CONFERENCE UPDATE: ENDO 2021
Minimizing acute endocrinopathy associated with immune checkpoint inhibitors
Immunotherapy has revolutionized the treatment of cancer, yet its increasing use has exposed cancer patients to an increased risk of immune-related adverse events (irAEs).1,2 These adverse reactions are usually mild to moderate albeit severe irAEs which are occasionally reported in the literature are associated with a mortality rate of 2%.1 In particular, chemotherapy-induced irAEs often occur rapidly following the initiation of treatment whereas immunotherapy-related irAEs usually have a delayed onset.1 As such, the early recognition irAEs and clinical interventions are important to reduce mortality.
Dr. Carla Moran, Associate Professor of the University College Dublin School of Medicine and Consultant Endocrinologist of the Beacon Hospital and the St. Vincent’s University Hospital of Dublin, Ireland, elaborated that upon encountering suspected adrenal crisis cases, blood cortisol should be tested and 100mg hydrocortisone should be given immediately followed by 50mg daily through the intravenous or intramuscular routes. For suspected hypophysitis as confirmed with random blood cortisol of <100nmol/L or blood cortisol of <200nmol/L at 9 a.m., Dr. Moran recommended hydrocortisone of 10, 5 and 5mg via oral route in the morning, afternoon and evening, respectively.
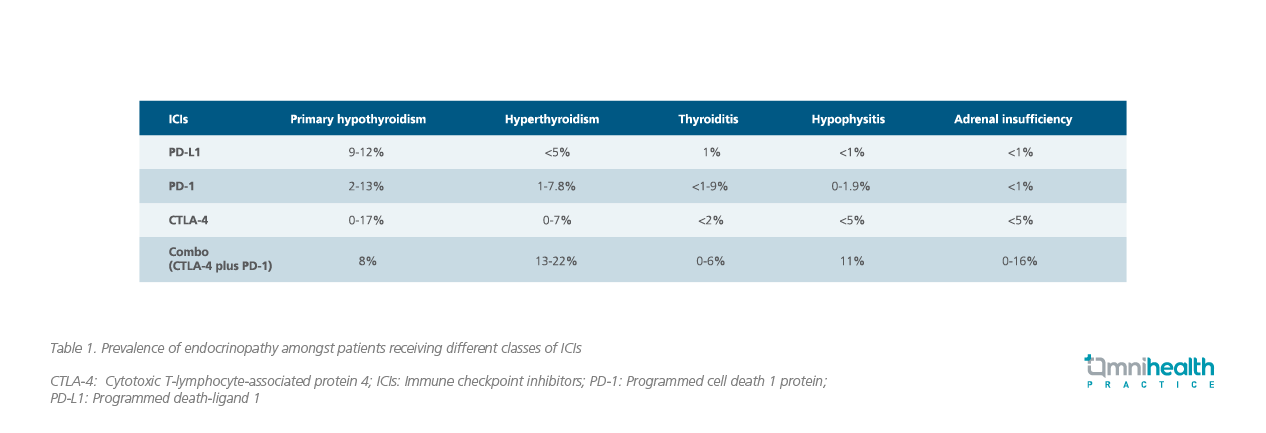
When considering immunotherapy with immune checkpoint inhibitors (ICIs), programmed death-ligand 1 (PD-L1) inhibitors (e.g., atezolizumab, durvalumab, avelumab) typically have less irAEs than programmed cell death 1 protein (PD-1) inhibitors (e.g., nivolumab, pembrolizumab) or cytotoxic T-lymphocyte-associated protein 4 (CTLA-4) (e.g., ipilimumab) (Table 1).2
While ICIs are not contraindicated in patients with pre-existing thyroid disease, Dr. Moran noted that ICI treatment can be temporarily suspended if severe orbitopathy (sight threatening) develops.3,4 In most cases, ICI therapy can be continued after temporary withdrawal and high-dose steroids are rarely required. Notably, while most irAEs usually occur within 3 months following the ICI therapy, some may occur later and close monitoring of endocrine conditions should be done in cancer patients receiving ICIs.3-6 Dr. Moran concluded, “Endocrinologists should be aware of the signs of acute adrenal crisis and suspected hypophysitis in cancer patients receiving ICIs.”

