and sufficient for the treatment of HMB. At a symposium organized by the Obstetrical and Gynecological Society of Hong Kong in 2020, Dr. Diana Mansour shared her insights about some modern approaches of diagnosing and management of HMB, as well as medical treatments for endometrial hyperplasia. She also highlighted the need for prompt HMB diagnosis among patients to improve their well-being and the importance of decision-making between both clinicians and patients according to the suggested treatment paradigm for HMB. Of note, Dr. Mansour discussed the use of levonorgestrel intrauterine system (LNG-IUS) as first-line treatment for HMB based on its demonstrated efficacy in reducing menstrual blood loss (MBL) and high acceptability and satisfaction from patients and physicians.
Definition and diagnostic criteria of HMB
According to the National Institute for Health and Care Excellence (NICE) guideline, HMB is defined as “the excessive menstrual blood loss (MBL) that interferes with a woman’s physical, social, emotional and /or material QoL. It can occur alone or in combination with other symptoms”.5 The NICE guideline focuses on improving the QoL by making informed decisions on ways to manage HMB.5 Dr. Mansour further highlighted the importance of avoiding complications, reducing length of hospital stays from surgery and minimizing healthcare costs and economic implications in the management of HMB.
In clinical practice, HMB can be identified by using 7 quick questions endorsed by the Society of Endometriosis and Uterine Disorders (SEUD).6 These questions look into changing of sanitary protection during the night and more than once every two hours on heavy days; experiencing excessively long and/or unpredictable periods; passing of large blood clots; feeling of lightheadedness or breathlessness during bleeding; worrying about bleeding-related accidents; and organizing social activities or planning for clothing around the bleeding.6
HMB continues to be poorly recognized and undertreated, substantially affecting quality of life
Despite the high prevalence and negative impact on women’s daily living, including work and sports performances, relationship with partners, and routine housework, HMB’s awareness and understanding amongst women are low.7 There is evidence suggesting that women with HMB symptoms do not seek medical help, and many women with HMB do not perceive heavy menstruation as a problem.8 In a large survey, it was found that approximately half the affected women never consulted a physician.8 Even for those who consulted a physician, almost half received no confirmation of HMB and a similar proportion was not offered medical treatment.8
Clinical consequences may also arise from HMB. It is recognized as the most common cause of iron deficiency anemia, warranting careful management and effective treatment to alleviate symptoms and improve QoL.2,8 Being unaware of the importance of managing iron deficiency can pose a negative impact on women’s QoL as it may take around 1 to 3 years to normalize the ferritin levels.
In Hong Kong, HMB patients are mainly offered conventional medical treatments in a stepwise and non-specific fashion that may be ineffective. A paradigm shift towards a personalized and effective treatment for HMB is therefore necessary and fundamental, particularly in providing sustained benefits to patients.
LNG-IUS as first-line option for HMB treatments
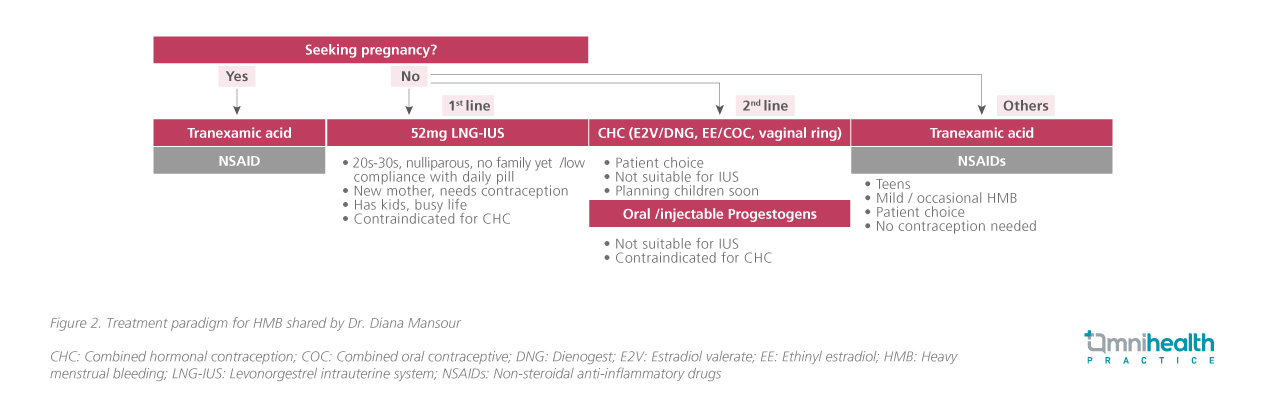
When deciding on HMB treatments, healthcare professionals should offer options that are not only effective in reducing bleeding, but also safe, tolerable and acceptable, in terms of treatment duration, compatibility with fertility and desire for future conception, as Dr. Mansour suggested.5 According to the NICE guideline, levonorgestrel intrauterine system (LNG-IUS) is recommended as first-line option for HMB, and other options may be considered when LNG-IUS is declined or is not suitable.5 Dr. Mansour added that combined hormonal methods may be the second option, and non-steroidal antifibrinolytics may be a useful option.
In a study of 20 women with HMB, LNG-IUS was inserted, and MBL was measured in 2 consecutive cycles before it was inserted, and after 3, 6 and 12 months of use.9 It was found that LNG-IUS significantly reduced MBL as early as 3 months after placement and sustained through 5 years (Figure 1).9 It was also shown that LNG-IUS was associated with significant increase in serum hemoglobin and ferritin.9
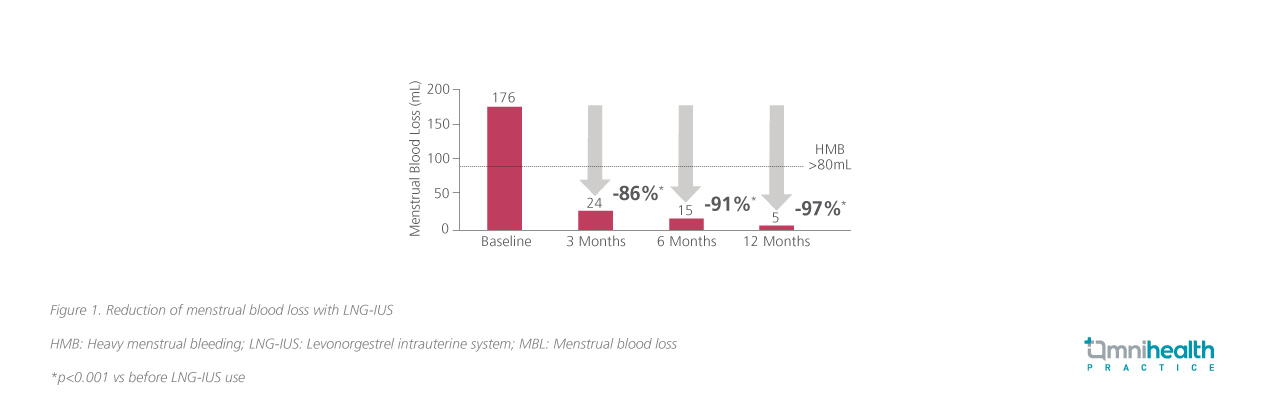
Similarly, when comparing with other treatment options like medroxyprogesterone acetate (MPA), flurbiprofen and tranexamic acid (TXA) and mefenamic acid (MFA), LNG-IUS significantly reduced MBL.10-12 It was also demonstrated to have a higher likelihood of treatment success than MPA and was the only treatment to reduce MBL to below 80mL per menstruation, suppressing and modulating cyclical endometrial build-up when compared with flurbiprofen and TXA.10,11
Advantages of adopting LNG-IUS over conventional medical and surgical treatments
In addition to the proven efficacy of LNG-IUS in HMB treatment, patient’s satisfaction with and acceptability of LNG-IUS, in combination with physician’s preference on LNG-IUS over other conventional medical treatments, makes LNG-IUS an alternative treatment choice. A prospective, observational cohort study using a non-interventional model investigated real-life treatment patterns and satisfaction in women using either LNG-IUS or conventional treatments, including hormonal treatment, antifibrinolytic treatment or a combination of both for HMB at 12 months.13 It was revealed that 83.5% of LNG-IUS users were very satisfied or satisfied as compared with 59.2% of conventional treatment users.13 Another prospective, non-interventional, observational cohort study comparing the cumulative continuation rate in the treatment of HMB with LNG-IUS and with conventional medical therapies showed that overall continuation was also significantly higher for LNG-IUS users than oral contraceptive pills, oral progestins and antifibrinolytics.14 On the other hand, a survey also showed that 80% of gynecological surgeons preferred LNG-IUS as first-line treatment as it is less invasive and associated with less potential morbidity than endometrial ablation or hysterectomy.15 As compared with other medical and surgical treatments like endometrial ablation and hysterectomy, LNG-IUS is also potentially less costly.15 The use of LNG-IUS resulted in the fewest hysterectomies, the most quality-adjusted life-year and the lowest cost among all nonsurgical strategies.15,16
Importance of counselling and selecting treatment based on patient profiles for long-term benefits with LNG-IUS
On top of the clinical benefits, high physician preference and patient satisfaction of LNG- IUS, counselling and educating patients is also essential in guiding treatment for HMB. As highlighted by Dr. Mansour, counselling and educating patients during their initial visit help explore treatment options, concerns, and expectations as well as rule out misconceptions about LNG- IUS.
When looking at the treatment options for HMB, Dr. Mansour discussed the following treatment protocols for HMB depending on patient profiles. Healthcare professionals should first consider if patients would like to get pregnant or not. Noncontraceptive medication like non-steroidal anti-inflammatory drugs (NSAIDs) and TXA should be offered to patients who plan to get pregnant. If patients are not considering getting pregnant at the moment, different options should be offered with LNG-IUS being the first choice. It is important that patients feel they have a shared decision-making when choosing the treatment plan (Figure 2).5
Dr. Mansour also reassured that nulliparity should not be a barrier when considering LNG-IUS treatment as fitting LNG-IUS in nulliparous women is simple and causes less complications as compared with parous women.17,18 It is also not associated with increased risk of pelvic infections or expulsion.18 It was demonstrated in a study that the use of LNG-IUS was reversible with a rapid return to fertility after removal as shown by normal conception rates. The endometrium was also shown to recover quickly, and cyclic ovarian function restored after the removal of LNG-IUS.19
LNG-IUS demonstrated significant regression of endometrial hyperplasia
Endometrial hyperplasia may be a cause of HMB. According to the NICE guideline, symptoms like intermenstrual bleeding, post-coital bleeding, pelvic pressure, and pain suggest that there might be an underlying endometrial pathology.5 Further investigation is required either with a transvaginal scan, or hysteroscopy, or both.5
Although, in certain circumstance, endometrial hyperplasia may regress spontaneously, it may also progress to endometrial carcinoma.20 Dr. Mansour discussed the medical options to treat those patients by presenting the results from a study that included 93,843 Finnish women aged 30 to 49 years using LNG-IUS for HMB treatment, comparing the incidence of cancers in this group of patients with that in the general population.20 It was found that using LNG-IUS lowered the incidence of endometrial adenocarcinoma, demonstrating the protective factor of LNG-IUS. 20 Regression to normal endometrium was observed in nearly all women with the use of LNG-IUS.20-24 Of note, even in women with atypia, the regression rate was still very high (Figure 3).21-24
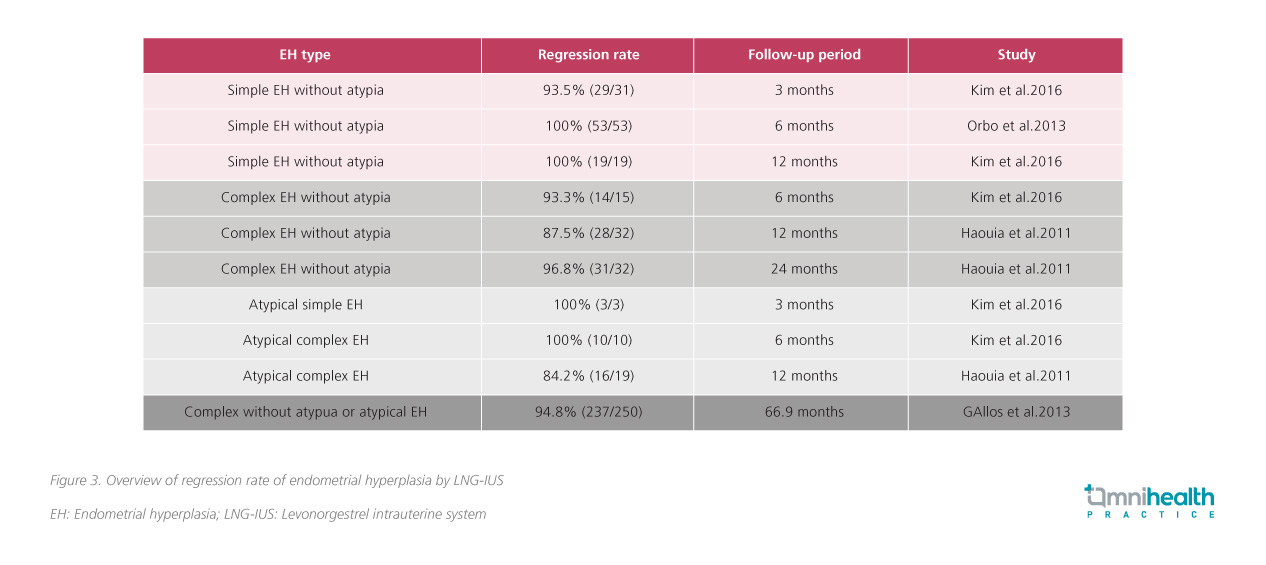
When compared with the other treatments like oral progestins, LNG-IUS is superior in treating hyperplasia-associated-HMB.22,23 Furthermore, it should be considered as the first choice for endometrial hyperplasia without atypia.25 Dr. Mansour highlighted that before considering hysterectomy, LNG-IUS should be considered according to patient’s need or wish.5
Conclusion
HMB adversely affects women’s daily living and may also lead to clinical consequences like iron deficiency anemia. In Hong Kong, patients are offered conventional medical treatments in a stepwise and non-specific fashion, which may not be optimal and sufficient for the treatment of HMB. A long-term, effective treatment should be offered upfront as an alternative to improve QoL and prevent iron deficiency efficiently. The NICE guideline recommends LNG-IUS as first-line treatment for HMB. Multiple studies have found that LNG-IUS not only reduces blood loss significantly in 3 months, but is also associated with substantial regression rate for endometrial hyperplasia. Besides, LNG-IUS is also recommended as first-line treatment for most nulliparous and parous women. For older patients at reproductive years, it is also considered as first choice treatment for endometrial hyperplasia without atypia upon investigation of risk factors for endometrial carcinoma.

