EXPERT INSIGHT
Pimecrolimus as a preferred option for mild-to-moderate atopic dermatitis - An updated recommendation for south and east asia
Eczema, also known as atopic dermatitis (AD), is a chronic, relapsing, inflammatory skin disease characterized by intense itch, recurrent eczematous lesions, and a fluctuating course.1,2 Statistics showed that up to 20% of children are affected by AD worldwide, while 15% of secondary school children in Hong Kong are reported to have the problem.3,4 In addition, evidence has suggested the prevalence of AD in Asia is on the rise.2 Although AD can be controlled through various proven strategies, optimizing AD management is still a challenge since certain situations, such as steroid phobia and poor patient compliance, could lead to treatment failure.4 In these regards, an algorithm for the topical AD treatment was developed and published in 2020 for use by the primary care physicians, pediatricians, and dermatologists in South and East Asia.2 In the interviews with Omnihealth Practice, Dr. Luk, Chi-Kong David and Professor Hon, Kam-Lun Ellis, authors of the practical recommendations, discussed the difficulties in managing mild-to-moderate AD, and shared their views on improving treatment outcomes in these AD patients.
Challenges in AD management
AD is a hereditary skin condition with fluctuating courses.5 However, the unrealistic expectations of curing AD in patients and their family members are very common in Hong Kong, thus often leading to non-compliance and treatment failure.4 “Patients must understand that AD is a chronic disease and there is no magic pill for disease cure,” Dr. Luk said. Although more and more treatment options are available for AD management, they might have little value for long-term disease control if the patients lack accurate information and sensible expectations about the disease. “Communication with the patients, therefore, is crucial to the treatment success”, stressed Dr. Luk.
Corticophobia is also common among patients in Hong Kong due to the concerns over skin atrophy and other potential side effects.2 Patients who are prescribed topical corticosteroids (TCSs) might discontinue the treatment prematurely to minimize steroid exposure.2 Since it can compromise the treatment outcome, patients’ attitude toward TCS must be assessed. An alternative to TCSs should be considered when the patients have concerns about steroid use.2 Steroid-sparing treatment strategies are therefore warranted.
Limitations of TCSs in mild-to-moderate AD management
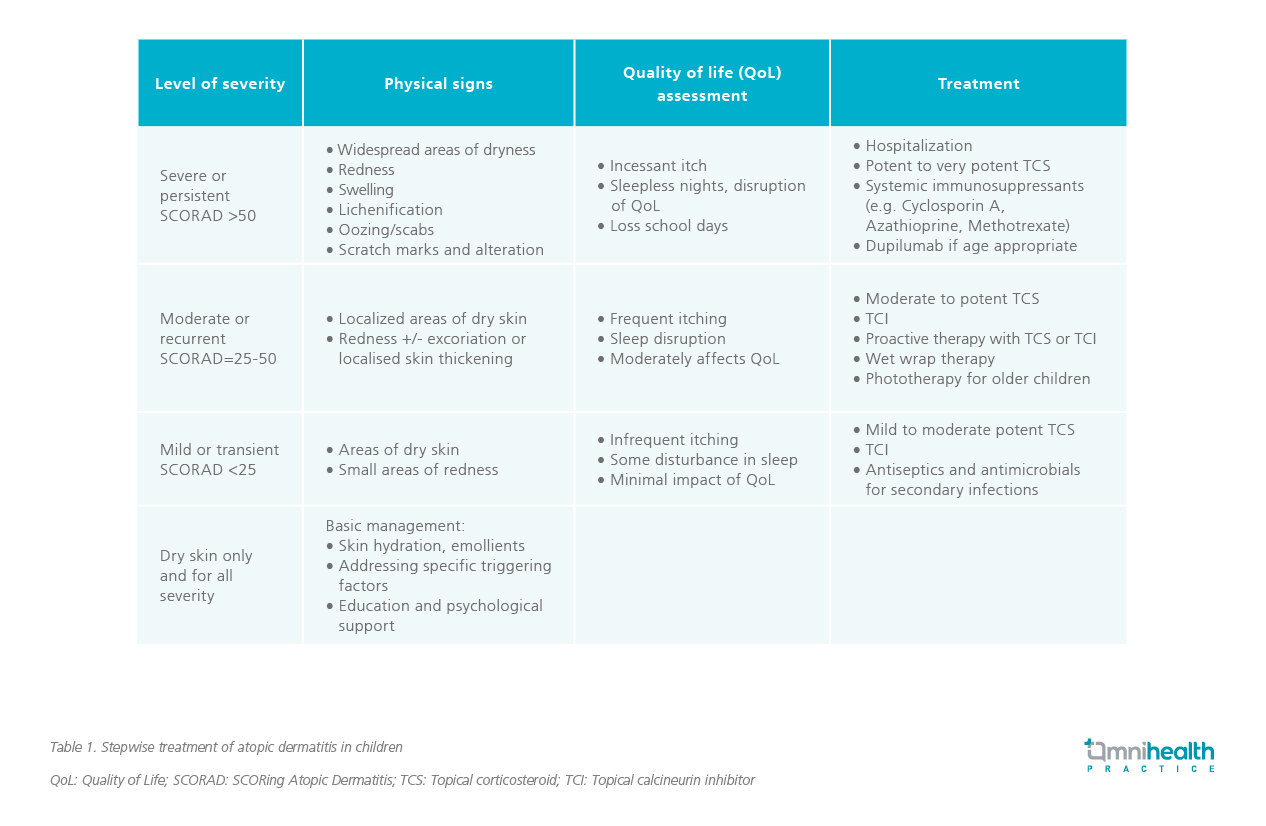
For mild-to-moderate AD patients, pharmacological agents are often required in the occurrence of acute flares. Although mild-to-moderate potent TCSs are regarded as first-line therapy recommended by the recently published paediatric AD management guideline (Table 1), other factors, including patients’ acceptance, site of AD lesions, and side effects of the medications, should also be taken into considerations when determining the most appropriate treatment option.2,4
Given steroid is associated with skin atrophy, the use of TCSs in sensitive skin areas such as face and neck may not be appropriate. Since these areas are susceptible to further skin barrier impairment, the use of TCSs could result in worsening of AD in the long run.2 Therefore, TCSs may not be an ideal treatment option in this scenario.
The emerging role of TCIs in mild to moderate AD
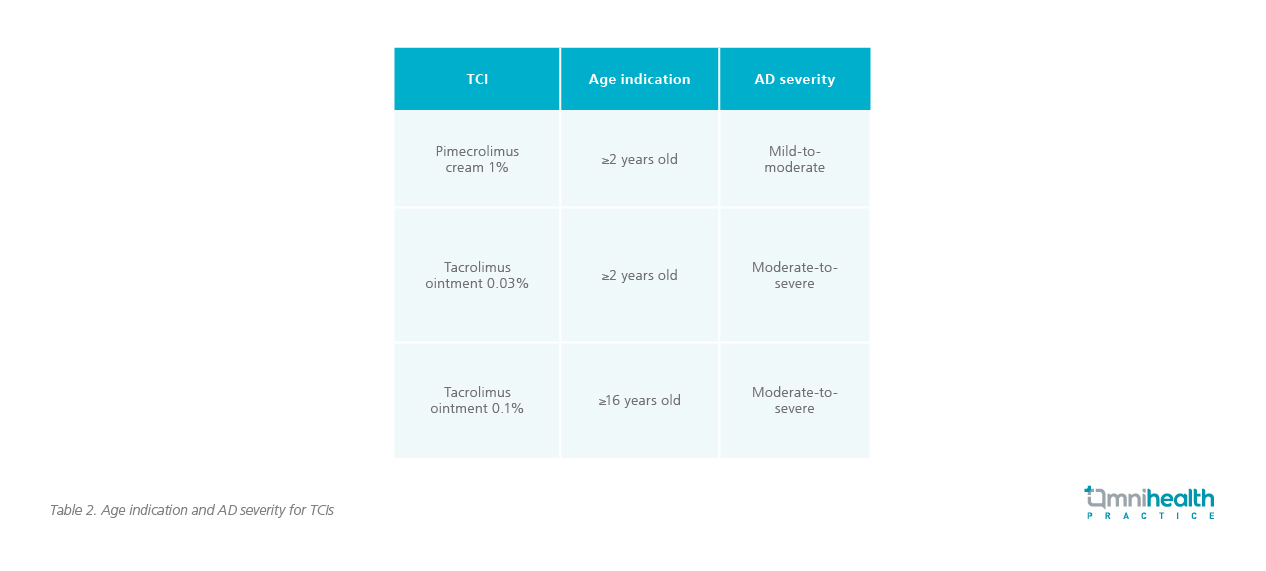
Considering the limitations of TCSs, an alternative is warranted to better manage acute flares and prevent flare recurrence. “The use of steroids is sometimes inevitable if AD is uncontrolled. The good news is that we have alternatives now,” said Prof. Hon. In corticophobic patients, topical calcineurin inhibitors (TCIs) could be used as a replacement. In contrast to skin atrophy of TCSs, TCIs have the advantage of increasing skin thickness. There are 3 TCI products currently available in the market, namely pimecrolimus cream 1% and tacrolimus ointments 0.03% and 0.1%. The pimecrolimus cream 1% and the tacrolimus ointment 0.03% can be applied in children as young as 2 years old for mild-to-moderate or moderate-to-severe AD, respectively (Table 2).4
TCI is an effective topical anti-inflammatory agent for acute flares and maintenance treatment in AD. It works by inhibiting calcineurin dependent T-cell activation and subsequently blocking the production of pro-inflammatory cytokines.6 Studies revealed the two TCIs demonstrated similar efficacy to that of the mid-potency TCSs.6 They are indicated for acute and proactive AD treatment.4 The recently published practical recommendations of AD management for South and East Asia, authored by Dr. Luk and Prof. Hon, suggest using pimecrolimus cream 1% in acute mild-to-moderate AD or continuous mild AD (Figure 1).2 Apart from the sensitive skin areas, it is also efficacious and recommended for controlling lesions on non-sensitive body locations (Figure 1).2 Tacrolimus ointment 0.03% and 0.1%, which are indicated for moderate-to-severe AD, is only recommended to be applied to non-sensitive skin areas.2
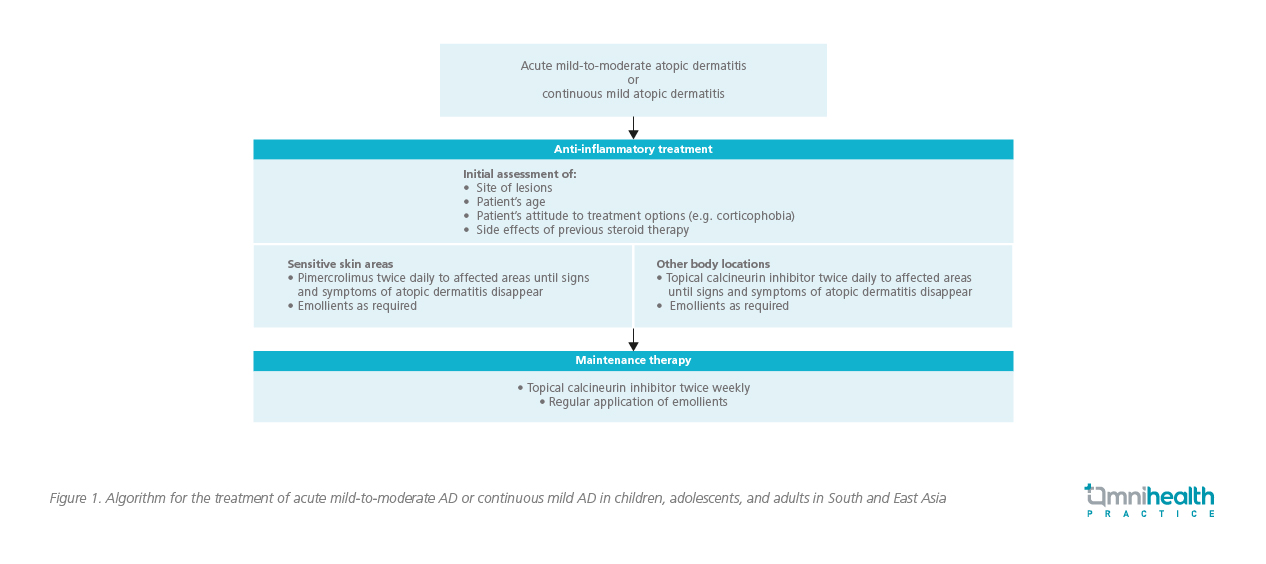
Once the acute flares are resolved, prevention of flare recurrence is of utmost importance to maintain the patient’s quality of life. The AD recommendations for South and East Asia recommend proactive maintenance therapy with twice-weekly TCI application and regular use of emollients to previously affected areas of skin in order to prevent flares from recurring, especially in moderate and recurrent AD.2,6 “Such a proactive therapy can decrease the frequency of AD flares while minimizing the potential side effects typically associated with the use of the medium- or high-potency TCSs,” said Dr. Luk.6
Selection of TCIs in mild-to-moderate AD
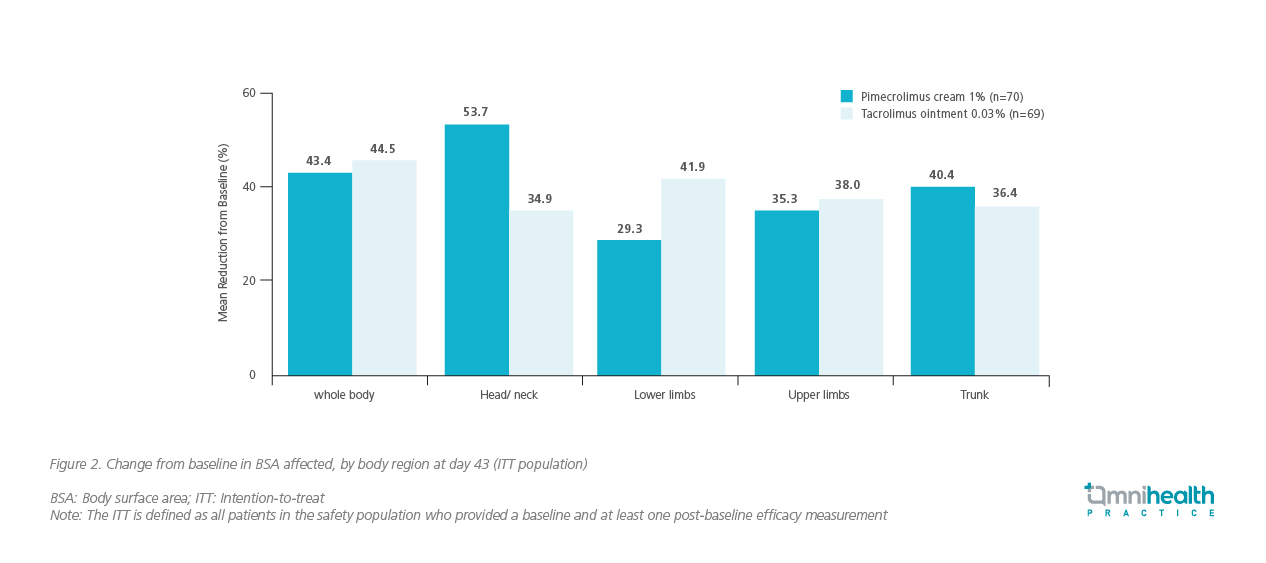
Both pimecrolimus cream 1% and tacrolimus ointment 0.03% are indicated for moderate AD. A study evaluating these 2 preparations showed similar overall efficacy and safety in paediatric patients with moderate AD.7 However, pimecrolimus cream 1% tended to achieve a better clinical outcome in the head and neck skin areas than tacrolimus ointment 0.03% (Figure 2).7 In addition, patients had higher acceptance of pimecrolimus cream 1% due to its less occlusive formulation.7 Since it is usually hot and humid during the summers in Hong Kong, the occlusive ointment preparation will not only render patients feel uncomfortable, trapping excess heat and sweat on the skin could also exacerbate the condition of AD.2 The less occlusive, non-sticky feel, and ease of rub-in features of pimecrolimus cream 1% are beneficial in the hot and humid climate of Hong Kong.2 “Pimecrolimus cream 1% is generally preferred by patients who dislike greasy preparations,” Prof. Hon added.
Ensuring safe use of TCIs
TCIs are generally well tolerated. The most common side effects are mild burning sensations that occur shortly after application, with pimecrolimus cream 1% causing less burning than tacrolimus ointments.2,7,8 The discomfort usually can resolve within a few days or with the emollient application.4 Although the United States Food and Drug Administration (FDA) issued a black box warning to all TCI products regarding concerns over increased lymphoma risks, clinical studies did not show any elevated lymphoma risk or other related cancers from TCI use. Of note, TCI-related malignancies have never been reported in Hong Kong, probably due to the lower potential of TCI for transcutaneous resorption, and hence minimizing the systemic exposure of the active drugs.2 That said, ultraviolet (UV) protection for TCI use to reduce the potential risk of carcinogenicity is still recommended.4
Suggestions of practical AD management strategies
“The regular use of emollients is the cornerstone in AD management,” stressed Prof. Hon. Provided that AD is a disease of the impaired skin barrier, the use of emollients can form a protective layer on the affected skin areas to keep skin hydrated and reduce their contact with allergens. Maintaining a balanced diet is also important. “Do not avoid over 2 to 3 types of food at the same time without consulting an expert physician as it can lead to malnutrition, which could be fatal if serious,” he added. Prof. Hon also suggested treating AD early, saying with proper treatment, AD symptoms can be relieved as early as 2 days. While treating AD symptoms, topical preparations should be selected with caution, especially for sensitive skin areas. For example, if the affected area is on the face, pimecrolimus cream 1% should be used, while TCSs should be avoided.
Besides, Dr. Luk emphasized the importance of psychological support for AD patients since AD-related suicide and homicide have been reported locally. Psychological and psychiatric intervention are crucial to providing timely support to the patients and their families. Psychotherapy, counselling, behavioral therapy, and the relaxation techniques could help the patients and their families better cope with the stress from the disease. In addition, Dr. Luk highlighted the importance of appropriate bathing and showering to remove sweat from the skin, particularly amid the humid and hot summers in Hong Kong. He recommended bathing daily in tepid or lukewarm water thoroughly but gently for not more than 10 minutes. When performing outdoor activities, sunscreen should be applied to protect the skin against UV light. Avoiding the triggers is necessary for preventing AD exacerbation. Therefore, Dr. Luk suggested asking patients to record the symptoms daily so as to find out the triggers.
Both Dr. Luk and Prof. Hon agreed that the success of AD treatment heavily relies on the cooperation between healthcare professionals (HCPs), parents and patients. They strongly suggested HCPs should allow sufficient time to educate patients during the initial consultations. Besides, HCPs should convey the messages to all AD patients clearly that while a cure may not be achieved shortly. It is important to improve the symptoms and control the inflammation of AD early to prevent the exacerbations. It is particularly crucial for HCPs to agree on a treatment plan and goals with the patients and address the concerns regarding each possible treatment option, especially when the use of steroids is unavoidable. Last but not least, since the Coronavirus Disease 2019 (COVID-19) vaccines are not contraindicated in AD patients, COVID-19 immunization is still recommended unless there is known hypersensitivity to the vaccines.
Conclusion
Since TCS is still the mainstay of treatment in AD management, understanding patients’ perception regarding the use of steroids is of paramount importance to avoid non-compliance. If corticophobia is identified, TCIs can be the alternatives. For mild-to-moderate AD, which accounts for about 90% of all AD cases, pimecrolimus cream 1% is recommended for treating all skin areas, including head and neck skin, in patients aged 2 years or up.9 For acute flares, the AD recommendations for South and East Asia recommend a twice-daily TCI regimen until signs and symptoms of AD disappear; as for maintenance therapy, a twice-weekly TCI regimen with regular application of emollients on the affected area is recommended. TCIs are generally well tolerated, with mild side effects usually resolving within a few days of application or with the use of emollients. Although TCI-related malignancies have not been reported in Hong Kong, and studies did not show any increased risk of lymphomas concerning the use of TCIs, UV protection for the use of TCIs is still recommended to minimize the risk of carcinogenicity.

