EXPERT INSIGHT
A patient-centered approach to optimizing T2D management with health-related quality of life in mind
According to the American Diabetes Association (ADA)/ European Association for the Study of Diabetes (EASD) guideline, a patient-centered approach to type 2 diabetes (T2D) management should be adopted with the goal of not only preventing complications but also optimizing patients’ quality of life.1 To achieve these goals, factors that affect health-related quality of life (HRQoL) such as social determinants of health, psychosocial well-being, and health behaviors are key considerations in glycemic management strategies for patients with T2D.1 At the EASD Annual Meeting 2023, Professor Chan, Chung-Ngor Juliana from the Department of Medicine and Therapeutics, The Chinese University of Hong Kong presented the results of a cross-sectional analysis of HRQoL in patients with T2D treated with oral glucose-lowering drugs (OGLDs) who were enrolled in the Joint Asia Diabetes Evaluation (JADE) Register. In a subsequent interview with Omnihealth Practice, Prof. Chan shared further insights on the application of the JADE® Program, shedding light on the dynamics between glycemic management strategies and patients’ HRQoL.
The need for HRQoL-focused approaches in young patients with T2D
T2D is a chronic condition that can be detrimental to patients’ HRQoL. Coexisting conditions such as hypertension, heart failure, neuropathy, retinopathy, nephropathy, and diabetic foot syndrome not only contribute to frequent medical appointments and hospitalizations, but also negative emotions, including low self-esteem, frustration, and depression.2 Prof. Chan highlighted that in some surveys, diabetes distress was a prominent psychological condition in over a third (36%) of patients with T2D.3 Distress is a feeling of being overwhelmed by the demands on self-management including strict adherence to treatment regimens and lifestyle modifications (LSMs) during one’s journey of living with diabetes.3 These comorbidities and negative emotions can adversely affect the HRQoL of patients with T2D.3
The devastating effects of T2D on patients’ HRQoL are particularly evident in patients with young onset of diabetes, arbitrarily defined as age of diagnosis before 40 years.4 These patients face long disease duration which puts them at a higher lifetime risk of micro and macrovascular complications than patients with an older age of disease onset, which can lead to a steep decline in HRQoL.4 Prof. Chan highlighted that roughly 1 in 5 patients had youngonset diabetes in Hong Kong.5 In a recent local study, patients with young-onset T2D had 3 times higher cumulative glycemic exposure and a more rapid rate of glycemic deterioration than their counterparts with older onset of diabetes.6 In the prospective Hong Kong Diabetes Register (HKDR), patients with young-onset T2D had a 3.6-fold [hazard ratio (HR)=3.57; 95% confidence interval (CI): 2.94-4.33] higher risk of developing cardiovascular diseases (CVDs) and 2.2-fold (HR=2.17; 95% CI: 1.80-2.63) higher risk of death than those with an older onset of diabetes.4 Furthermore, the development of complications in patients with diabetes was associated with marked decrements in HRQoL which often did not improve after the event.7 With the demographics of T2D shifting towards a younger population with an anticipated increased burden of complications, optimizing HRQoL is a key outcome in glycemic management.
Patient empowerment and HRQoL
Empowerment is a patient-centered approach proven to be effective in attaining treatment goals and improving psychological well-being.8 It encourages patients to be actively involved in health decisions instead of passively following orders from healthcare providers.8 Patient empowerment starts by equipping them with the necessary knowledge and skills that influence the progression of T2D accompanied by a personalized treatment regimen that balances clinical efficacy and patients’ preferences.8 These strategies help motivate patients to make informed decisions and adhere to long-term treatment.8
Multiple clinical studies have demonstrated that empowered patients with T2D were less likely to have diabetes distress, anxiety and depression.8 A 3-month empowerment-based care program with an emphasis on establishing personally meaningful goals, facilitating collaborative partnerships with shared decision-making, and resolving life-disease conflicts via situational reflection reduced diabetes distress (including emotional and regimen distress) and improved overall QoL.8 This was accompanied by reduced physician-related distress after 1 week of implementation of the program.9 Aside from psychological benefits, empowerment-based interventions have also been shown to improve glycemic control.10
The JADE® Program: A platform for promoting quality assurance and identifying care gaps in diabetes
To facilitate patient empowerment, Prof. Chan said that physicians should understand their patients' risk profiles, care standards and unmet needs. To that end, HKDR established in 1995 aims to empower patients with their personalized risk profiles and help doctors individualize treatment through stratifying risk and triaging care.11 In 2000, the HKDR protocol was adopted to become a territory-wide risk assessment and management program.11 In 2007, the HKDR was digitalized to establish the web-based JADE® Program used in over 11 Asian countries/regions.11 Based on risk algorithms generated from the HKDR, the JADE® portal gathered data and issued personalized reports with risk categories and 5-year probabilities of complications aimed at reducing clinical inertia and empowering self-management.11,12
Prof. Chan emphasized that the JADE® Program is an evidence-based diabetes multisystem assessment aimed at driving actions and is more than just blood and urine tests. During a single visit, the JADE® portal guides providers to perform structured assessments and gather information systematically including sociodemographics, comorbidities, disease duration, medications, and patient-reported outcomes such as lifestyles, self-management and HRQoL, along with other physical and laboratory measurements.11 These structured assessments mark the beginning of a journey of patient education, empowerment and engagement.11 In line with international recommendations, these comprehensive assessments should be performed at diagnosis and every 12-24 months for quality improvement.1,11 When linked with other clinical informatics and biogenetic markers, the big data gathered during this integrated assessment, empowerment and management program can track secular trends to identify unmet needs and verify interventions in a naturalistic environment.11
At the EASD Annual Meeting 2023, Prof. Chan presented the results of a cross-sectional analysis based on the real-world data from the JADE® Program, which examined factors associated with HRQoL of patients with T2D treated with OGLDs.12 During the assessment, participants completed the self-reported EuroQol 5 Dimension 3-Level survey (EQ- 5D-3L), which is a standardized measure of HRQoL encompassing 5 dimensions of mobility, self-care, usual activities, pain/discomfort, and anxiety/depression.12 After excluding patients treated with insulin or glucagon-like peptide-1 receptor agonists (GLP-1RAs), 47,895 patients treated with OGLDs and/or lifestyle modification (LSM) with complete EQ-5D-3L data enrolled in the JADE® Program between November 2007 and December 2019 were included.12
The EQ-5D-3L index of each patient was estimated within a range of 1 to 0, with 1 indicating full health and 0 indicating a state similar to death.12 With a median EQ-5D-3L index score of 0.796, the study Conclusion The patient demographic of T2D is shifting towards a younger population associated with long disease duration, high lifetime risk of comorbidities and decrements in HRQoL.4-7 Prof. Chan concluded that 20% of Asian patients with T2D treated with OGLDs experienced some problems, notably with anxiety, depression, pain, or discomfort. As such, the implementation of patient-centered approaches with patient empowerment is an important strategy to optimize treatment outcomes and HRQoL.8-10 Aside from LSMs, the choices of OGLDs could also influence HRQoL with gliclazide-treated patients having better HRQoL than other users of SUs.12 Taken together, this real-world evidence supports the safety, effectiveness and tolerability of gliclazide as a preferred OGLD among Asian patients with T2D. population was categorized into 3 groups of high (=1) (n=25,943), medium (≥0.796-1) (n=8,455), or low (<0.796) (n=8,415) EQ-5D-3L index scores.12 On univariate analysis, patients with low EQ-5D-3L index scores (<0.796) were older, more likely to be female, less physically active, and had longer disease duration and cardiometabolic risk factors such as hypertension, dyslipidemia and obesity (p<0.001 for all).12 These patients also had higher levels of hemoglobin A1c (HbA1c) and were more likely to experience peripheral sensory neuropathy (PSN), coronary heart disease (CHD), stroke, and heart failure (p<0.001 to all). They were also more likely to receive ≥3 OGLDs, renin-angiotensin system (RAS) inhibitors, or statins (p<0.001 to all).12
On multivariate analysis, male gender, college or above education, adherence to a balanced diet and regular exercise (≥3 times/week) were associated with an EQ-5D-3L index score of 1 (p=0.003 for balanced diet, p<0.001 for others).12 On the other hand, stroke, self-reported hypoglycemia, PSN, CHD, smoking, HbA1c, older age, higher BMI and longer disease duration were associated with poor HRQoL (p=0.012 for CHD, p=0.036 for HbA1c, p=0.001 for disease duration, p<0.001 for others).12
Associations of lifestyle modification and OGLDs with HRQoL
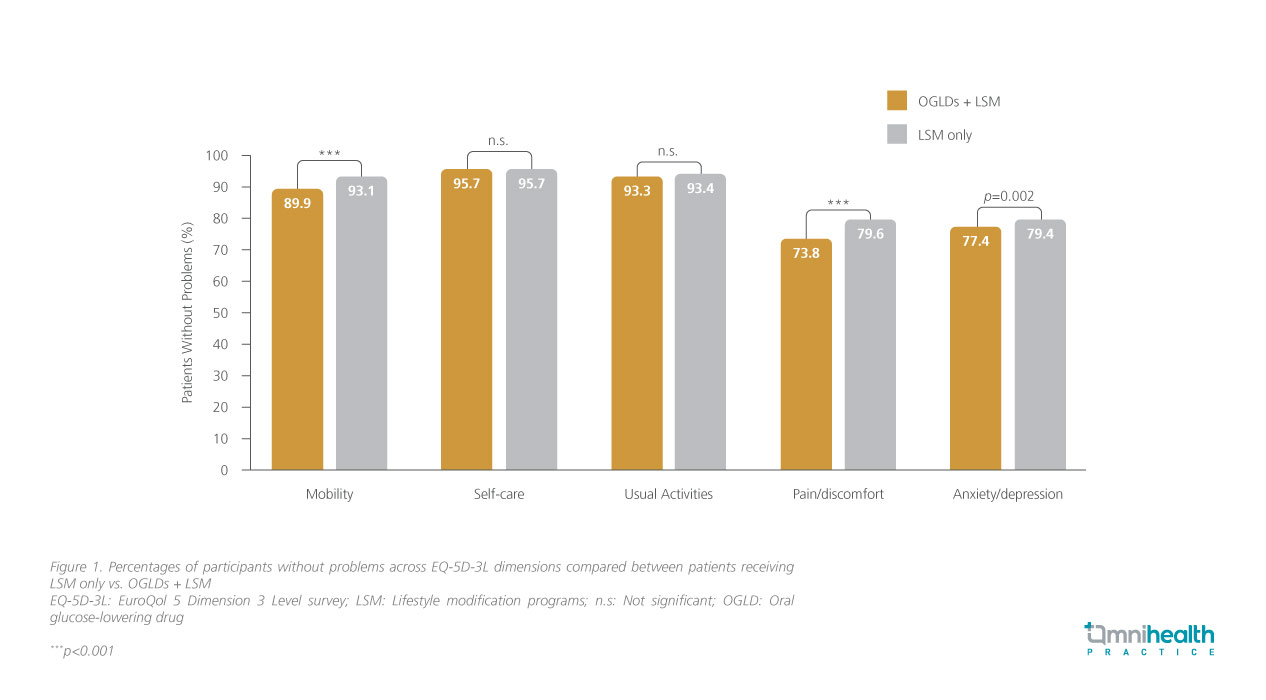
In this analysis, treatment modalities were also associated with EQ- 5D-3L scores.12 A total of 5,082 patients received LSM only, while the majority (n=42,813) had both OGLDs and LSM.12 Patients who received LSM only had a higher index score (0.910 vs. 0.896; p<0.001) with more participants having a high EQ-5D-3L score (64.5% vs. 60.6%; p<0.001).12 More patients treated with LSM reported “no problem” in the mobility (p<0.001), pain/discomfort (p<0.001) and anxiety/depression (p=0.002) categories than patients treated with OGLDs (figure 1).12
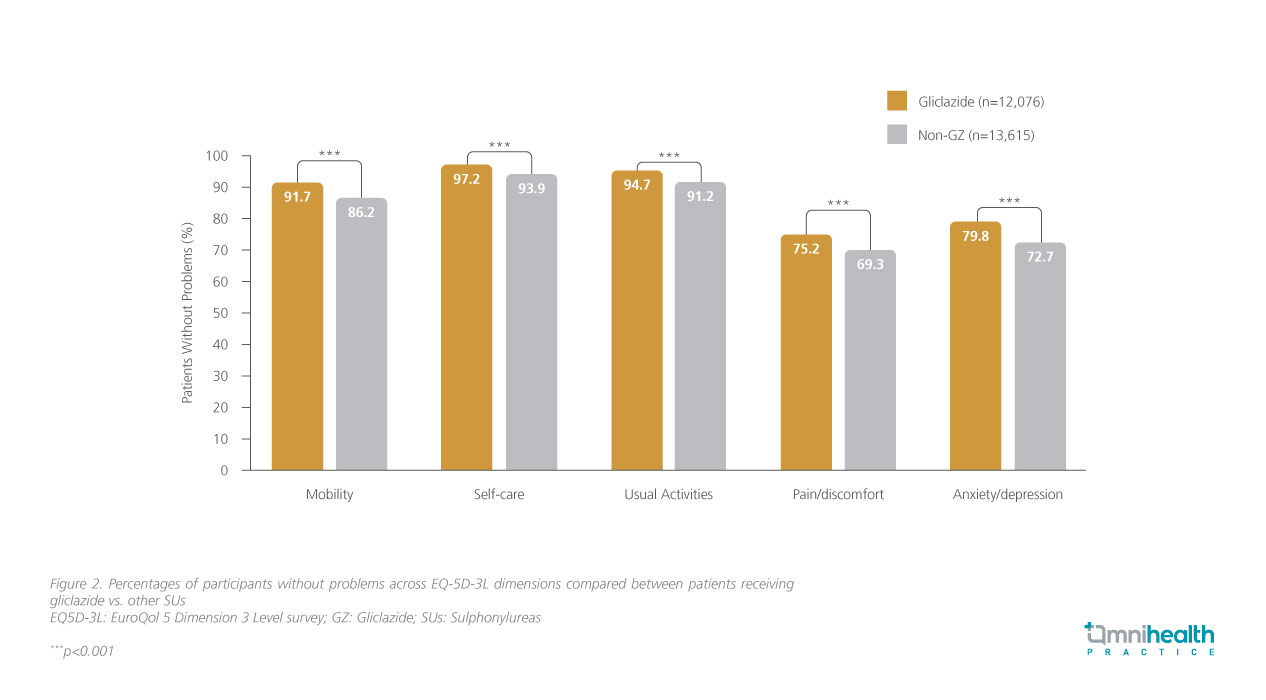
Among those treated with OGLDs, 60% (n=25,693) received sulphonylureas (SUs), of whom 47% (n=12,078) had received gliclazide. Compared to non-SU users, SU users had lower index scores (0.889 vs. 0.907; p<0.001) with a lower proportion having a high EQ-5D-3L score (58.7% vs. 63.4%; p<0.001).12 However, among the users of SUs, more patients treated with gliclazide reported “no problem” in all dimensions (p<0.001) than non-gliclazide users (figure 2).12 Despite their older age and higher prevalence of cardiovascular and renal comorbidities, gliclazide users had higher index scores (0.903 vs. 0.877; p<0.001) and were more likely to have high EQ-5D-3L score (62.9% vs. 55.0%; p<0.001) than non-gliclazide users.12 This difference was attributed to their better control of HbA1c, lipid and blood pressure without an increased risk of hypoglycemia.12,13
Conclusion
The patient demographic of T2D is shifting towards a younger population associated with long disease duration, high lifetime risk of comorbidities and decrements in HRQoL.4-7 Prof. Chan concluded that 20% of Asian patients with T2D treated with OGLDs experienced some problems, notably with anxiety, depression, pain, or discomfort. As such, the implementation of patient-centered approaches with patient empowerment is an important strategy to optimize treatment outcomes and HRQoL.8-10 Aside from LSMs, the choices of OGLDs could also influence HRQoL with gliclazide-treated patients having better HRQoL than other users of SUs.12 Taken together, this real-world evidence supports the safety, effectiveness and tolerability of gliclazide as a preferred OGLD among Asian patients with T2D.

