Managing anorexia nervosa-associated low bone density in young women
Anorexia nervosa (AN) ranks the third most common chronic illness among adolescent girls and is associated with a 5.6% mortality rate per decade.1 Comparing to healthy individuals, girls with AN had significantly lower total body, lumbar and hip bone mineral density (BMD) (all p<0.001) that can be contributed to the increased deposition of adipose tissue in the bone marrow and the dysregulated activity of the growth hormone (GH)/insulin-like growth factor-1 (IGF-1) axis.1,2 Indeed, low BMD is highly prevalent in girls with AN with 41% of whom having a BMD z-score of ≤-1 and 11% having z-score ≤-2.1
Estrogen replacement is a mainstay of therapy for increasing BMD by reducing marrow adipose tissue deposition through the inhibition of Pref-1 and sclerostin.3 Specifically, Pref-1 inhibits the differentiation of mesenchymal stem cell in the marrow into osteoblasts whereas sclerostin inhibits the canonical WNT signaling pathway and osteoblastic activity.3 In other words, suppressing Pref-1 and sclerostin could restore the activity of osteoblasts and improve BMD.
However, Professor Madhusmita Misra, Talbor Professor of Pediatrics at the Harvard Medical School and Chief of the Division of Pediatric Endocrinology at the Massachusetts General Hospital for Children, noted that the oral administration of estrogen is often hindered by the hepatic first-pass effects which downregulate the production of IGF-1, an important bone-trophic hormone.4,5 In this connection, transdermal estrogen may be more effective in improving BMD due to the lack of IGF-1 inhibition.4
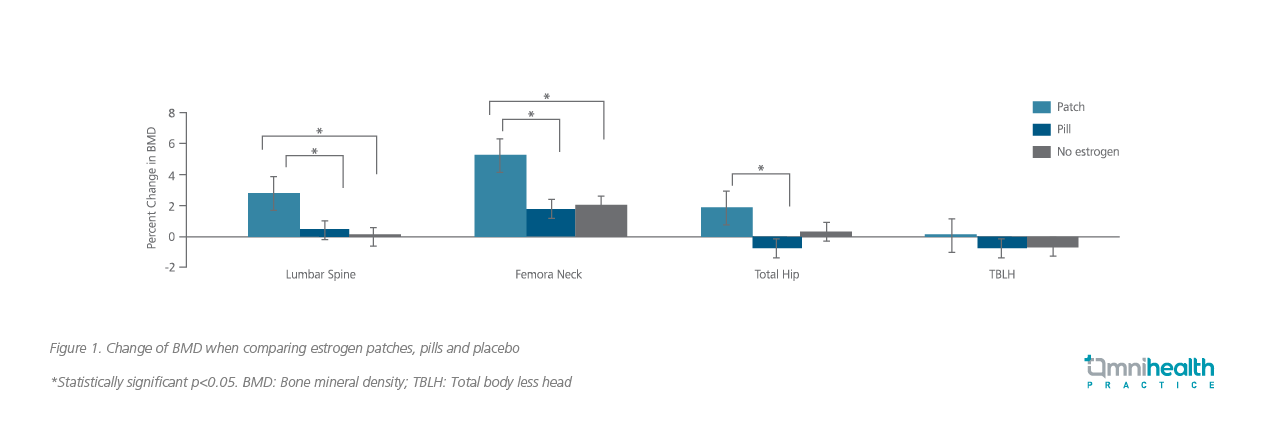
To evaluate the effectiveness of transdermal estrogen patches, a three-arm clinical trial comparing transdermal patch estrogen versus oral estrogen versus placebo showed that the greatest increase of BMD in the lumbar spine, femoral neck and total hip in the group receiving estrogen patch (Figure 1).4 In addition, the patch group had the greatest increase in tibial trabecular number and trabecular volumetric BMD.4 In another 18-month randomized control trial comparing estradiol patch versus oral medroxyprogesterone, a significant increase in spinal and hip BMD was observed with transdermal estradiol replacement plus cyclic oral progestin among AN patients aged 12 to 18-years-old.5 With both studies supporting the effectiveness of transdermal estrogen in improving BMD among women with AN, Prof. Misra concluded, “The [estrogen] patch but not the pill is effective in improving bone outcomes.”