CASE REVIEW
Revolutionizing orbital fracture repair with 3-dimensional printing: Sharing of local cases
Orbital fractures are amongst the commonest form of facial trauma and often require orbital reconstruction for proper management.1,2 However, the operation remains challenging as the procedure not only requires surgeons to possess profound anatomical knowledge and detailed preoperative planning, but also prudent judgement during the surgery to avoid compromising the visual function and facial appearance.1,2 With the advancement of computer-assisted technologies, many of these surgical challenges can now be handled.2 In a recent interview with Omnihealth Practice, Dr. Chong, Kam-Lung Kelvin introduced an innovative approach on the orbital reconstruction utilizing a combination of 3-dimensional (3D) printing and semi-automatic computerized segmentation process that can save valuable surgical time and effort in implant shaping and fitting during orbital fracture repair. (Information supplemented by Dr. Chin, Kar-Yee Joyce)
An emerging opportunity to improve current surgical approach towards orbital fractures
Approximately 40% of all craniomaxillofacial traumas are orbital fractures, of which blow-out fractures are the most common due to the central and exposed position of the orbit as well as the fragile composition of its surrounding bone tissues.2-4 Clinically, patients with orbital floor involvement are often presented with diplopia especially on looking up or enophthalmos due to the loss of bony support.2,5 While blunt trauma around the eyes does cause typical alarming symptoms of eyelid swelling, bruises and subconjunctival hemorrhage, many patients may not be aware of other concerning symptoms including double vision, enophthalmos and cheek numbness. Majority of them are referred to ophthalmologists weeks after their initial injuries.
Orbital floor and medial wall are the thinnest bone in our body and therefore standard methods of open reduction and internal fixation are not feasible options.4 Instead, surgeons often opt for orbital floor reconstruction to restore vision, visual function and periocular appearance when the symptoms of orbital fractures become apparent.4,6 However, orbital reconstruction surgery remains a challenging procedure due to the limited view and access to the bony defect from the tight orbital space created by lifting or shifting the eyeball intraoperatively.4 Also, while computed tomography (CT) serves as the gold standard for reviewing and identifying orbital fractures, its isolated use without additional processing only provides 2-dimensional (2D) imaging that is difficult to translate to the 3D , intricate and delicate shape of the orbit.1,7,8
Conventionally, a flat malleable metal retractor is inserted after manual bending under the eyeball to lift up the orbital content until the fracture site is completely visualized. Unstable bone fragments are removed. Entrapped or prolapsed orbital tissues are released and repositioned when the orbital content is lifted away by the malleable retractor. Surgeons then need to anticipate the 3-dimensional shape of the orbital defect and fashion it out from commercially available flat implant sheet and shape it manually. Repeated implant fitting, repositioning and retrieval is then carried out which may lead to iatrogenic trauma to the already injured orbital tissues.5 Despite the labor-intensive and time-consuming effort, inadequate bony defect coverage, implant displacement or impingement on orbital tissues are not uncommonly reported leading to suboptimal surgical outcomes.1
The choice of orbital implant material has been a long-term topic of debate: while titanium mesh has been commonly used in other hand and neck region for fracture reconstruction, its use in orbital fracture has been associated with long-term peri-implant extraocular muscle fibrosis and progressive worsening of double vision.1,9
Combining conventional 2D imaging and the latest 3D printing technology
To address the limitations of traditional CT imaging and manual molding of implant and instrument intraoperatively,2 the authors proposed “3D-printing for surgical instrument and orbital molds (3SIOM)” as an innovative technique that leverages conventional 2D CT imaging and novel 3D printing to improve efficacy and safety of orbital fracture repair.10
During preoperative planning, the regions of interest over the patient’s fractured orbit as well as the contralateral, uninjured orbit from 2D orbital CT scans are semi-automatically segmented by a patented machine-learning and computer vision algorithm.10,11 The digital data is then transformed into a 3D stereolithography model. Using mirror image overlay (MIO) technique, the patient’s uninjured orbit was mirrored as a template onto the contralateral, fractured side to simulate its pre-injured shape.10,11
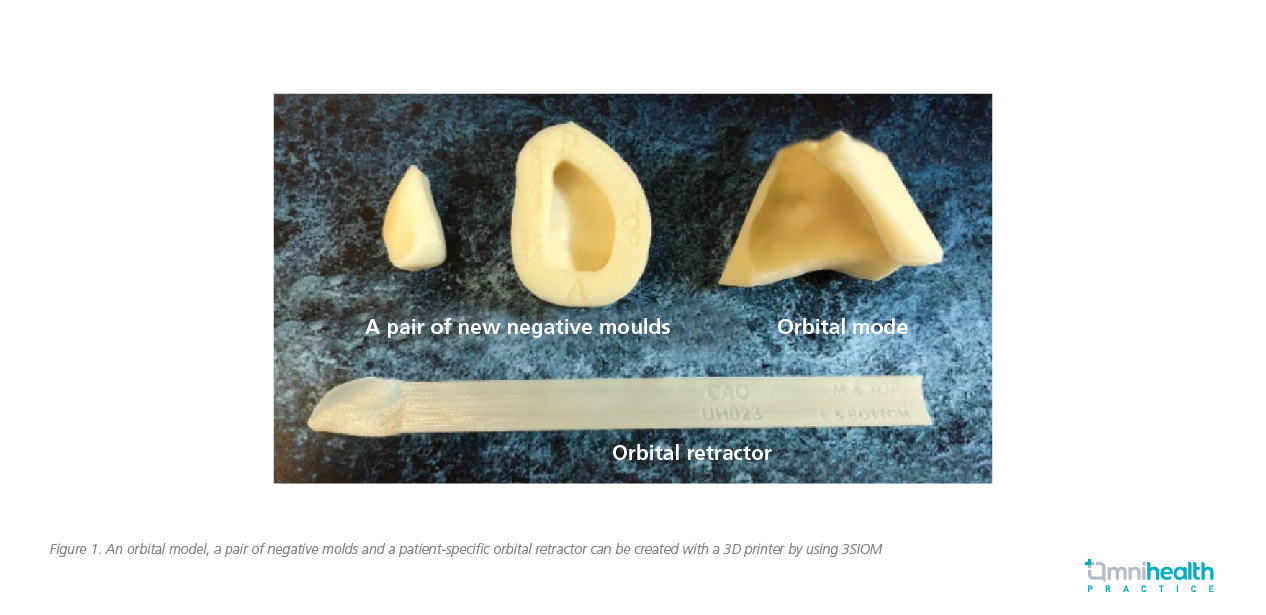
After segmenting the CT images into a 3D stereolithography model, a 3D “preinjured” model of the fractured region will be generated through a professional grade 3D printer (Fortus 400mc, Fused Deposition Modeling (FDM) system, Stratasys Inc., Eden Prairie, MN).10 The orbital model is paired with a set of negative molds that is used to manually shape any commercially available, 2D implant sheets from porous polyethylene with/without barrier surface, composite porous polyethylene-titanium mesh implant to absorbablesheets such as 85:15 poly (L-lactide-co-glycolide) or polycaprolactone.10 Importantly, 3SIOM generates patient-specific surgical instruments including orbital tissue retractor to assist the complete retraction of prolapsed orbital tissues before implant insertion. The patient-specific retractor bears the shape of each patient’s orbit and facilitates gentle and ergonomically-friendly tissue retraction (Figure 1).10 The 3D printing material used is ABSm30i of 0.127mm resolution, biocompatible (ISO 10993 USP Class VI) and the final products can be sterilized by heat up to 110oC.10
During orbital fracture operation, surgeons may also obtain realtime coordinates in particular to confirm the clearance of posterior edge of the fracture defect under the guidance of intraoperative navigation.2 This image-guided approach can minimize subjectivity and document surgical landmarks during complex orbital surgeries.2 Last but not least the posterior edge of the fracture, infraorbital nerve and the safe placement of the orbital floor implant can be readily visualized with the use of transantral endoscopy.10
Favorable adoption of 3SIOM: A sharing of local experience
The performance of 3SIOM was investigated in a pilot study (supported by Innovation and Technology Commission) that explored the application of additive manufacturing based on semi-automated image segmentation and endoscopy in assisting unilateral orbital reconstruction.10 Patients who had post-trauma orbital fracture with primary or down-gaze diplopia, ≥2mm enophthalmos, persistent infraorbital numbness and >50% orbital wall involvement were included.12
Among the 10 patients who underwent 3SIOM-assisted large orbital fracture repair or orbital reconstruction, the preoperative chair-time on image segmentation by software engineers was only 4-6 minutes using 3SIOM’s semi-automatic software-programmed segmentation process. Compared to the standard manual segmentation process which took an average of 4-6 hours, 3SIOM had significantly reduced the time needed for CT image segmentation per case (p<0.01).10 The study team revealed that this proves to be one of the most challenging tasks of the study as existing segmentation method in medical imaging typically does not account for CT artifacts and noise.13 As orbital bones are the thinnest structures in human bodies, certain part of the CT images of intact, normal orbital walls are too thin to be recognized and correctly segmented by standard segmentation algorithm. Orbital fractures are therefore inherently subject to segmentation errors which requires intensive manual adjustments and anatomical modeling for correction.13
On the other hand, the availability of an ergonomically-friendly tissue-retractor and a pair of negative molds for implant contouring evidently reduced the operative time required to shape and fit the implants from 20-30 minutes to 2-3 minutes (p<0.05).10 Such benefit was consistent across different subjects in the study.10
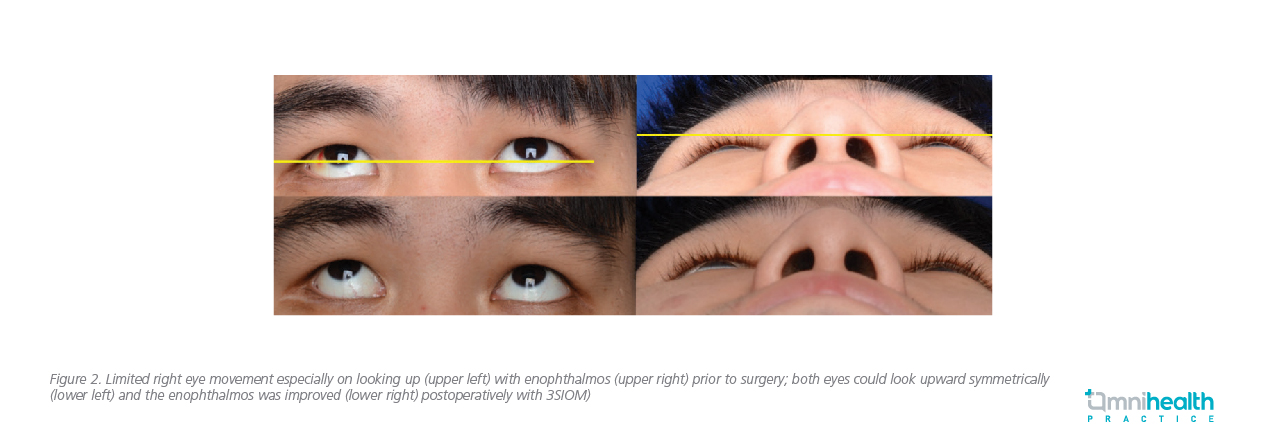
In this case review, 2 local patient cases were shared to illustrate the benefits of 3SIOM. The first patient was a 26-year-old male with good medical and ocular health who had sustained right eye blunt trauma by opponent’s elbow during a handball game in December 2017. CT scans of his orbits showed large blowout fracture of the right eye orbital floor and part of the medial wall. Apart from severe periorbital swelling, he had limited right eye movement especially on looking up and out, and he suffered from primary and down-gaze diplopia as well as infraorbital numbness. He received 3SIOM-assisted orbital fracture repair and insertion of implant in January 2018. He had good postoperative recovery with improvement of double vision and eye movement with some residual facial numbness (Figure 2). Postoperative CT scan done in November 2018 showed satisfactory repair of the orbital fracture with prolapsed orbital soft tissue repositioned. Dynamic MRI revealed improved vertical and horizontal movement of the right eye.
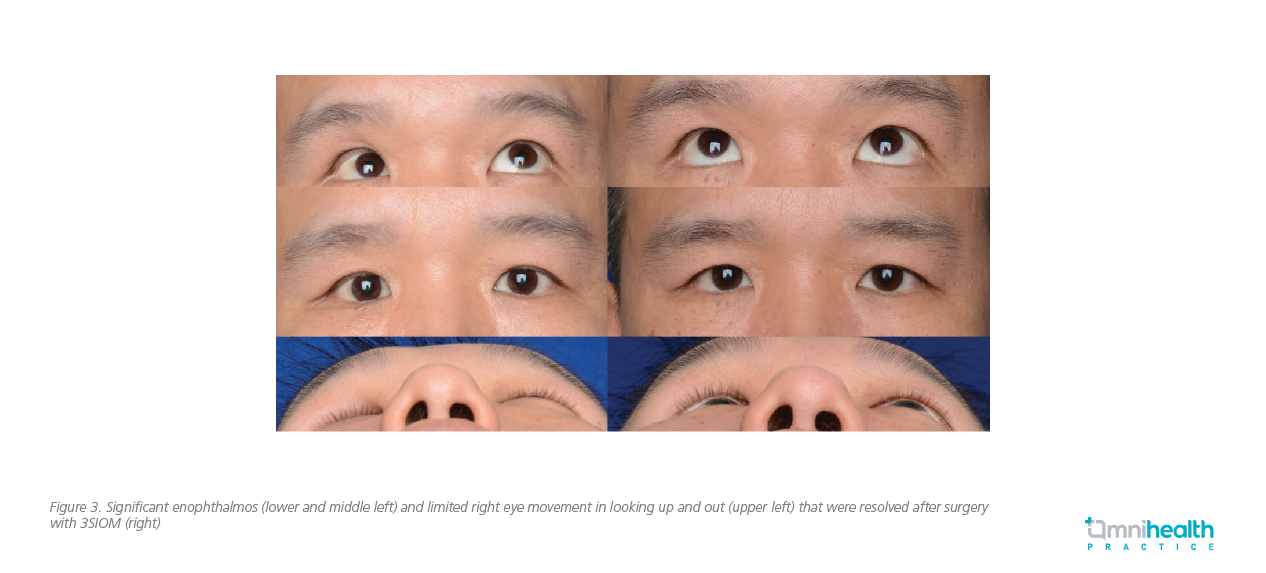
The second patient was a 41-year-old male who had sustained right eye blunt trauma resulting in diplopia in 2015. However, he did not seek for any medical attention until another episode of right eye blunt trauma that occurred in April 2017 when he slipped and fell after drinking. He had significant enophthalmos due to the combination of old and new orbital fractures as well as limited right eye movement especially on looking up and out. He complained of primary and down-gaze diplopia as well as infraorbital numbness. His orbital CT scans showed large blowout fracture of the right eye orbital floor and medial wall. He also underwent 3SIOM-assisted orbital fracture reconstruction. He had significant improvement in his enophthalmos and diplopia after the operation (Figure 3). Postoperative CT scan and dynamic MRI scan done in April 2018 showed satisfactory repair of orbital fracture and symmetrical eye movement after the operation.
Message to physicians
While the traditional orbital reconstruction technique has been widely practiced and had reasonable success rate in managing ocular fracture, there is still room for optimization to conserve resources and time both during the preoperative planning and intraoperative stages. In particular, as standard CT images are 2D in nature, it is often difficult, if not impossible, to translate the information into 3D anatomical shape for surgeons.
3SIOM holds the potential as a more cost-effective and accurate supporting technique for orbital reconstruction. As a semi-automated process, 3SIOM still requires some degree of manual input including uploading the scanned CT images and starting the medical image processing software. Previous studies have demonstrated that convolutional neural networks with deep supervision, a deep-learning method, can achieve expert-level accuracy in the segmentation of hematoma or intracranial structures from CT brain scans.14,15 Deep learning assisted image segmentation may further conserve time and improve accuracy for both the software engineers and surgeons involved in the orbital fracture reconstructions. The authors are currently investigating the role of 3SIOM in complex orbital fracture and patients undergoing revision orbital reconstruction.

